Abstract
The purpose of this prospective study was to evaluate the efficacy and safety of adefovir dipivoxil with or without ongoing lamivudine in decompensated lamivudine-resistant chronic hepatitis B patients. Forty-six hepatitis B e antigen (HBeAg)-positive patients with decompensated liver function and lamivudine-resistant hepatitis B virus (HBV) were assigned to adefovir dipivoxil monotherapy (n=18) or combination therapy with ongoing lamivudine (n=28) according to their own preference. After 24 weeks of treatment, 83% of monotherapy and 86% of combination therapy showed serum HBV DNA below detection limit (<0.5 pg/mL). Alanine aminotransferase (ALT) normalized in 78% and 82% respectively. Median Child-Pugh-Turcotte (CPT) score or Model for End-Stage Liver Disease (MELD) score reduced significantly by 3 or 5 point in monotherapy and 2 or 2 point in combination therapy respectively. There were no significant differences in rate of undetectable serum HBV DNA, median change of ALT and median reduction of CPT or MELD scores between the two groups. In conclusion, both adefovir dipivoxil monotherapy and combination therapy with ongoing lamivudine result in comparable virologic, biochemical, and clinical improvements in HBeAg-positive patients with decompensated liver function and lamivudine-resistant HBV. Combination with lamivudine showed no additional benefit over monotherapy during 24 weeks of treatment in these patients.
Chronic hepatitis B virus (HBV) infection is a worldwide health problem affecting an estimated 350 million individuals in the world, and is a leading cause of cirrhosis and hepatocellular carcinoma in Asian countries (1, 2). The therapeutic goal in patients with chronic HBV infection is to limit or to reverse the progression of the disease through sustained suppression of HBV replication (3).
Lamivudine, an oral nucleoside analogue, potentially inhibits HBV replication by interfering with HBV DNA polymerase and results in serum alanine aminotransferase (ALT) level normalisation, hepatitis B e antigen (HBeAg) seroconversion enhancement and liver histology improvement (3-11). However, these effects are not sustained in a significant proportion of patients due to the development of drug resistance, which is mediated largely by point mutations at the YMDD motif of the HBV DNA polymerase gene. By the end of one year of lamivudine therapy, 15 to 20% of patients have resistant HBV variants in the circulation; the figures rises to 67% by the fourth year (12, 13). Follow-up studies on continued lamivudine therapy after the emergence of YMDD mutation showed that acute exacerbation of hepatitis with hepatic decompensation may occur (13-15). Moreover, even fatal hepatic failure cases by lamivudine-resistant HBV during lamivudine therapy have been reported (16, 17).
Orthotopic liver transplantation can be an option for patients with hepatic decompensation by lamivudine-resistant HBV. However, patients with high serum levels of lamivudine-resistant HBV DNA may be unable to undergo liver transplantation, as they are at high risk for recurrent HBV infection in the liver graft besides an inadequate supply of donor livers (18). Consequently, there is a clear need for a safe and effective treatment regimen for patients with decompensated liver disease by lamivudine-resistant HBV.
Adefovir dipivoxil is an oral prodrug of an acyclic monophosphate adenine analog, which is a selective inhibitor of DNA polymerase and reverse transcriptase of HBV and has been shown to suppress potently both lamivudine-resistant and wild-type HBV (19-21). A randomized controlled study in patients with compensated liver disease and lamivudine-resistant HBV showed that adefovir dipivoxil was potent in suppression of lamivudine-resistant HBV replication, while lamivudine provided little or no additional benefit in combination therapy (21). However, in patients with hepatic decompensation and lamivudine-resistant HBV, the clinical benefit and safety of adefovir dipivoxil monotherapy compared to adefovir dipivoxil/lamivudine combination therapy has not been reported in controlled trials so far. Two separate uncontrolled studies showed that addition of adefovir dipivoxil to ongoing lamivudine decreased HBV DNA levels and improved biochemical markers (22, 23). However, they did not evaluate the effects of switching from lamivudine to adefovir dipivoxil monotherapy. Moreover, in another study, adefovir dipivoxil was reported to be associated with deterioration of renal function in patients with recurrent hepatitis B after liver transplantation or with decompensated hepatitis B in need of transplantation (24).
We performed this prospective, open-labeled, controlled study to evaluate the efficacy and safety of adefovir dipivoxil monotherapy and adefovir dipivoxil/lamivudine combination therapy in patients with decompensated liver disease and lamivudine-resistant HBV.
