Abstract
Triple therapy with bismuth subsalicylate, amoxicillin, metronidazole (BAM) or with omeprazole, amoxicillin, clarithromycin (OAC) has been commonly used for the eradication of Helicobacter pylori infection. We compared the efficacy of these triple therapies in children with H. pylori infection. We retrospectively analyzed results in 233 children with H. pylori infection and treated with OAC (n=141) or BAM (n=92). Overall eradication rates of triple therapy with OAC and BAM were 74% and 85%, respectively, which showed no statistical difference. Our study showed that the triple therapy with BAM was more effective for the first-line eradication of H. pylori infection in Korean children, but has no statistical difference with OAC regimen.
Helicobacter pylori (H. pylori) is a spiral-shaped, Gram-negative bacillus first isolated in 1983 (1). H. pylori is the major pathogen of chronic gastritis and peptic ulcer disease and is strongly associated with gastric adenocarcinoma and lymphoma (2, 3). Triple therapy with two antibiotics and a proton pump inhibitor (PPI) has been recommended as the treatment of choice for H. pylori infection (4, 5), producing an eradication rate of 70-80% in adults, but there have been few large-scale trials of the efficacy of PPI-based triple eradication therapy in children. In addition, H. pylori has shown antimicrobial resistance, which may be the cause of treatment failure in many patients (6-8). The aim of this study was to compare the efficacy in pediatric patients of two triple eradication therapies commonly used in Korea.
This is a retrospective study of 233 pediatric patients with H. pylori infection at two tertiary general hospitals (Asan Medical Center and Samsung Medical Center) between January 1999 and July 2004. Patients were excluded if they had undergone previous treatment for H. pylori or if they had taken any antibiotics or PPI in the 4 weeks prior to the study. Esophagogastroduodenoscopy was performed in each patient prior to treatment since all patients had suffered from dyspepsia or upper abdominal pain suggestive of an organic disease. H. pylori infection was diagnosed when both histology and a rapid urease test showed positive result.
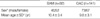
While 141 of 233 children were initially treated with an OAC regimen, and 92 of 233 children were initially treated with a BAM regimen. Details of regimens were described in Table 1.
Efficacy was evaluated 12 weeks after the end of treatment using a 13C-urea breath test (UBT), performed according to a previously validated technique. Briefly, after a fasting baseline sample breath collection, 13C-labelled urea was administered orally in water, and a second breath sample was collected 20 min later. Breath samples were analyzed by isotope ratio mass spectrometry (UBiT-IR300; Photal Otsuka Electronics, Japan) and 2.5 δ ‰ (subtraction of baseline from sample) was used as the cut-off value.
The 233 children consisted of 115 males and 118 females and mean age was 10 yr (ranged from 2 to 15 yr). There were no demographic differences between the children treated with the OAC and BAM regimens (Table 1).
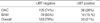
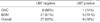
Of the 141 children treated with the OAC regimen, 105 were UBT negative after treatment. Of the 36 children who failed the OAC regimen, 26 were secondarily treated with the BAM regimen, of whom 21 became UBT negative.
Of the 92 children treated with the BAM regimen, 78 were UBT negative after treatment. Of the 14 children who failed the BAM regimen, 7 were secondarily treated with the OAC regimen, of whom 6 became UBT negative (Fig. 1).
As the first-line therapies, the eradication rates of the OAC and BAM regimens were 74% and 85%, respectively, and the overall eradication rate of both first-line triple regimens was 79% (Table 2). Although the BAM regimen was more effective than the OAC regimen in eradicating H. pylori infection, the difference did not reach statistical significance (p=0.07). As the second-line therapies, the eradication rates of the OAC and BAM regimens were 86% and 81%, respectively, and the overall eradication rate of both second-line triple regimens was 82% (Table 3). Again, the difference between the two regimens was not statistically significant (p=0.53). After the second-line treatment, as both first and second-line the overall eradication rate of the OAC and BAM regimens was 90% (210/233).
The previous studies of H. pylori eradication according to antibiotic regimens were rare in Korean children. Bae et al. (9) reported 90% with BAM regimen in 1998, Choi et al. (10) reported 82% with OAC regimen in 2002. Both results were better than our results, which may reflect the increasing rate of antibiotic resistance with time, although we did not directly test the H. pylori sensitivity to antibiotics in this population. Bae et al. (9) also reported that triple therapy with BAM regimen was more effective and safe than dual therapy with bismuth subcitrate and amoxicillin, eradication rate was 90% in group treated with triple regimen, 61% in group treated with dual regimen. However there have been no reports on the comparison of eradication rate of between BAM and OAC regimen in Korean children.
