Abstract
The primary ovarian lymphoma is a rare disease with poor prognosis. The incidence of autoimmune hemolytic anemia in patients with non-Hodgkin's lymphoma is estimated at 3%. However, a substantial portion of the previously reported cases of ovarian lymphoma actually represented ovarian involvement by more diffuse lymphomatous process. If stringent criteria are used for case selection, true primary ovarian lymphoma usually carries a favorable prognosis. We present a primary malignant lymphoma of ovary accompanied by autoimmune hemolytic anemia in a 29-yr-old patient. After ablative surgery, the hemoglobin level and the reticulocyte count were normalized. One year following surgery and chemotherapy, the patient is alive and disease free.
Secondary ovarian involvement by malignant lymphoma is well recognized with a frequency as high as 20-30% in some autopsy series (1). Primary ovarian lymphoma (POL) is quite rare and accounts for less than 0.8-1% of all lymphoma involving the ovary (2, 3). The incidence of autoimmune hemolytic anemia (AIHA) is known to be approximately 3% in patients with non-Hodgkin's lymphoma (NHL) (4, 5).
We report a case of POL and AIHA successfully managed with a combination of surgery and adjuvant chemotherapy.
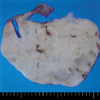
In September 2001, a 29-yr-old woman with low abdominal pain visited our emergency room. Laboratory data showed a hemoglobin level of 6.7 g/dL and a reticulocyte count of 7.2%. Serum direct/indirect bilirubin levels were 3.2/1.0 mg/dL. The lactate dehydrogenase level was 2,450 U/L. The direct and indirect Coomb's tests were positive. The erythrocyte sedimentation rate was 30 mm/hr. The C-reactive protein was not increased. The anti-nuclear antibody and anti-double-stranded DNA antibody were absent. The complement level was normal. Peripheral blood smear showed a normocytic normochromic anemia with red blood cell agglutination. The pelvis MRI showed a well marginated pelvic cavity mass (Fig. 1). We suspected a myoma or a solid adnexal tumor accompanied by AIHA. We concluded that AIHA should be treated first, and then exploratory laparotomy be needed.
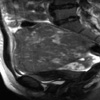
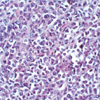
The patient was treated with prednisolone 1 mg/kg daily. The dosage of prednisolone was gradually tapered to 7.5 mg over the next 3 months. In November 2001, exploratory laparotomy revealed a 14 cm sized multinodular mass involving the right ovary. The mass was not adherent to the adjacent organs and was removed with the right Fallopian tube without difficulty. The left Fallopian tube, ovary, uterus, and kidneys were normal. The liver, diaphragm, and omentum were not involved. No enlarged lymph node, more than 1 cm size, was identified in the abdomen. Peritoneal washing was performed and the pathology finding revealed no abnormal cells. On gross examination, the right ovarian mass measured 14×10×9 cm. The cut surface of the ovarian mass revealed a solid, multilobulated tumor (Fig. 2). Microscopic examination revealed complete replacement of the ovarian tissue by sheets of neoplastic cells (Fig. 3). Paraffin immunoperoxidase studies showed strong positive marking of the neoplastic cell for CD45 (LCA) and CD20 (L-26).
Therefore, a diagnosis of NHL with the type of diffuse large B-cell was possible. The chest, abdomen, and neck computerized tomography scan were performed postoperatively and there were no evidence of abnormal lymph node enlargement. There were no specific abnormality on a 67Gallium scan, endoscopy, and bone marrow biopsy. Serum protein electrophoresis showed normal pattern.
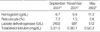
We stopped prednisolone but the hemoglobin level and the reticulocyte count were normalized (Table 1). The direct and indirect Coomb's test were converted to negative. In December 2001, the patient was treated with a combination of chemotherapeutic agents including vincristine, adriamycin, cyclophosphamide, and prednisolone with no major side-effect. One year following surgery and six cycles of chemotherapy, the patient alive and anemia free (Table 1).
POL is a rare disease and many authors have been questionable about the existence of disease entity. Since the normal ovary is devoid of any lymphoid tissue, other sources, such as lymphoid aggregates in the ovarian hilum or chronic inflammatory cells in the ovary in response to ovarian lesions, such as pelvic inflammatory disease or endometriosis, have been cited as possible origins for POL (6). More recent studies have found benign lymphoid aggregates in approximately half of normal ovaries (7). It is hypothetically possible that on rare occasion these lymphoid aggregates may undergo malignant transformation, giving to a POL (6).
In the past, the diagnosis of POL required only substantiation by histologic examination of the ovarian lesion. Many cases of POL reported in larger series were actually cases of malignant lymphoma with ovarian enlargement as the presenting symptom (8, 9). All types of lymphomas have been represented, mostly NHL with rare cases of Hodgkin's disease included (2, 9, 10). Only a few cases of POL have been reported, and the prognosis was generally poor with survival rates ranging from 7 to 38% (2, 11).
Fox et al. (12) proposed the following criteria for the diagnosis of POL: The lymphoma is clinically confined to the ovary at the time of diagnosis and full investigations fail to reveal evidence of lymphoma elsewhere. A lymphoma can still be considered to be of ovarian origin if spread has occurred to the immediately adjacent lymph nodes or if there has been direct spread infiltrating the immediately adjacent structures. The peripheral blood and bone marrow should not contain any abnormal cell. If further lymphomatous lesions occur at sites remote from the ovary, at least several months should have elapsed between the appearance of the ovarian and extraovarian lesions. If these stringent criteria are applied, POL becomes vanishingly rare, and only 20 cases have been reported in the world literature. Skodras et al. (13) reviewed the literature and found 15 cases of ovarian lymphoma meeting the above criteria. The patients'ages ranged from 2 to 63 yr (mean age, 37.7 yr). Nine patients were found to have diffuse large cell or mixed large and small cell lymphoma. Following treatment that consisted of ablative surgery with or without adjuvant chemotherapy, all 15 patients were alive with no evidence of disease except one who developed multiple local recurrences. Our patients met the criteria for POL and had a favorable outcome similar to those reviewed in this series.
The process of rearrangement of the immunoglobulin and T-cell receptor gene segments in the DNA of precursor lymphocytes not only allows the formation of a large number of complete genes, but also creates the potential for the generation of autoreactive lymphocytes on daily basis. Failure to eliminate these autoreactive cells or the breakdown in the mechanisms that prevent their expansion may lead to several autoimmune manifestations. Therefore, it is not surprising that patients with a tumor of the immune system such as B- or T-cell NHL are at risk of developing antibodies against hematopoietic cells or other tissues (4, 14, 15). Sallah et al. (5) reported that the patients with NHL/AIHA have poor prognosis. The impact of this finding on the recommendation that can be offered based on this report is two fold. First, consideration should be given for the inclusion of immunomodulators such as cyclosporine or other agents in the treatment regimens of patients with NHL who develop AIHA with an emphasis on achieving rapid resolution of the hemolytic process. Second, AIHA should be included in the risk-stratification of patients with NHL as an adverse prognotic sign. Our patient was resolved from a AIHA by a combination of prednisolone and surgery.
In summary, we report a case of POL accompanied by AIHA, which was successfully managed with a combination of surgery and chemotherapy.
Figures and Tables
Fig. 2
The cut surface of the right ovarian lesion shows a solid, gray white to yellow, multilobulated tumor.
References
1. Mittal KR, Blechman A, Greco MA, Alfonso F, Demopoulos R. Lymphoma of ovary with stromal luteinization, presenting as secondary amenorrhea. Gynecol Oncol. 1992. 45:69–75.