Patients eligible for the study were 18-67 yr of age with serum hepatitis B surface antigen (HBsAg) for at least 6 month, positive for HBeAg, and had an elevated serum ALT levels >1.3 times upper limit of normal (ULN) on at least two occasions at least two months apart and decompensated hepatic function. All patients had received lamivudine treatment for at least 6 months that was ongoing at the time of screening and had serum HBV DNA level ≥2.5 pg/mL, as measured by Digene Hybrid Capture II assay (Digene Corporation, Gaithersburg, MD, U.S.A.). Decompensation of hepatic function was defined as the presence of one or more of the followings: 1) serum bilirubin level >two times ULN without other causes; 2) prothrombin time >3 sec prolonged; 3) serum albumin level <3.2 g/dL; 4) a history of ascites, variceal hemorrhage, or hepatic encephalopathy; 5) Child-Pugh-Turcotte (CPT) score ≥7 (23).
Patients were excluded from the study if they were HBeAg-negative or coinfected with hepatitis C virus, hepatitis delta virus or human immunodeficiency virus, or had prior use of adefovir dipivoxil or other drugs with activity against HBV within the 12 months preceding study screening. Patients were also excluded if they had a documented hepatocellular carcinoma, screening calculated creatinine clearance <50 mL/min, or serum creatinine level >1.5 mg/dL. The majority of patients were not candidates for liver transplantation because of social, economic and/or medical problems.
All patients and their relatives signed the informed consent form before enrollment. The study protocol was in accordance with the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the Investigation and Ethics Committee for Human Research (protocol No ADF20001) at Asan Medical Centre.
From June 2003 to February 2004, 52 consecutive patients were recruited at screening. Two of the 52 patients were excluded from the study because they had transplantation within two months of adefovir dipivoxil/lamivudine combination therapy. 3 patients with HBeAg-negative hepatitis B were also excluded from the study. One patient died of rapid progression of hepatic failure before the administration of adefovir dipivoxil. At baseline, the remaining 46 patients were assigned to switch from previous lamivudine monotherapy to either adefovir dipivoxil 10 mg once daily (n=18) or combination therapy with adefovir dipivoxil 10 mg once daily plus lamivudine 100 mg once daily (n=28) for 24 weeks. The assignment was made according to the patient's own preference for economic reasons. All patients were hospitalized before enrollment for close monitoring and subsequently followed up in outpatient clinic of our hospital. Serum biochemical test results, CPT score, Model for End-Stage Liver Disease (MELD) score, HBeAg, anti-HBe, and serum HBV DNA levels were recorded every eight weeks. The therapeutic efficacy was measured by the change of CPT or MELD score, serum HBV DNA levels and serum biochemical test results. Virologic response was defined as the loss of previously detectable serum HBV DNA.
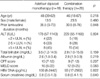
Baseline characteristics including age, sex, duration of prior lamivudine treatment, ALT level, total bilirubin level, CPT score, MELD score, and HBV DNA level were not statistically different between the two groups, although total bilirubin level and MELD score tended to be higher in patients receiving adefovir dipivoxil monotherapy than those receiving combination therapy (p=0.159 for total bilirubin level, p=0.083 for MELD score) (Table 1). All patients had normal serum creatinine levels and were hemodynamically stable at baseline.
A MALDI-TOF mass spectrometry-based genotyping assay, termed Restriction Fragment Mass Polymorphism (RFMP), was performed to detect hepatitis B virus mutations that confer resistance to lamivudine as previously described (25). This technique has been shown to be superior to DNA sequencing, as it is able to detect HBV mutations that confer resistance to lamivudine in the presence of wild-type virus background and is sensitive to a lower limit of 100 copies of HBV DNA/mL (25, 26). Blood samples to confirm the gene mutation within the YMDD motif were available in 24 of the 46 patients, and all patients with available samples had YMDD mutant HBV.
The associations of categorical variables such as sex, HBeAg loss or HBeAg seroconversion between the two groups were evaluated using Fisher's exact test. Continuous variables such as ALT level, total bilirubin level, HBV DNA level, age, CPT score, and MELD score between the two groups were compared using Wilcoxon rank sum test. The Wilcoxon signed rank test was used to compare changes of the paired data in each group. The correlation between baseline ALT level and change of CPT or MELD score after 24 weeks of treatment was analyzed using Spearman's rank correlation. p-values of less than 0.05 were considered to be statistically significant. The analysis software was Statistical Package for the Social Sciences, version 11.0 (SPSS Inc., Chicago, IL, U.S.A.).
