Abstract
We investigated which of the three FRAX fracture risk assessment tool models is most applicable to Korean women. For 306 postmenopausal women (mean age, 77 yr) with a hip fracture, fracture probabilities were calculated using FRAX models from Japan, Turkey and China. Data on bone mineral density (BMD) at the femoral neck were available for 103 patients. Significant differences existed among the models, independent of the inclusion of BMD in the calculation of fracture probabilities. The probabilities of both major osteoporotic fractures and hip fractures were significantly higher in the Japanese model than in the Turkish or Chinese models. In all of the models, the probabilities of a major osteoporotic fracture, but not of a hip fracture, decreased significantly if calculated without BMD values. By applying the Japanese model, the ten-year probabilities for major osteoporotic and hip fractures increased significantly with age. Our results suggest that the Japanese FRAX model might be the most appropriate for Korean women.
Fractures related to osteoporosis are a major health issue and produce a significant economic and social burden in Asian countries, as well as in Western countries. Hip fractures result in higher cost, disability, and mortality than do other osteoporotic fractures, showing 11.3-17.1% of one-year mortality rate in Korea (1-3). In addition, approximately 25% of women require long-term care after a hip fracture, and 50% will have some long-term loss of mobility (1, 4). Early recognition and management of individuals who may be susceptible to fractures provides a substantial benefit by reducing the burden of fractures.
Osteoporosis, as defined on the basis of bone mineral density (BMD), is a major risk factor for fractures, and hip BMD best predicts fracture risk in the hip (5). However, 36% of women with a hip fracture have a T-score > -2.5 (6). A number of clinical risk factors that predispose a person to fractures other than BMD have been identified in various populations (7). The integration of these factors could be used to estimate the absolute risk of fractures and to determine the threshold of the risk for the intervention, which may result in cost savings. FRAX, a fracture risk assessment tool, is a computer-based algorithm sponsored by the World Health Organization. Using easily obtainable clinical risk factors in addition to femoral neck BMD, FRAX provides models for assessing the ten-year probability of a major osteoporotic fracture (hip, clinical spine, humerus or wrist fracture) and a hip fracture, helping to identify high-risk candidates for intervention (8, 9).
In addition to the clinical risk factors, fracture probability varies markedly in different regions of the world (10). FRAX models need to be calibrated to those countries where the epidemiology of fractures and death is known (11). Currently, FRAX models are available for 18 different countries through the web page (http://www.shef.ac.uk/FRAX), but few other countries have sufficient data to construct their own FRAX models. Although a surrogate country is recommended in the absence of a FRAX model for a specific country (11), the model that is most appropriate for Korean women has never been determined. This study was conducted to determine the most suitable FRAX model for the assessment of fracture risk in Korean women.
Postmenopausal women who were admitted to Samsung Medical Center with a proximal femoral fracture between March 2005 and September 2009 were enrolled in this study. Women were considered postmenopausal if the amenorrhea duration was ≥12 months or if the serum follicle-stimulating hormone level was >40 IU/L. Only women with a complete set of data for estimating fracture risk were included, and women with polytrauma or in a comatous condition were excluded.
The following clinical risk factors required for FRAX were obtained from the patients' medical records and telephone interviews: age, body mass index, a prior fragility fracture, a parental history of a hip fracture, smoking history, history of long-term oral glucocorticoid use, rheumatoid arthritis, daily alcohol consumption of three or more units daily, and other causes of secondary osteoporosis. The BMD (expressed as g/cm2) was determined at the femoral neck by dual-energy X-ray absorptiometry (Delphi W, Hologic Inc., Bedford, MA, USA). Only BMD determined within six months of a fracture was included in the investigation. The in vivo coefficient of variation using our densitometer was 1.4% for the hip. For the evaluation of fracture probabilities, three FRAX models developed in Japan, Turkey, and China were chosen.
Data are presented as the mean±standard deviation (SD) or number (percent). Fisher's exact test was used to compare frequencies. A paired t test or Mann-Whitney test was used to analyze differences according to inclusion of BMD values. The differences among the three models were tested using the Kruskal-Wallis test or one-way analysis of variance (ANOVA). A P<0.05 was considered statistically significant. All statistical calculations were performed with PASW Statistics 17 (SPSS Inc., Chicago, IL, USA).
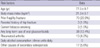
Three hundred six women between the ages of 48 and 101 yr were enrolled in this study. The clinical risk factors for fracture are presented in Table 1. Data on the BMD at the femoral neck were available in 103 women (33.7%) and were calculated to be 0.482±0.094 g/cm2 with a T-score of -3.12±0.81.
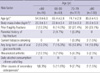