For effective treatment regimens, the treatment should achieve an eradication rate of over 80% on a rigorous intention to treat basis and over 90% on a per protocol basis (11-13). This result may imply per protocol analysis because we enrolled retrospectively the only children who completed the prescribed regimen and followed up; therefore there needs a better regimen to eradicate H. pylori in children more effectively.
Result of susceptibility testing yields best treatment outcome, however susceptibility testing is generally unavailable. Therefore, study of antibiotic susceptibility in Korean children infected with H. pylori will be necessary.
Clarithromycin and metronidazole are important key antibiotics in the treatment of H. pylori infection especially in children, so increasing resistance to both antibiotics has become a major problem in eradication, including in children (6-8, 14, 15). In Korean children, the resistance rate of H. pylori to clarithromycin was 19% in 2000 (16) and that in our unpublished personal data in 2005 was 33% (unpublished personal data in 9 children). These results suggest that the rate of clarithromycin is increasing in Korean children. Those in Korean adult also showed increasing rate of resistance from 7.1% in 1999 to 13.8% in 2003 (17). For example, of children infected with H. pylori, the rate of resistance to clarithromycin has been reported to range from 12.4% to 23.5% in Europe, from 10.6% to 25% in North America, and from 5.4% to 17% in East Asia (8).
The essential risk factor for clarithromycin resistance is previous consumption of macrolides (18-20). Macrolides, which include clarithromycin, azithromycin, and erythromycin, have been used in Korea since the early 1990s to treat children with respiratory tract infections, enterocolitis, otitis media, and chronic sinusitis. During macrolides treatment, H. pylori colonizing the stomach of a child may become resistant to clarithromycin, leading to high rates of primary clarithromycin resistance (21).
Metronidazole has been used as a primary antimicrobial agent to treat H. pylori infection because it is actively secreted in the saliva and gastric juice, becoming highly concentrated in the stomach. In Europe and the U.S.A., the prevalence of H. pylori resistance to metronidazole has been found to vary from 20% to 40% (22-24), and its prevalence is much higher in developing countries (50-80%) (25). In contrast, H. pylori resistance to metronidazole is quite low in Japan (9-12%) (26). In Korean adult, H. pylori resistance to metronidazole has increased from 52.9% in 1987 to 66.2% in 2003 (17). In Korean children in our unpublished personal data in 2005 was 44% (unpublished personal data in 9 children).
Recently, doubly resistant strains have been reported worldwide, but their prevalence is still low in Europe (0.8-9.1%) and Asia (2-3%) (27, 28). In our study, 6 children failed treatment with both the OAC and BAM regimens, suggesting that they may harbor multi-drug resistant strains of H. pylori and in our unpublished data 33% children showed resistance to both clarithromycin and metronidazole.
We changed OAC as first-line treatment since 2001, because NASPGHN (North American Society for Pediatric Gastroenterology, Hepatology and Nutrition) (5) recommended bismuth compound as second-line treatment because of the availability and clinician's reluctance to use bismuth compound, however BAM regimen showed superior eradication rate to OAC regimen.
In some studies, poor compliance has been a major risk factor for failure to eradicate H. pylori infection (29). In our study, the compliance was not investigated, so we could not estimate the compliance issue.
Our study had several limitations. Firstly, we could not evaluate compliance and eradication rate to intention to treat and per protocol since it was not a randomized controlled study, although we found no demographic differences between children treated with the two triple regimens. Secondly we do not have antibiotic susceptibility testing data, which might have given more detailed information.
In conclusion, we have compared the efficacy of a metronidazole-based regimen and a clarithromycin-based regimen in a large population of children infected with H. pylori. Our study showed that the triple therapy with BAM was more effective for the first-line eradication of H. pylori infection in Korean children, but has no statistical difference with OAC regimen.
Figures and Tables
Fig. 1
Treatment strategies and outcomes of the study population. OAC, omeprazole+amoxicillin+clarithromycin; BAM, bismuth subsalicylate+amoxicillin+metronidazole; UBT, urea breath test.