The median serum HBV DNA levels decreased rapidly and remained low during the 24 weeks of treatment in both groups (Fig. 1). At week 8, 10 (56%) of 18 patients in adefovir dipivoxil monotherapy group and 19 (68%) of 28 patients in combination therapy group had serum HBV DNA level below detection limit (<0.5 pg/mL) and the number of the patients with undetectable serum HBV DNA level increased to 15 (83%) and 24 (86%) in each group at week 24. Even in 7 patients who had detectable serum HBV DNA levels at week 24 in both groups, HBV DNA levels were much lower at week 24 than baseline (Table 2). There was no significant difference in the rate of undetectable serum HBV DNA between the two groups (p=1.000).
Loss of HBeAg occurred in 4 (22%) patients in adefovir dipivoxil monotherapy group and 8 (28%) in combination therapy group at week 24. HBeAg seroconversion (HBeAg negative and anti-HBe positive) occurred in 3 (17%) and 6 (21%) patients in each group respectively. However, there was no significant difference in the rate of HBeAg loss or HBeAg seroconversion between the two groups (p=1.000 in both comparisons).
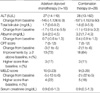
The median serum ALT levels in both groups decreased rapidly and remained lower than the baseline levels throughout the 24-week period (Fig. 2). Median reductions in serum ALT levels were 145 IU/L in adefovir dipivoxil monotherapy group and 197 IU/L in combination therapy group at week 24 (Table 3). There was no significant difference in median reduction of serum ALT levels between the two groups (p=0.778). 7 (39%) patients in adefovir dipivoxil monotherapy group and 13 (46%) in combination therapy group had normal serum ALT levels at week 8, and 14 (78%) and 23 (82%) patients at week 24 respectively.
The median total bilirubin levels decreased significantly from 3.5 at baseline to 1.7 mg/dL at week 24 in adefovir dipivoxil monotherapy group (p=0.026) and from 2.8 to 1.6 mg/dL in combination therapy group (p=0.000). Although the median reduction of total bilirubin levels was 1.7 or 1.1 mg/dL in each group respectively (Table 3), there was no significant difference in the median reduction of total bilirubin levels between the two groups (p=0.581).
The median CPT score decreased from 10 at baseline to 7 at week 24 in adefovir dipivoxil monotherapy group and from 9 to 7 in combination therapy group. The reduction of CPT score from baseline to week 24 in each group was significant respectively (p=0.001 in monotherapy group, p<0.001 in combination therapy group). However, the difference of median reduction of CPT score between the two groups was not significant (p=0.276). 13 (72%) patients in monotherapy group and 18 (64%) in combination therapy group had CPT score improvement by ≥2 point from baseline at week 24. Despite overall improvements of CPT score in both groups, 3 (17%) patients in monotherapy group and 3 (11%) in combination therapy group had higher CPT scores at week 24 than baseline (Table 3). Although 2 of the 6 patients with increased CPT scores had detectable HBV DNA levels at week 24, ALT levels and HBV DNA levels of these patients remained lower at week 24 than baseline (Table 2, case 2 and 6).
The median MELD score was 16 in adefovir dipivoxil monotherapy group and 12 in combination therapy group at baseline, and 10 and 9 at week 24 respectively (Table 3). A significant reduction of MELD scores was observed in each group at week 24 (p=0.009 in monotherapy group, p<0.001 in combination therapy group) (Fig. 3). However, there was no significant difference in median reduction of MELD score between the two groups (p=0.405). Deterioration in MELD scores was observed in 4 (22%) patients in monotherapy group and 5 (18%) in combination therapy group at week 24 (Table 3). Although 3 of the 9 patients with increased MELD scores had detectable HBV DNA level at week 24, ALT levels and HBV DNA levels at week 24 remained lower than baseline (Table 2, case 1, 2 and 6).
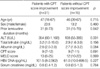
All the enrolled 46 patients were divided into two groups according to the degree of improvement in CPT score. 31 patients who had improvement of ≥2 point in CTP score and the remaining 15 patients were evaluated separately. In univariate analysis, baseline ALT level was the only significant factor associated with CPT score improvement of ≥2 point (Table 4). Furthermore, there was a statistically significant negative correlation between baseline ALT levels and the changes of CPT or MELD score from baseline to week 24 in the patients of both groups (correlation coefficients were -0.382 for CPT score, p=0.009, and -0.347 for MELD score, p=0.018).