The ten-year probabilities of major osteoporotic fractures and hip fractures using the three different models are shown in Table 2, which shows that significant differences were found among the models. The ten-year probabilities of both major osteoporotic and hip fractures were significantly higher with the Japanese model including BMD data (mean 25.0% and 10.4%, respectively) than with the Turkish (2.6% and 1.2%) or Chinese model (4.8% and 2.2%). In all of the models, ten-year probabilities calculated excluding BMD values were significantly lower for major osteoporotic fractures, but not for hip fractures. The differences among models, however, remained significant.
Table 3 shows the clinical risk factors according to age. Body mass index decreased with age, and the causes of secondary osteoporosis other than rheumatoid arthritis, smoking, glucocorticoid use or alcohol intake had different distributions among the groups. In addition, the BMD and T-score gradually decreased with increasing age (Table 4).
Fig. 1 illustrates the fracture probabilities in the Japanese FRAX model according to age. The fracture probabilities of both major osteoporotic fractures and hip fractures significantly increased with age, regardless of the addition of BMD for the estimation of risks. In addition, the fracture probabilities of both major osteoporotic fractures and hip fractures calculated excluding BMD values were significantly lower than those calculated with BMD values for all the age groups, except for the age group ≥80 yr.
This study was performed to determine the most applicable FRAX model for evaluating fracture risk in Korean women. It appears that the Japanese model may be the most adequate surrogate model for Korean women.
For constructing FRAX models in each country, reliable epidemiologic studies on the risk factors and fracture occurrences in the general population are necessary because fracture risk varies according to geographic region. Since there are currently only a limited number of FRAX models worldwide, most countries use a pre-existing model from a surrogate country. Because Korea and Turkey belong to the same risk group for hip fracture, Kanis et al. (11) suggested that Koreans adopt the low-risk group model developed in Turkey. Both Japan and China are categorized as moderate-risk, but these countries are very close to Korea both geographically and genetically. In the current study, we therefore tested the three FRAX models from Turkey, Japan and China.
The probabilities of both major osteoporotic fractures and hip fractures using the Japanese model were five- to ten-fold higher than those using the Turkish or Chinese model, regardless of BMD data inclusion. Because only women with a hip fracture were included in the present study, higher probability by FRAX is believed to better reflect the real risk of fracture. In addition, the probabilities in the Japanese model escalated as age increased, equivalent to the actual exponential increase in fracture risk with age (12). Together, these findings suggest that the Japanese model could be a better surrogate.
In contrast to major osteoporotic fracture, the overall probability of hip fracture did not change with inclusion of BMD data in the Japanese model. However, when analyzed further by age, the probabilities of hip as well as major osteoporotic fracture in women less than 80 yr old became higher when the BMD results were included. These findings are consistent with those of a recent study that showed that the effect of BMD on fracture probabilities decreases in very old woman (13). The discrepancy between major osteoporotic fractures and hip fractures in our study might also be explained, at least in part, by the limited statistical power, because BMD data were only available for one-third of the subjects.
This is the first study to evaluate the application of various surrogate FRAX models in Korean women. In contrast to the recommendation by Kanis et al. (11), the Japanese model was more appropriate for Korean women than was the Turkish model. Furthermore, including women who had already sustained a hip fracture in the assessment provided a better examination of which model could better predict fracture probabilities in Korean women.
There were some limitations to the current study. First, subjects were recruited from a tertiary care center, so the distribution of clinical risk factors might not represent that of the general Korean population. Second, the subjects were elderly (mean age, 77 yr), and most subjects (77.7%) had osteoporosis, as determined by BMD. Thus, younger non-osteoporotic women should have been included in the study. Finally, although we could choose the Japanese model as the surrogate FRAX model in Korean women, the clinical implications of this application are still limited. To identify the threshold of fracture probability required for osteoporosis treatment, a country-specific cost-effectiveness analysis should be performed.
In conclusion, our results indicate that Japan's FRAX model is a suitable surrogate model for Korean women. A study with a larger general population is needed to confirm our conclusion.
Figures and Tables
Fig. 1
Ten-year fracture probabilities using Japan FRAX model according to age. (A) Major osteoporotic fracture, (B) Hip fracture. The 10-yr probabilities increase significantly according to age for both major osteoporotic fractures and hip fractures (P<0.001 by ANOVA).
*P<0.05 vs inclusion of BMD by Mann-Whitney or t test, as indicated.

