Abstract
A heterotopic pancreas in the gastrointestinal tract is mostly found incidentally and its malignant transformation is extremely rare. We describe the second case of adenocarcinoma arising in a gastric heterotopic pancreas of an asymptomatic 35-yr-old man in Korea. Esophagogastroduodenoscopy revealed a submucosal tumor with an irregular central umbilication in the gastric antrum. A wedge resection specimen demonstrated a submucosal oligolocular cystic mass (1.7×1.4×1.2 cm) with a solid portion. Microscopically, the cystic portion was composed of dilated pancreaticobiliary type ducts with adjacent small foci of periductal glandular structures. The adenocarcinoma components in the solid area infiltrated the proper muscle and the overlying mucosa of the stomach. The transitional area between the benign ductal structures and the adenocarcinoma component was found. The follow-up course was uneventful 5 months postoperatively.
The heterotopic pancreas is defined as a pancreatic tissue found outside the eutopic pancreas without anatomic or vascular connections between them. It is not uncommon with an incidence of approximately 0.5-13.7% in autopsy studies and 0.5% in upper abdominal laparotomies (1). It can be found anywhere in the gastrointestinal tract and the predilection site is the stomach, mostly in the antrum and prepyloric region on the greater curvature or posterior wall. Unusual sites include the Meckel's diverticulum (2), the common bile duct, the gallbladder (3), the papilla, the umbilicus (4), the mesocolon (5), and the mesenteric tissue. The heterotopic pancreas is asymptomatic in general and is usually found incidentally, however, mass-like manifestations causing pyloric obstruction, ulcer, and bleeding can be observed in the gastric area.
Although a heterotopic pancreas may demonstrate most of the pathologic changes seen in the eutopic pancreas, such as acute and chronic pancreatitis (3), a pseudocyst (6), an abscess (7), and an exocrine or endocrine neoplasm (8), an adenocarcinoma arising in a gastric heterotopic pancreas is extremely rare with less than twenty cases reported in the literature (1, 9-14).
We describe the second case of adenocarcinoma arising in a gastric heterotopic pancreas in Korea (10), which occurred in an asymptomatic patient.
A 35-yr-old man who had been healthy underwent a routine medical check-up. On esophagogastroduodenoscopy (EGD), a submucosal mass with an irregular central umbilication was found in the gastric antrum (Fig. 1). The physical examination and all the laboratory findings were normal. The tumor markers including CEA (2.7 ng/mL), CA-19-9 (6.9 u/mL) and CA-72-4 (3.1 u/mL) were within normal ranges. Abdominal CT scan revealed a well-demarcated multiseptate cystic mass in the gastric antrum (Fig. 2). A wedge resection was performed under the clinical impression of gastrointestinal stromal tumor.
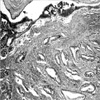
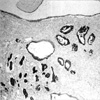
Grossly, the submucosal mass (2×1.7×1.2 cm) was composed of a whitish tan oligolocular cystic portion and a yellowish tan solid granular portion with an intact overlying mucosa. Microscopically, the cystic portion was lined by a single layer of flat, cuboidal epithelium and surrounded by smooth muscle layers (Fig. 3, arrow and Fig. 4A). Periductal glandular structures were focally identified without islet cells (Fig. 4B). In the solid area, the adenocarcinoma components forming well-formed tubules (Fig. 5) infiltrated the underlying proper muscle layer and the overlying mucosa of the stomach. Lymphovascular tumor emboli were frequently seen in areas adjacent to the adenocarcinoma components. A dysplastic change was found in the epithelium of the cystic portion of the heterotopic pancreas, adjacent to the invasive adenocarcinoma (Fig. 5). The neoplastic cells and the heterotopic pancreas tissue showed diffusely strong positivity for cytokeratin 7 (CK7+, 1:200, DAKO, Denmark) and negativity for cytokeratin 20 (CK20-, 1:200, DAKO, Denmark) by immunohistochemical stainings (Fig. 6). The overlying gastric mucosa showed CK7+ only in mucous neck cells and CK20+ in foveolar epithelial cells. The subsequent distal gastrectomy specimen revealed no residual tumor. Lymph node metastasis was not identified. The follow-up course was uneventful 5 months postoperatively.
The heterotopic (ectopic) pancreas may contain any mixture of tissues normally found in the pancreas. Heinrich classified the heterotopic pancreas into 3 types (15): type I, all the components of the pancreas including ducts, acini, and endocrine islets; type II, ducts with acini; and type III, ducts with a few acini or dilated ducts only, so called adenomyoma. When the pancreaticobiliary-type ducts predominate, they are often surrounded by hypertrophic smooth muscle bundles. The present case belongs to the Heinrich type III (adenomyoma) showing predominant dilated pancreaticobiliary-type ducts with periductal glandular structures and surrounding smooth muscle bundles.
The heterotopic pancreas is usually small, measuring 3 cm or less in diameter, however, the gastric lesions tend to be larger than those in other sites. The classic radiologic and endoscopic appearances are well-circumscribed intramural nodules with a central umbilication, which may be the site of ductal drainage to the mucosal surface. The umbilication is observed less than half of cases, therefore, other intramural masses such as gastrointestinal stromal tumor or even metastatic carcinoma must be differentiated.
For histologic diagnosis of a carcinoma arising in a heterotopic pancreas, 3 criteria have been proposed in the literature (13). Firstly, the carcinoma must be found within or close to the heterotopic pancreas. Secondly, the transitional area between pancreatic structures and carcinoma must be observed and a metastatic carcinoma or extension of carcinoma from the adjacent gastrointestinal tract must be excluded. Thirdly, the non-neoplastic heterotopic pancreatic tissue must comprise at least fully developed acini or ductal structures. The present case meets the above three criteria. In addition, the identical CK7+/CK20- phenotype in both tumor cells and non-neoplastic ductal epithelium in the heterotopic pancreas corresponds to the result of the study by Duval et al. (14), which showed the CK7+/CK20- phenotype in about 96% carcinomas of the pancreas.
The clinical course of gastric heterotopic pancreas is generally uneventful. Asymptomatic lesions of less than 2 cm in size can be followed without specific therapy. However, the clinical symptoms such as weight loss, nausea, and vomiting should raise a suspicion of malignant transformation, which may occur even without any clinical symptoms as in the present case. Therefore, a gastric heterotopic pancreas with clinical symptoms or a lesion larger than 3 cm in size regardless of the symptoms should be treated with surgical resection with histologic diagnosis. For asymptomatic small lesions less than 2 cm in size, only local resection can be considered, although histologic confirmation is required at the operation field by frozen section to decide the extent of surgery. The clinical course of adenocarcinomas arising in a gastric heterotopic pancreas has not been well documented because of the small number of reported cases, however, the same treatment modality as that for a primary gastric carcinoma is being considered (16).
The early diagnosis of malignant transformation in the gastric heterotopic pancreas may be difficult by endoscopic biopsy because of the intramural location of the mass and the delayed involvement of the overlying mucosa. Thus, a clinicoradiologic correlation and a high index of suspicion are needed in cases having a solid portion or even in an asymptomatic patient and histologic confirmation through surgical resection are required to detect malignant transformation in the gastric heterotopic pancreas as in the present case.
Figures and Tables
Fig. 1
The EGD shows a submucosal tumor with an irregular central umbilication in the gastric antrum.
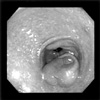
Fig. 2
The abdominal CT reveals a well-demarcated multiseptate cystic mass (arrows) in the gastric antrum.