References
1. Warren JR, Marshall BJ. Unidentified curved bacilli on gastric epithleium in active chronic gastritis. Lancet. 1983. 1:1273–1275.
2. Kim KM, Oh YL, Ko JS, Choe YH, Seo JK. Histopathology and expression of Ki-67 and cyclooxygenase-2 in childhood Helicobacter pylori gastritis. J Gastroenterol. 2004. 39:231–237.

3. Kim KM, Oh YL, Seo JK. Analysis of genes of Helicobacter pylori and relationship to histopathology, cyclooxygenase-2, and Ki-67 expression in Korean children. Helicobacter. 2004. 9:550(A).
4. Malfertheiner P, Megraud F, O'Morain C, Hungin AP, Jones R, Axon A, Graham DY, Tytgat G. Current concepts in the management of Helicobacter pylori infection--the Maastricht 2-2000 Consensus Report. Aliment Pharmacol Ther. 2002. 16:167–180.

5. Gold BD, Colletti RB, Abbott M, Czinn SJ, Elitsur Y, Hassall E, Macarthur C, Snyder J, Sherman PM. Helicobacter pylori infection in children: recommendations for diagnosis and treatment. J Pediatr Gastroenterol Nutr. 2000. 31:490–497.

6. Kalach N, Bergeret M, Benhamou PH, Dupont C, Raymond J. High levels of resistance to metronidazole and clarithromycin in Helicobacter pylori strains in children. J Clin Microbiol. 2001. 39:394–397.

7. Crone J, Granditsch G, Huber WD, Binder C, Innerhofer A, Amann G, Hirschl AM. Helicobacter pylori in children and adolescents: increase of primary clarithromycin resistance, 1997-2000. J Pediatr Gastroenterol Nutr. 2003. 36:368–371.

8. Megraud F. H pylori antibiotic resistance: prevalence, importance, and advances in testing. Gut. 2004. 53:1374–1384.

9. Bae SH, Koh JS, Seo JK. Therapeutic efficacy of dual therapy and triple therapy for Helicobacter pylori infection in children. J Korean Pediatr Soc. 1997. 41.
10. Choi IK, Lee SY, Chung KS. Effect of one- or two-week triple therapy with omeprazole, amoxicillin, and clarithromycin on eradication of Helicobacter pylori infection in children. Korean J Pediatr Gastroenterol Nutr. 2002. 5:19–25.

11. Current European concepts in the management of Helicobacter pylori infection. The Maastricht Consensus Report. European Helicobacter pylori Study Group [published erratum appears in Gut 1997 Aug; 41(2): 276]. Gut. 1997. 41:8–13.
12. Lam SK, Talley NJ. Report of the 1997 Asia Pacific Consensus Conference on the management of Helicobacter pylori infection. J Gastroenterol Hepatol. 1998. 13:1–12.

13. NIH Consensus Conference. Helicobacter pylori in peptic ulcer disease. NIH Consensus Development Panel on Helicobacter pylori in Peptic Ulcer Disease. JAMA. 1994. 272:65–69.
14. Rerksuppaphol S, Hardikar W, Midolo PD, Ward P. Antimicrobial resistance in Helicobacter pylori isolates from children. J Paediatr Child Health. 2003. 39:332–335.