2. Chorlton I, Norris HJ, King FM. Malignant reticuloendothelial disease involving the ovary as a primary manifestation: a series of 19 lymphomas and 1 granulocytic sarcoma. Cancer. 1974. 34:397–407.

3. Oh SY, Kim JW, Park NH, Song YS, Kang SB, Lee HP. A case of primary ovarian lymphoma. Korean J Obstet Gynecol. 1997. 40:1090–1096.
4. Gronbak K, D'Amore F, Schmidt K. Autoimmune phenomena in non-Hodkin's lymphoma. Leuk Lymphoma. 1995. 18:311–316.
5. Sallah S, Sigounas G, Vos P, Wan JY, Nguyen NP. Autoimmune hemolytic anemia in patients with non-Hodgkin's lymphoma: characteristics and significance. Ann Oncol. 2000. 11:1571–1577.

6. Woodruff JD, Noli Castilla RD, Novak FR. Lymphoma of the ovary: a study of 35 cases from the Ovarian Tumor Registry of the American Gynecological Society. Am J Obstet Gynecol. 1963. 185:912.
7. Monterroso V, Jaffe ES, Merino MJ, Medeiros LJ. Malignant lymphomas involving the ovary: clinicopathologic analysis of 39 cases. Am J Surg Pathol. 1993. 17:154–170.
8. Dao AH. Malignant lymphoma of the ovary: reports of a case successfully managed with surgery and chemotherapy. Gynec Oncol. 1998. 70:137–140.
9. Dimopoulos MA, Daliani D, Pugh W, Gershenson D, Cabanillas F, Sarris AH. Primary ovarian non-Hodgkin's lymphoma: outcome after treatment with combination chemotherapy. Gynec Oncol. 1982. 64:446–450.

10. Rotmensh J, Woodruff JD. Lymphoma of the ovary: report of twenty new cases and update of previous series. Am J Obstet Gynecol. 1982. 143:870–875.
11. Osborne BM, Robboy SJ. Lymphomas or leukemia presenting as ovarian tumors: an analysis of 42 cases. Cancer. 1983. 35:1933–1943.

12. Fox H, Langley FA. Tumors of the ovary. 1976. London: Heinemann;293.
13. Skodras G, Fields V, Kragel PJ. Ovarian lymphoma and serous carcinoma of low malignant potential arising in the same ovary: a case report with literature review of 14 primary ovarian lymphomas. Arch Pathol Lab Med. 1994. 118:647–650.
14. Polliack A, Lugassy G. Autoimmunity and auto-immune syndromes associated with and preceding the development of lymphoproliferative disorders. Leukemia. 1992. 6:152–154.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download