Abstract
We report on an exceptional vascular cause of gastrointestinal hemorrhage. A 30-yr-old man was admitted because of recurrent hematochezia. Colonoscopy showed circumferential, erythematous, and nodular vascular distensions with hematocystic spots in the terminal ileum resembling varicosis and subsequent computed tomography with 3-dimensional angiographic reconstruction revealed a vascular architecture around the terminal ileum. No other potential source of bleeding was identified. The patient was treated by ileocecectomy and the final diagnosis was of an arteriovenous malformation confined to the terminal ileum. He has been followed-up without a further hemorrhagic episode.
Vascular lesions of the small intestine and colon are common causes of acute or chronic gastrointestinal hemorrhage, and arteriovenous malformations (AVMs) are an important vascular cause of obscure and intermittent gastrointestinal bleeding (1). Histologically, AVMs are persistent communications between thick-walled arteries and veins without intervening capillaries and are divided into true or congenital and acquired forms according to their locations and age at their presentations. Although the endoscopic appearances of AVMs occurring in gastrointestinal tracts are not distinctive, some reported cases were observed as flat or mildly elevated hemorrhagic spots or erosions, while others have been appeared as polypoid masses. AVMs are usually small, single, and are located mainly in the rectum and descending colon in case of congenital or true AVMs, unlike acquired AVMs which are located mainly within the right colon. AVMs are relatively uncommon in the small bowel, and it is extremely rare that they present as a circumferential, transmural, and dilated vascular structure encasing only the terminal ileum and mimicking intestinal varicosis.
We report a rare case in which a transmural AVM mimicking intestinal varicosis and encasing the terminal ileum circumferentially. The lesion was successfully treated by surgical resection.
A 30-yr-old man was transferred to our hospital for the investigation and management of intermittent hematochezia for a 5-yr duration. On admission, the patient was severely anemic (Hb 7.2 g/dL). He was not being prescribed a nonsteroidal anti-inflammatory drug, nor was suffering from portal hypertension or liver disease. There was no history of a peptic ulcer, and examinations of skin, oral, and anal mucosa revealed no abnormal findings. His liver function test was normal.
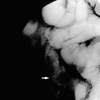
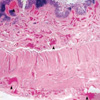
An urgent upper endoscopy was performed and yielded a result within normal limits. Subsequent colonoscopy revealed a circumferential erythematous, nodular, and elevated lesion with hematocystic spots in the terminal ileum resembling varicosis (Fig. 1). Computed tomography (CT) scans with 3-dimensional angiographic reconstruction showed a vascular tuft located around the terminal ileum (Fig. 2). To exclude other synchronous intraluminal sources of bleeding in the small bowel we performed enteroclysis, which revealed a segmental, nodular, and uneven elevated lesion with a length of 10 cm in the terminal ileum (Fig. 3). No further lesion was found to be suspected as being another bleeding source. The patient was treated by ileocecectomy, which encompassed the nodular and dilated vascular structure in the terminal ileum that resembled a varicosis lesion on gross inspection (Fig. 4). Surgical biopsy specimens revealed dilated vascular channels with a thickened wall involving the entire bowel wall and secondary arterialization of veins consistent with an AVM (Fig. 5). His postoperative course was uneventful, and the patient has been followed-up without a further episode of hemorrhage.
Despite dramatic improvements in diagnostic and therapeutic modalities, it is not always possible to determine the appropriate diagnosis and treatment for vascular lesions, such as, vascular ectasia, hemangiomas, Dieulafoy lesions, and AVMs. In particular in the case of AVMs, no distinctive endoscopic or radiologic appearance has been elucidated because of their rarity, terminologic inconsistencies, and the diverse natures of their endoscopic morphologies. The presented case describes an unusual AVM that involved the full thickness of the terminal ileum, mimicking intestinal varicosis on endoscopic and gross inspection. Endoscopic finding of our case which demonstrates dilated and tortuously distended vascular tufts with red markings is a typical feature of intestinal varicosis (2, 3). The majority of AVMs reported are focal, flat, or mildly elevated with erythematous spots or erosions, and a minority of AVMs have polypoid or pedunculated masses (4-6). A MEDLINE search revealed that only a small proportion of AVMs mimic intestinal varicosis with transmural involvement of the small and/or large bowel, and no endoscopic pictures were provided (7-9). We found only one case of an AVM with complete endoscopic pictures and gross pictures of dilated, tortuous, vascular tufts similar to our case. It involved the entire colon without displaying a vascular texture by angiography (10).
Although AVMs can occur in jejunum (11), the most common sites of involvement of true congenital AVMs are the rectum or sigmoid colon. Many reports have suggested that they are most common in the cecum and ascending colon, but the terminologic confusion concerning the differentiation of angiodysplasia and acquired AVMs, which mainly develop in right colon, from congenital AVMs may have influenced the results. True AVMs are developmental and mainly occur in the rectum or sigmoid colon of patients younger than 50 yr, and correspond to type 2 lesions according to Moore's classification (12). Acquired AVMs or angiodysplasia correspond to type 1 according to this classification and occur in patients older than 50 yr. AVMs in younger patients tend to occur at atypical sites such as in the small bowel, but no segmental form of AVM has been previously reported to involve only the terminal ileum in a cylindrical manner.
The usefulness of CT for the detection of sources of gastrointestinal bleeding has been recently described in the context of imaging modality developments (13). In the present case, we performed CT with a 3-dimensional angiographic reconstruction instead of conventional mesenteric arterial angiography because we did not consider invasive radiological therapeutic intervention as a potential elective hemostatic modality, and because we required an evaluation of the relation between the vascular architecture and the bowel wall. In addition, our case would not have been suitable for endoscopic therapeutic options. Ultimately, surgical resection offers the best chance of curative treatment in such situations.
In conclusion, we experienced a rare case of a segmental transmural AVM involving the terminal ileum and mimicking intestinal varicosis, which presented as a case of recurrent lower gastrointestinal hemorrhage, and which was successfully treated by surgical resection.
Figures and Tables
Fig. 1
Colonoscopic view of the arteriovenous malformation. This image shows circumferential, erythematous, tortuous vascular distensions with hematocystic spots in the terminal ileum, resembling the varices seen in the esophagus of patients with portal hypertension.
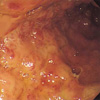
Fig. 2
Computed tomography (CT) scan finding with 3-dimensional angiographic reconstruction. The high-density architecture encasing the terminal ileum was identified on arterial phase CT (A) with delayed enhancement on venous phase. This three-dimensional angiographic reconstruction reveals a vascular tuft with a long draining vein in the right lower quadrant area (B). Arrow, arteriovenous malformation.
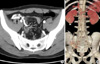
Fig. 3
Finding of enteroclysis revealed a segmental, nodular, and uneven elevated lesion with a length of 10 cm in the terminal ileum, with no other obvious source of hemorrhage in the remaining small bowel (arrow).
References
1. Meyer CT, Troncale FJ, Galloway S, Sheahan DG. Arteriovenous malformations of the bowel: an analysis of 22 cases and a review of the literature. Medicine (Baltimore). 1981. 60:36–48.
2. Tang SJ, Zanati S, Dubcenco E, Cirocco M, Christodoulou D, Kandel G, Haber GB, Kortan P, Marcon NE. Diagnosis of small-bowel varices by capsule endoscopy. Gastrointest Endosc. 2004. 60:129–135.