Among all 46 patients, the median creatinine levels increased significantly from 0.8 mg/dL at baseline to 0.9 at week 24 (p=0.006). However, an increase in serum creatinine level of ≥0.5 mg/dL above baseline was observed in only two patients. In one patient, serum creatinine level increased from 0.9 mg/dL at baseline to 1.4 at week 16, but adefovir dipivoxil was continuously administered without dose reduction because her creatinine level was still within ULN (≤1.5 mg/dL). There was no further increase of serum creatinine level during the 24 week treatment. The other patient's creatinine level increased from 0.8 mg/dL at baseline to 1.3 at week 24. No one developed a decreased serum phosphate level of <1.5 mg/dL.
Two patients had higher ALT levels at week 24 than their baseline levels. One patient received adefovir dipivoxil alone, and his CPT and MELD score were improved by 4 and 8 point at week 24 respectively. The other received combination therapy, and his CPT and MELD score worsened by 1 and 5 point at week 24 respectively. None of the elevation in ALT levels was accompanied by detectable serum HBV DNA.
There was no death or drug-induced other serious adverse event during the 24 weeks of treatment.
The present study indicates that both adefovir dipivoxil monotherapy and adefovir dipivoxil/lamivudine combination therapy for 24 weeks resulted in significant virologic and clinical improvements in patients with decompensated liver disease and lamivudine-resistant HBV, who were not candidates for liver transplantation. Both therapies led to marked and rapid suppression of viral replication. At week 24, 83% of adefovir dipivoxil monotherapy group and 86% of combination therapy group had undetectable HBV DNA level. ALT levels normalized in 78% of adefovir dipivoxil group and 82% of adefovir dipivoxil/lamivudine group at week 24. 72% and 64% of each group, respectively, had improvement in liver function, as evidenced by a ≥2 point improvement in CPT score. Furthermore, 22% and 28% of each group achieved HBeAg loss, while HBeAg seroconversion occurred in 17% and 21% respectively at week 24. The rate of HBeAg loss or HBeAg seroconversion in our study is little bit higher than those achieved in patients with compensated liver disease and lamivudine-resistant HBV, in which only 16% of adefovir dipivoxil group and 17% of adefovir dipivoxil/lamivudine group were HBeAg negative and 11% and 6% of each group achieved HBeAg seroconversion at week 48 (21). These findings may be related to the high baseline ALT levels of decompensated patients in our study, which is suggested in previous studies showing that chronic hepatitis B patients with higher pretreatment ALT levels have significantly enhanced HBeAg seroconversion rates during lamivudine treatment (27, 28).
Our results of adefovir dipivoxil/lamivudine combination therapy are in agreement with the findings of other uncontrolled studies in which the addition of adefovir dipivoxil to lamivudine treatment were evaluated in patients with decompensated chronic hepatitis B resistant to lamivudine and in pre- and post-liver transplantation patients with active liver disease due to lamivudine-resistant HBV respectively (22, 23). Moreover, in the present controlled study, adefovir dipivoxil monotherapy was as effective as adefovir dipivoxil/lamivudine combination in suppressing viral replication. These findings suggest that the continuation of lamivudine has no additional or synergistic effect over adefovir dipivoxil monotherapy in these patients, which are similar to the findings of the study performed in patients with compensated chronic hepatitis B and lamivudine-resistant HBV (21). Because wild-type HBV emerges rapidly over HBV mutants after the discontinuation of lamivudine or a switch to adefovir dipivoxil monotherapy, the virologic responses observed in adefovir dipivoxil monotherapy group in our study support the findings of previous studies that adefovir dipivoxil is active against both wild-type and lamivudine-resistant HBV (19-21).
In patients with chronic hepatitis B with lamivudine-resistant HBV, it is reported that about 16% of patients experience ALT flares after the withdrawal of lamivudine by reversion of wild-type HBV and 5% of patients with ALT flare experience severe acute exacerbation of chronic hepatitis B (29). In the previous study of compensated patients with lamivudine-resistant chronic hepatitis B, about one-third of patients receiving the adefovir dipivoxil monotherapy experienced ALT flares within 12 weeks. However, these ALT flares were not accompanied by concurrent elevations of HBV DNA levels and/or signs of reduced hepatic function, or even associated with reversion to wild-type HBV (21). In the present study, only one patient receiving adefovir monotherapy had higher ALT level than the baseline at week 24, and undetectable HBV DNA level and improved CTP score. However, because the number of patients receiving adefovir dipivoxil monotherapy was relatively small and laboratory data were recorded every 8 weeks, it is possible that the ALT flares within the eight-week period might not be detected in our study.
