Abstract
Intravascular papillary endothelial hyperplasia (Masson's hemangioma) is a disease characterized by exuberant endothelial proliferation within the lumen of medium-sized veins. In 1923, Masson regarded this disease as a neoplasm inducing endothelial proliferation, however, now it is considered to be a reactive vascular proliferation following traumatic vascular stasis. The lesion has a propensity to occur in the head, neck, fingers, and trunk. Occurrence within the abdominal cavity is known to be very rare, and especially in the liver, there has been no reported case up to date. The authors have experienced intravascular papillary endothelial hyperplasia of the liver in a 69-yr-old woman, and report the case with a review of the literature.
First named 'hemangioendotheliome vegetant intravasculaire' by Masson (1) in 1923, Masson's hemangioma is an exuberant endothelial proliferation that requires differential diagnosis from angiosarcoma. Masson described it to be a form of neoplasm and explained the pathogenesis as the proliferation of endothelial cells into the vessel lumen, followed by obstruction and subsequent secondary degeneration and necrosis. On the other hand, Henschen (2) depicted the lesion as a reactive process rather than a neoplasm. Kauffman and Stout (3) remarked that although endothelial proliferation that can be mistaken for a characteristic of sarcoma is present, the endothelial layer of the lesion is composed of normal endothelial cells, the endothelial proliferation is of benign papillae pattern, and the cells show no atypia. Nowadays, it is considered to be a reactive vascular proliferation following traumatic vascular stasis.
According to the reported cases so far, the lesion occurs in the fingers, head and neck, trunk, lower extremities, and upper extremities, in order decreasing frequency. No report has been made of the lesion occurring in the organs of the abdominal cavity, especially the liver.
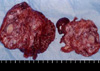
We report here a new hepatic lesion in a 69-yr-old Korean woman with a left hepatic tumor. The authors diagnosed the patient as having intravascular papillary endothelial hyperplasia of the liver based on the following findings : characteristic fibrohyalinized tissue surrounded by papillary structure of a single endothelial cell layer, forming irregular sponge-like reticular pattern; papillary endothelial proliferation occurring within the vessel lumen; a large amount of hematoma in the center and the scarcity of solid tissue and necrotic debris; and the paucity of cellular atypia and mitotic figures.
A 69-yr-old woman presenting with myalgia, fever, chill, and epigastric pain for 10 days visited a private clinic and was diagnosed with tsutsugamushi disease. The patient was transferred to our hospital because of abnormal liver function and received further study and management. She had no remarkable past medical history. The vital signs were all normal, except for a slightly increased body temperature at 37.2℃. Physical examination revealed no abnormal findings.
Initial laboratory data included a white blood cell count of 3,400/µL, hemoglobin 11.8 g/dL, hematocrit 35.6%, platelet counts 116,000/µL, FBS 290 mg/dL, BUN 5.5 mg/dL, creatinine 0.5 mg/dL, sodium 137 mEq/L, potassium 3.8 mEq/L, AST 194 IU/L, ALT/186 IU/L, total bilirubin 0.6 IU/L, direct bilirubin 0.2 IU/L, amylase 38 U/L, and normal urinalysis results.
Abdominal CT scan showed a 10×7 cm-sized, lobulated, heterogenous contrast enhancing, soft tissue mass involving the entire left hepatic lobe. The tumor showed focal nodular enhancement around the peripheral portion of the hepatic mass during the arterial phase, and an increased extent of peripheral nodular contrast-enhancement with a persistent low density noncontrast-enhancing portion in the center of the tumor during the delayed phase (Fig. 1, 2). The angiography illustrated some tumor supplying arteries from the left hepatic artery, with no evidence of gross invasion to the main arteries (Fig. 3). MRCP (magnetic resonance cholangio-pancreatogram) revealed no dilatation of the intrahepatic duct or the common bile duct. The left intrahepatic duct was not visualized, probably due to tumor replacement (Fig. 4).
Under the suspicion of cholangiocarcinoma or hemangiosarcoma, the patient underwent left hemihepatectomy including the caudate lobe with surrounding lymphadenectomy. The mass seen during operation was limited to the left lobe, of 10×7 cm size, and was a non-homogenous multinodular mass including a focal necrosis. No major vessel invasion was observed (Fig. 5).
Thrombotic material fragmented and entrapped by the ingrowing endothelial cells was reported by the pathologist. There was no soft tissue invasion, atypia, or significant necrosis, which collectively supported the diagnosis of intravascular papillary endothelial hyperplasia (Masson's hemangioma) of the liver (Fig. 6). The surgical procedure and recovery period were not complicated.