3. Tang SJ, Jutabha R, Jensen DM. Push enteroscopy for recurrent gastrointestinal hemorrhage due to jejunal anastomotic varices: a case report and review of the literature. Endoscopy. 2002. 34:735–737.

4. Chung YW, Jeon YC, Paik CH, Kim JP, Han DS, Sohn JH, Oh YH, Park YW, Hahm JS. Pedunculated angiodysplasia of the colon treated with endoscopic resection: a case report. Dig Dis Sci. 2005. 50:1550–1552.

5. Nasseri-Moghaddam S, Mohamadnejad M, Malekzadeh R, Tavangar SM. Images of interest. Gastrointestinal: polypoid arteriovenous malformation of the colon. J Gastroenterol Hepatol. 2004. 19:1419.
6. Maeng L, Choi KY, Lee A, Kang CS, Kim KM. Polypoid arteriovenous malformation of colon mimicking inflammatory fibroid polyp. J Gastroenterol. 2004. 39:575–578.

7. Ichikawa T, Koyama A, Fujimoto H, Honma M, Saiga T, Matsubara N, Ozeki Y, Uchiyama G, Ohtomo K. Diffuse arteriovenous malformation involving jejunum and total colon with mesenteric varices. Clin Imaging. 1994. 18:221–223.

8. Defreyne L, Meersschaut V, van Damme S, Berrevoet F, Robberecht E, Praet M. Colonic arteriovenous malformation in a child misinterpreted as an idiopathic colonic varicosis on angiography: remarks on current classification of childhood intestinal vascular malformations. Eur Radiol. 2003. 13:Suppl 4. L138–L141.

9. Steffani KD, Eisenberger CF, Gocht A, Izbicki JR, Yekebas EF. Recurrent intestinal bleeding in a patient with arterio-venous fistulas in the small bowel, limited mesenteric varicosis without portal hypertension and malrotation type I. Z Gastroenterol. 2003. 41:587–590.

10. Haringsma J, Tytgat GN. Chronic intestinal bleeding caused by congenital arteriovenous malformations. Endoscopy. 1988. 20:330–331.

11. Park KH, Kim YI, Yoo YO, Park SH, Lee HI, Joo DH, Kim HG, Sung NK. A case of bleeding vascular malformation of the jejunum. J Korean Surg Soc. 1998. 54:748–751.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download