Although adefovir dipivoxil was effective in improving liver function in our patients, approximately 28% of adefovir dipivoxil monotherapy group and 36% of combination therapy group failed to show significant clinical responses, as evidenced by the improvement of CPT scores ≥2 point, despite the overall virologic and biochemical improvement. These observations could result from the differences in the severity of pre-existing liver damage rather than the differences in virologic response, indicating that there may be a point in the natural history of decompensated HBV infection after when the application of antiviral therapy may be of limited benefit.
In the present study, CPT score improvement of ≥2 point was significantly associated with higher baseline ALT levels. Furthermore there was a significant correlation between the baseline ALT levels and the improvement of CPT or MELD score. This suggests that the hepatic function is more likely to be reversible in decompensated patients with higher necroinflammatory activity resulting from active viral replication. Thus, the effective suppression of the viral load by adefovir dipivoxil may result in a decrease of the necroinflammatory activity of the liver and eventually lead to clinical improvement.
Adefovir dipivoxil was generally well-tolerated during the 24-week treatment period in the current study, as shown in other studies (22, 23). No patient discontinued adefovir dipivoxil due to drug-related adverse events. Furthermore, there was no development of nephrotoxicity due to adefovir dipivoxil in our patients with decompensated liver disease and normal renal function.
It can be argued that this study does not prove the efficacy of adefovir dipivoxil because we did not include a control group with lamivudine monotherapy matched for the severity of hepatic decompensation due to lamivudine-resistant HBV. However, considering the current knowledge of the poor prognosis of decompensated cirrhosis and diminished clinical and virologic response of continued lamivudine monotherapy in patients with YMDD mutant HBV (4, 13-15, 30), such an approach would raise critical ethical concerns especially in patients with decompensated liver function due to lamivudine-resistant HBV.
Our study has other limitations. First, the treatment period was relatively short for only 24 weeks. However, previous experiences with lamivudine therapy for decompensated HBV-cirrhosis have suggested that six-month survival rates with antiviral treatment might be sufficient to predict substantially longer survival rates (6, 7, 10, 11). Second, because patients were not randomly assigned into two groups, there were slight differences in baseline characteristics such as MELD score between the two groups. However, the differences were not statistically significant. Finally, HBV polymerase gene mutation within the YMDD motif was not performed in all patients.
In summary, the current study shows that a 24-week course of adefovir dipivoxil alone or in combination with lamivudine results in significant suppression of HBV replication, normalisation of ALT levels, HBeAg loss or seroconversion, and overall improvement in CPT and MELD score without any significant treatment-related adverse events in decompensated patients with lamivudine-resistant HBV. The virologic, biochemical and clinical responses of the two adefovir dipivoxil containing regimens seems to be similar suggesting that continuation of lamivudine may not confer any further benefit over adefovir dipivoxil monotherapy in these patients. A further study is warranted to confirm the long term effect and safety of adefovir dipivoxil monotherapy in patients with lamivudine-resistant decompensated chronic hepatitis B.
Figures and Tables
Fig. 1
Median values of HBV DNA levels in adefovir dipivoxil monotherapy and adefovir dipivoxil/lamivudine combination therapy group over 24 weeks of treatment. Median serum HBV DNA levels decreased rapidly within 8 weeks and remained low throughout the 24 weeks in both groups. The 0 marker on Y axis more accurately represents a value of <0.5 pg/mL HBV DNA because the lower limit of detection of Digene Hybrid Capture II assay used for measurement of HBV DNA was 0.5 pg/mL. The horizontal lines in the box mark the 25th, 50th, and 75th percentiles of the data. Error bars extend from the quartiles to the farthest observation.