Fig. 3
The submucosal mass consists of oligolocular cystic (arrows) and solid areas without overlying mucosal change (H&E stain, ×10).

Fig. 4
The cystic area (arrows in Fig. 3) shows dilated benign ductal structures lined by cuboidal epithelium (A, H&E stain, ×200) and focal periductal glandular structures without islet cell islands (B, H&E stain, ×100).

References
1. Herold G, Kraft K. Adenocarcinoma arising from ectopic gastric pancreas: two case reports with a review of the literature. Z Gastroenterol. 1995. 33:260–264.
2. St-Vil D, Brandt ML, Panic S, Bensoussan AL, Blanchard H. Meckel's diverticulum in children: a 20-year review. J Pediatr Surg. 1991. 26:1289–1292.

3. Qizilbash AH. Acute pancreatitis occurring in heterotopic pancreatic tissue in the gallbladder. Can J Surg. 1976. 19:413–414.
4. Caberwal D, Kogan SJ, Levitt SB. Ectopic pancreas presenting as an umbilical mass. J Pediatr Surg. 1977. 12:593–599.

5. Ishikawa O, Ishiguro S, Ohhigashi H, Sasaki Y, Yasuda T, Imaoka S, Iwanaga T, Nakaizumi A, Fujita M, Wada A. Solid and papillary neoplasm arising from an ectopic pancreas in the mesocolon. Am J Gastroenterol. 1991. 85:597–601.
6. Kakizaki Y, Ishiwatari Z, Hukushi K. A case of submucosal cyst of the stomach originating in the heterotopic pancreas. Stomach Intestine. 1975. 10:1651–1657.
7. Kaneda M, Yano T, Yamamoto T, Suzuki T, Fujimori K, Itoh H, Mizumoto R. Ectopic pancreas in the stomach presenting as an inflammatory abdominal mass. Am J Gastroenterol. 1989. 84:663–666.
8. Makhlouf HR, Almeida JL, Sobin LH. Carcinoma in jejunal pancreatic heterotopia. Arch Pathol Lab Med. 1999. 123:707–711.

9. Jeng KS, Yang KC, Kuo SHF. Malignant degeneration of heterotopic pancreas. Gastrointest Endosc. 1991. 37:196–198.

10. Ahn YS, Cho JS, Shin KS, Noh SM, Jeong HY, Song KS. Ductal adenocarcinoma arising from heterotopic pancreas in the stomach; a case report. J Korean Radiol Soc. 2001. 45:51–53.

11. Chapple CR, Muller S, Newman J. Gastric adenocarcinoma associated with adenomyoma of the stomach. Postgrad Med J. 1998. 64:801–803.

12. Kneafsey PD, Demetrick DJ. Malignant transformation in a pyloric adenomyoma: a case report. Histopathology. 1992. 20:433–435.

13. Osanai M, Miyokawa N, Tamaki T, Yonekawa M, Kawamura A, Sawada N. Adenocarcinoma arising in gastric heterotopic pancreas: clinicopathological and immunohistochemical study with genetic analysis of a case. Pathol Int. 2001. 51:549–554.

14. Duval JV, Savas L, Banner BF. Expression of cytokeratin 7 and 20 in carcinomas of the extrahepatic biliary tract, pancreas, and gallbladder. Arch Pathol Lab Med. 2000. 124:1196–1200.
15. von Heinrich H. Ein Beitrag zur Histologie des sogen: Akzessorischen Pankreas. Virchows Arch A Pathol Anat Histopathol. 1909. 198:392–401.
16. Hickman DM, Frey CF, Carson JW. Adenocarcinoma arising in gastric heterotopic pancreas. West J Med. 1981. 135:57–62.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download