Intravascular papillary endothelial hyperplasia is a peculiar benign intravascular process that bears a remarkable resemblance to a hemangiosarcoma. In 1923, Pierre Masson (1) first described an intravascular papillary proliferation formed within the lumen of inflamed hemorrhoidal plexus in a 68-yr-old man. He termed the lesion "vegetant intravascular hemangioendothelioma." He believed the lesion to be a proliferation of endothelial cells, resulting in the obliteration of the vascular lumen, and causing degeneration and necrosis in the manner of secondary red infarct. In 1932, Henschen (2) portrayed a similar endothelial proliferation, but he regarded it more as a reactive process than an endothelial neoplasm. The lesion came to be called "L'endovasculite proliferante thrombopoietique", or Masson's intravascular vegetant hemangioendothelioma (4, 5). Through numerous further studies, scholars stated that this lesion is a vascular proliferation reaction following traumatic vascular stasis, rather than a true neoplasm. This hypothesis formed a quick consensus, and the term intravascular papillary endothelial hyperplasia, first named by Clearkin and Enzinger (6) in 1976, is most widely used instead of the mistaken definition of Masson's pseudoangiosarcoma.
According to the reported cases so far, there is no gender or age predilection, as it occurs in males and females ranging from ages 9 months to 80 yr. Clinically, intravascular papillary endothelial hyperplasia occurs most frequently in the head and neck, fingers, trunk, and cutaneous vein as a small, firm, superficial mass, with red to blue discoloration of the overlying skin (5-10). Intravascular papillary endothelial hyperplasia of the abdominal cavity is considered to be very rare, and hepatic lesion has never been documented anywhere in the world (5-11).
Histologically, intravascular papillary endothelial hyperplasia has a characteristic exuberant endothelial proliferation within the lumen of medium-sized veins. Microscopically, the tuftlike or papillary proliferation of endothelial cells was nearly always intimately associated with a thrombus and seemed to represent a peculiar variant of an organizing process. The papillary structure and exuberant endothelialization of intravascular papillary endothelial hyperplasia necessitate ruling out angiosarcoma. The following features are important in the differential diagnosis: 1) intravascular papillary endothelial hyperplasia is often well-circumscribed or encapsulated; 2) the proliferative process is limited completely to the intravascular spaces; 3) though the endothelial cells are hyperchromatic, extreme nuclear atypia and frequent mitotic figures cannot be seen; 4) papillae are composed of fibro-hyalinized tissue of two or more endothelial cell layers without any covering; 5) there are no true endothelial confirm in intravascular papillary endothelial hyperplasia; 6) tangential sectioning may reveal pseudochannels, but no irregular and anastomosing blood vessels in the stroma; and 7) necrosis is an unusual finding in intravascular papillary endothelial hyperplasia (12).
In summary, we report the first case of intravascular papillary endothelial hyperplasia arising in the liver in a 69-yr-old female patient. The patient underwent left hemihepatectomy including the caudate lobe for the left hepatic mass, and the postoperative follow-up has been uneventful.
Figures and Tables
Fig. 1
Abdominal CT shows a lobulated, heterogenous contrast enhancing, soft tissue mass involving the entire left hepatic lobe (10×7 cm). Note the focal nodular enhancement around the peripheral portion of the hepatic mass in arterial phase.
Fig. 2
Abdominal CT shows an increased extent of peripheral nodular contrast-enhancement with a persistent low density noncontrast-enhancing portion of the tumor centrally in delayed phase.
Fig. 3
Angiography shows some tumor-supplying arteries from the left hepatic artery. There is no evidence of gross invasion in the main arteries.
References
1. Masson P. Hemangioendotheliome vegetant intravasculaire. Bull Soc Anat Paris. 1923. 93:517–523.
2. Henschen P. L'endovasculite proliferante thrombopoietique dans la lesion vasculaire locale. Ann Anat Pathol. 1932. 9:113–121.
3. Kauffman SL, Stout AP. Malignant hemangioendothelioma in infants and children. Cancer. 1961. 14:1186–1196.

4. Eusebi V, Fanti PA, Fedeli F, Mancini AM. Masson's intravascular vegetant hemangioendothelioma. Tumori. 1980. 66:489–498.

5. Kuo T, Sayers CP, Rosai J. Masson's "vegetant intravascular hemangioendothelioma:" a lesion often mistaken for angiosarcoma: study of seventeen cases located in the skin and soft tissues. Cancer. 1976. 38:1227–1236.
6. Clearkin KP, Enzinger FM. Intravascular papillary endothelial hyperplasia. Arch Pathol Lab Med. 1976. 100:441–444.
7. Hashimoto H, Daimaru Y, Enjoji M. Intravascular papillary endothelial hyperplasia: a clinicopathologic study of 91 cases. Am J Dermatopathol. 1983. 5:539–546.
8. Amerigo J, Berry CL. Intravascular papillary endothelial hyperplasia in the skin and subcutaneous tissue. Virchows Arch A Pathol Anat Histol. 1980. 387:81–90.
9. Schwartz IS, Parris A. Cutaneous intravascular papillary endothelial hyperplasia: a benign lesion that may simulate angiosarcoma. Cutis. 1982. 29:66–69. 72–74.
10. Park SJ, Kim HJ, Park SH, Yeo UC, Lee ES. A case of intravascular papillary endothelial hyperplasia on upper lip. Korean J Dermatol. 2000. 38:1693–1695.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download