Fig. 2
Median values of ALT levels in adefovir dipivoxil monotherapy and adefovir dipivoxil/lamivudine combination therapy group over 24 weeks of treatment. Median ALT levels decreased rapidly within 8 weeks and remained lower than the baseline levels throughout the 24 weeks in both groups. The horizontal lines in the box mark the 25th, 50th, and 75th percentiles of the data. Error bars extend from the quartiles to the farthest observation.

Fig. 3
Changes of MELD score at baseline and at week 24 in adefovir dipivoxil monotherapy and adefovir dipivoxil/lamivudine combination therapy group. There was a significant reduction of median values of MELD score at week 24 compared with baseline in both groups.

Table 2
Changes in serum HBV DNA levels, serum ALT levels and CPT (MELD) scores in patients who had detectable serum HBV DNA levels at week 24

References
2. Ganem D, Prince AM. Hepatitis B virus infection-natural history and clinical consequences. N Engl J Med. 2004. 350:1118–1129.
3. Conjeevaram HS, Lok AS. Management of chronic hepatitis B. J Hepatol. 2003. 38:Suppl 1. S90–S103.

4. Dienstag JL, Goldin RD, Heathcote EJ, Hann HW, Woessner M, Stephenson SL, Gardner S, Gray DF, Schiff ER. Histological outcome during long-term lamivudine therapy. Gastroenterology. 2003. 124:105–117.

5. Liaw YF, Sung JJ, Chow WC, Farrell G, Lee CZ, Yuen H, Tanwandee T, Tao QM, Shue K, Keene ON, Dixon JS, Gray DF, Sabbat J. Cirrhosis Asian Lamivudine Multicentre Study Group. Lamivudine for patients with chronic hepatitis B and advanced liver disease. N Engl J Med. 2004. 351:1521–1531.