References
1. Moon YW, Yoon BK, Min YK, Chang MJ, Jung SM, Lim SJ, Park YS. Mortality, second fracture, and functional recovery after hip fracture surgery in elderly Koreans. Korean J Bone Metab. 2008. 15:41–47.
2. Lee SR, Kim SR, Chung KH, Ko DO, Cho SH, Ha YC, Kim BG, Kim JR, Kim SY. Mortality and activity after hip fracture: a prospective study. J Korean Orthop Assoc. 2005. 40:423–427.

3. Kho DH, Kim KH, Shin JY, Lee JH, Kim DH. Postoperative mortality rate of hip fracture in elderly patients. J Korean Fract Soc. 2006. 19:117–121.

4. North American Menopause Society. Management of osteoporosis in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010. 17:25–54.
5. Fink HA, Harrison SL, Taylor BC, Cummings SR, Schousboe JT, Kuskowski MA, Stone KL, Ensrud KE. Study of Osteoporotic Fractures (SOF) Group. Differences in site-specific fracture risk among older women with discordant results for osteoporosis at hip and spine: study of osteoporotic fractures. J Clin Densitom. 2008. 11:250–259.

6. Schuit SC, van der Klift M, Weel AE, de Laet CE, Burger H, Seeman E, Hofman A, Uitterlinden AG, van Leeuwen JP, Pols HA. Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone. 2004. 34:195–202.

7. Kanis JA, Borgstrom F, De Laet C, Johansson H, Johnell O, Jonsson B, Oden A, Zethraeus N, Pfleger B, Khaltaev N. Assessment of fracture risk. Osteoporos Int. 2005. 16:581–589.

8. Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX™ and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008. 19:385–397.

9. Kanis JA. on behalf of the World Health Organization Scientific Group. Assessment of osteoporosis at the primary health-care level. Technical report. 2008. University of Sheffield, UK: WHO Collaborating Centre.
10. Kanis JA, Johnell O, De Laet C, Jonsson B, Oden A, Ogelsby AK. International variations in hip fracture probabilities: implications for risk assessment. J Bone Miner Res. 2002. 17:1237–1244.

11. Kanis JA, Oden A, Johansson H, Borgstrom F, Strom O, McCloskey E. FRAX and its applications to clinical practice. Bone. 2009. 44:734–743.

12. Siris ES, Brenneman SK, Barrett-Connor E, Miller PD, Sajjan S, Berger ML, Chen YT. The effect of age and bone mineral density on the absolute, excess, and relative risk of fracture in postmenopausal women aged 50-99: results from the National Osteoporosis Risk Assessment (NORA). Osteoporos Int. 2006. 17:565–574.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download