15. Duck WM, Sobel J, Pruckler JM, Song Q, Swerdlow D, Friedman C, Sulka A, Swaminathan B, Taylor T, Hoekstra M, Griffin P, Smoot D, Peek R, Metz DC, Bloom PB, Goldschmidt S, Parsonnet J, Triadafilopoulos G, Perez-Perez GI, Vakil N, Ernst P, Czinn S, Dunne D, Gold BD. Antimicrobial resistance incidence and risk factors among Helicobacter pylori-infected persons, United States. Emerg Infect Dis. 2004. 10:1088–1094.
16. Ko JS, Yang HR, Seo JK. Detection of 23S rRNA mutation associated with clarithromycin resistance in children with Helicobacter pylori infection. Korean J Pediatr Gastroenteril Nutr. 2004. 7:137–142.

17. Kim JM, Kim JS, Jung HC, Kim N, Kim YJ, Song IS. Distribution of antibiotic MICs for Helicobacter pylori strains over a 16-year period in patients from Seoul, South Korea. Antimicrob Agents Chemother. 2004. 48:4843–4847.

18. Cabrita J, Oleastro M, Matos R, Manhente A, Cabral J, Barros R, Lopes AI, Ramalho P, Neves BC, Guerreiro AS. Features and trends in Helicobacter pylori antibiotic resistance in Lisbon area, Portugal (1990-1999). J Antimicrob Chemother. 2000. 46:1029–1031.

19. Goh KL. Update on the management of Helicobacter pylori infection, including drug-resistant organisms. J Gastroenterol Hepatol. 2002. 17:482–487.

20. Czinn SJ. Helicobacter pylori infection: detection, investigation, and management. J Pediatr. 2005. 146:Suppl 3. S21–S26.

21. Taneike I, Goshi S, Tamura Y, Wakisaka-Saito N, Matsumori N, Yanase A, Shimizu T, Yamashiro Y, Toyoda S, Yamamoto T. Emergence of clarithromycin-resistant Helicobacter pylori (CRHP) with a high prevalence in children compared with their parents. Helicobacter. 2002. 7:297–305.

22. Debets-Ossenkopp YJ, Herscheid AJ, Pot RG, Kuipers EJ, Kusters JG, Vandenbroucke-Grauls CM. Prevalence of Helicobacter pylori resistance to metronidazole, clarithromycin, amoxycillin, tetracycline and trovafloxacin in The Netherlands. J Antimicrob Chemother. 1999. 43:511–515.

23. Parsons HK, Carter MJ, Sanders DS, Winstanley T, Lobo AJ. Helicobacter pylori antimicrobial resistance in the United Kingdom: the effect of age, sex and socio-economic status. Aliment Pharmacol Ther. 2001. 15:1473–1478.

24. Osato MS, Reddy R, Reddy SG, Penland RL, Malaty HM, Graham DY. Pattern of primary resistance of Helicobacter pylori to metronidazole or clarithromycin in the United States. Arch Intern Med. 2001. 161:1217–1220.

25. Torres J, Camorlinga-Ponce M, Perez-Perez G, Madrazo-De la Garza A, Dehesa M, Gonzalez-Valencia G, Munoz O. Increasing multidrug resistance in Helicobacter pylori strains isolated from children and adults in Mexico. J Clin Microbiol. 2001. 39:2677–2680.

26. Kato M, Yamaoka Y, Kim JJ, Reddy R, Asaka M, Kashima K, Osato MS, El-Zaatari FA, Graham DY, Kwon DH. Regional differences in metronidazole resistance and increasing clarithromycin resistance among Helicobacter pylori isolates from Japan. Antimicrob Agents Chemother. 2000. 44:2214–2216.

27. Ellenrieder V, Boeck W, Richter C, Marre R, Adler G, Glasbrenner B. Prevalence of resistance to clarithromycin and its clinical impact on the efficacy of Helicobacter pylori eradication. Scand J Gastroenterol. 1999. 34:750–756.
28. Isomoto H, Inoue K, Furusu H, Enjoji A, Fujimoto C, Yamakawa M, Hirakata Y, Omagari K, Mizuta Y, Murase K, Shimada S, Murata I, Kohno S. High-dose rabeprazole-amoxicillin versus rabeprazole-amoxicillin-metronidazole as second-line treatment after failure of the Japanese standard regimen for Helicobacter pylori infection. Aliment Pharmacol Ther. 2003. 18:101–107.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download