6. Jung S, Suh DJ, Park HJ, Park YH, Song HG, Lee HC, Chung YH, Lee YS. Therapeutic efficacy of lamivudine in patients with hepatitis B virus-related decompensated cirrhosis in Korea. Korean J Hepatol. 2002. 8:418–427.
7. Kapoor D, Guptan RC, Wakil SM, Kazim SN, Kaul R, Agarwal SR, Raisuddin S, Hasnain SE, Sarin SK. Beneficial effects of lamivudine in hepatitis B virus-related decompensated cirrhosis. J Hepatol. 2000. 33:308–312.

8. Hann HW, Fontana RJ, Wright T, Everson G, Baker A, Schiff ER, Riely C, Anschuetz G, Gardner SD, Brown N, Griffiths D. United States Lamivudine Compassionate Use Study Group. A United States compassionate use study of lamivudine treatment in nontransplantation candidates with decompensated hepatitis B virus-related cirrhosis. Liver Transpl. 2003. 9:49–56.

9. Villeneuve JP, Condreay LD, Willems B, Pomier-Layrargues G, Fenyves D, Bilodeau M, Leduc R, Peltekian K, Wong F, Margulies M, Heathcote EJ. Lamivudine treatment for decompensated cirrhosis resulting from chronic hepatitis B. Hepatology. 2000. 31:207–210.

10. Yao FY, Bass NM. Lamivudine treatment in patients with severely decompensated cirrhosis due to replicating hepatitis B infection. J Hepatol. 2000. 33:301–307.

11. Yao FY, Terrault NA, Freise C, Maslow L, Bass NM. Lamivudine treatment is beneficial in patients with severely decompensated cirrhosis and actively replicating hepatitis B infection awaiting liver transplantation: a comparative study using a matched, untreated cohort. Hepatology. 2001. 34:411–416.

12. Liaw YF, Leung NW, Chang TT, Guan R, Tai DI, Ng KY, Chien RN, Dent J, Roman L, Edmundson S, Lai CL. Effects of extended lamivudine therapy in Asian patients with chronic hepatitis B. Gastroenterology. 2000. 119:172–180.

13. Chang TT, Lai CL, Chien RN, Guan R, Lim SG, Lee CM, Ng KY, Nicholls GJ, Dent JC, Leung NW. Four years of lamivudine treatment in Chinese patients with chronic hepatitis B. J Gastroenterol Hepatol. 2004. 19:1276–1282.

14. Wong VW, Chan HL, Wong ML, Tam JS, Leung NW. Clinical course after stopping lamivudine in chronic hepatitis B patients with lamivudine-resistant mutants. Aliment Pharmacol Ther. 2004. 19:323–329.

15. Angus P, Locarnini S. Lamivudine-resistant hepatitis B virus and ongoing lamivudine therapy: stop the merry-go-round, it's time to get off! Antivir Ther. 2004. 9:145–148.
16. Kagawa T, Watanabe N, Kanouda H, Takayama I, Shiba T, Kanai T, Kawazoe K, Takashimizu S, Kumaki N, Shimamura K, Matsuzaki S, Mine T. Fatal liver failure due to reactivation of lamivudine-resistant HBV mutant. World J Gastroenterol. 2004. 10:1686–1687.

17. Kim JW, Lee HS, Woo GH, Yoon JH, Jang JJ, Chi JG, Kim CY. Fatal submassive hepatic necrosis associated with tyrosine-methionine-aspartate-aspartate-motif mutation of hepatitis B virus after long-term lamivudine therapy. Clin Infect Dis. 2001. 33:403–405.

18. Samuel D, Muller R, Alexander G, Fassati L, Ducot B, Benhamou JP, Bismuth H. Liver transplantation in European patients with the hepatitis B surface antigen. N Engl J Med. 1993. 329:1842–1847.

19. Marcellin P, Chang TT, Lim SG, Tong MJ, Sievert W, Shiffman ML, Jeffers L, Goodman Z, Wulfsohn MS, Xiong S, Fry J, Brosgart CL. Adefovir Dipivoxil 437 Study Group. Adefovir dipivoxil for the treatment of hepatitis B e antigen-positive chronic hepatitis B. N Engl J Med. 2003. 348:808–816.

20. Hadziyannis SJ, Tassopoulos NC, Heathcote EJ, Chang TT, Kitis G, Rizzetto M, Marcellin P, Lim SG, Goodman Z, Wulfsohn MS, Xiong S, Fry J, Brosgart CL. Adefovir Dipivoxil 438 Study Group. Adefovir dipivoxil for the treatment of hepatitis B e antigen-negative chronic hepatitis B. N Engl J Med. 2003. 348:800–807.

21. Peters MG, Hann Hw, Martin P, Heathcote EJ, Buggisch P, Rubin R, Bourliere M, Kowdley K, Trepo C, Gray Df, Sullivan M, Kleber K, Ebrahimi R, Xiong S, Brosgart CL. Adefovir dipivoxil alone or in combination with lamivudine in patients with lamivudine-resistant chronic hepatitis B. Gastroenterology. 2004. 126:91–101.
22. Schiff ER, Lai CL, Hadziyannis S, Neuhaus P, Terrault N, Colombo M, Tillmann HL, Samuel D, Zeuzem S, Lilly L, Rendina M, Villeneuve JP, Lama N, James C, Wulfsohn MS, Namini H, Westland C, Xiong S, Choy GS, Van Doren S, Fry J, Brosgart CL. Behalf of the Adefovir Dipovoxil Study 435 International Investigators Group. Adefovir dipivoxil therapy for lamivudine-resistant hepatitis B in pre- and post-liver transplantation patients. Hepatology. 2003. 38:1419–1427.

23. Perrillo R, Hann HW, Mutimer D, Willems B, Leung N, Lee WM, Moorat A, Gardner S, Woessner M, Bourne E, Brosgart CL, Schiff E. Adefovir dipivoxil added to ongoing lamivudine in chronic hepatitis B with YMDD mutant hepatitis B virus. Gastroenterology. 2004. 126:81–90.

24. Schiff E, Neuhaus P, Tillman HL, Samuel D, Terrault N, Marcellin P, Lama N. Safety and efficacy of adefovir dipivoxil for the treatment of lamivudine resistant HBV in patients post liver transplantation [abstract]. Hepatology. 2001. 34:446A.
25. Hong SP, Kim NK, Hwang SG, Chung HJ, Kim S, Han JH, Kim HT, Rim KS, Kang MS, Yoo W, Kim SO. Detection of hepatitis B virus YMDD variants using mass spectrometric analysis of oligonucleotide fragments. J Hepatol. 2004. 40:837–844.
27. Chien RN, Liaw YF, Atkins M. Pretherapy alanine transaminase level as a determinant for hepatitis B e antigen seroconversion during lamivudine therapy in patients with chronic hepatitis B. Hepatology. 1999. 30:770–774.

28. Lai CL, Chien RN, Leung NW, Chang TT, Guan R, Tai DI, Ng KY, Wu PC, Dent JC, Barber J, Stephenson SL, Gray DF. A one-year trial of lamivudine for chronic hepatitis B. N Engl J Med. 1998. 339:61–68.

29. Honkoop P, de Man RA, Niesters HG, Zondervan PE, Schalm SW. Acute exacerbation of chronic hepatitis B virus infection after withdrawal of lamivudine therapy. Hepatology. 2000. 32:635–639.

30. Lai CL, Dienstag J, Schiff E, Leung NW, Atkins M, Hunt C, Brown N, Woessner M, Boehme R, Condreay L. Prevalence and clinical correlates chronic hepatitis B. Clin Infect Dis. 2003. 36:687–696.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download