Non-cardiac chest pain is a type of angina with a non-cardiac origin that 23% of the population in the United States suffers from [1] which mainly occurs due to physical and psychological problems [2]. While physical factors such as lung and musculoskeletal diseases justify a significant portion of these pains, in 66% of cases it cannot be attributed to any physical cause [3]. In particular, psychological problems are considered the cause of pain in 41% of cases [4], however, the affection mechanism of psychological factors is not well known. Previous studies have addressed the role of factors such as stress, anxiety, depression, and personality type [56] and this issue has led to the neglect of other possible factors. Irrational beliefs in patients with non-cardiac chest pain, as a cognition factor, have received more attention during recent years compared with other factors [23]. Irrational beliefs, negative automatic thoughts, and tendency to a disastrous interpretion of bodily sensations in patients with non-cardiac chest pain [3] lead these patients continue to incorrectly interpret the cause of their pain despite the absence of cardiovascular problems [2] and subsequently suffer from pervasive distress. Discomfort and distress caused by pain in these patients is an annoying condition [1]. Identification of the cause can be effective in improving their quality of life and reduce visits to the emergency department.
Based on these considerations, a study was conducted to investigate the predictive role of irrational beliefs for pain/discomfort among patients with non-cardiac chest pain. During August to November 2014, 93 patients with non-cardiac chest pain and normal coronary angiography (37-76 years, mean and standard deviation of 52.3 ± 9.1 years) were invited to participate in the study after angiography at Imam Ali hospital in Kermanshah city (in western Iran). According to the formula (N > 50 + 8 m) which is used to determine the sample size in regression analysis, the sample size for this study must be at least 82 people [7]. Thus, the number of 93 cases was suitable. After written informed consent to participate in the study was given, demographic data and medical records of the patients were evaluated and recorded by a cardiologist. Then, an Iranian version of the Jones Irrational Beliefs Questionnaire [8] and the pain discomfort scale of Jensen et al. [9], as appropriate validated scales, were delivered to the patients by a clinical psychologist, and the patients, after receiving the necessary explanations, completed the forms. The psychologist read the items for the illiterate patients and recorded the patients' responses. Descriptive and inferential statistics and linear regression analysis were used to evaluate the linear relationship between irrational beliefs and pain/discomfort and the predictive role of irrational beliefs in the severity of pain/discomfort. All statistical analyzes were performed using SPSS 20 software.
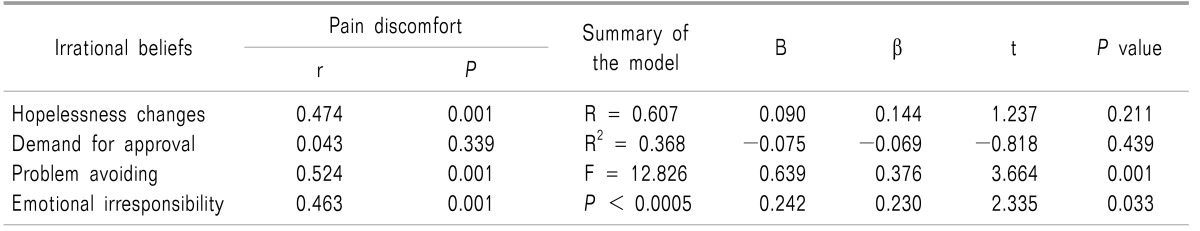
According to the findings, 69.9% of the patients were female. In terms of job status, 66.6% of the patients were housewives, 15.1% were self-employed, 6.8% were employees, and 7.9% were retired. In terms of education, 43% had no diploma, 54.8% had a high school diploma, and 2.2% had a college education. In relation to the main analysis, the correlation between four types of irrational belief and pain/discomfort can be seen in Table 1. As you can see, there is a significant relationship between the hopelessness in the face of change (P < 0.001), problem avoidance (P < 0.001), and emotional irresponsibility beliefs (P < 0.001) with pain/discomfort. But, there is no significant relationship between need of or demand for approval and pain/discomfort (P > 0.05). Of course, given that the P value is significant in the regression model only to problem avoidance (β = 3.664, P < 0.001) and emotional irresponsibility (β = 2.335, P = 0.033), it can be suggested that responsibility is the most predictive factor among these two variables. In fact, avoiding the problem and emotional irresponsibility respectively are the strongest predictors of pain discomfort. However, the model summary shows that irrational beliefs significantly can predict pain/discomfort (F = 12.826, P < 0.0005) and in general can express 36.8% of the pain/discomfort variance.
Our results showed that these irrational beliefs are important factors in pain/discomfort experienced by patients with non-cardiac chest pain. In this respect, Bahremand and colleagues [3] found that patients with severe non-cardiac chest pain, compared with patients with mild pain, present more irrational beliefs. It seems that as those with irrational beliefs aren't looking for synchronization and coordination with reality, this leads to stressful conditions and increased negative behavior and performance, and discomfort/pain [3]. So, when a patient shows signs of physical discomfort such as non-cardiac chest pain, health professionals should consider irrational beliefs as a cognition factor affecting the pain/discomfort and distress caused by it [234].
References
1. Bahremand M, Saeidi M, Komasi S. How effective is the use of metaphor therapy on reducing psychological symptoms and pain discomfort in patients with non-cardiac chest pain: a randomized, controlled trial. J Cardiothorac Med. 2016; 4:444–449.
2. Bahremand M, Moradi G, Saeidi M, Mohammadi S, Komasi S. Reducing irrational beliefs and pain severity in patients suffering from non-cardiac chest pain (NCCP): a comparison of relaxation training and metaphor therapy. Korean J Pain. 2015; 28:88–95. PMID: 25852829.

3. Bahremand M, Saeidi M, Komasi S. Non-coronary patients with severe chest pain show more irrational beliefs compared to patients with mild pain. Korean J Fam Med. 2015; 36:180–185. PMID: 26217482.

4. Bahremand M, Saeidi M, Takallo F, Komasi S. Comparison of depression, anxiety, and stress between mild and severe non-cardiac chest pain. Thrita. 2016; 5:e32752.

5. Kuijpers PM, Denollet J, Wellens HJ, Crijns HM, Honig A. Noncardiac chest pain in the emergency department: the role of cardiac history, anxiety or depression and Type D personality. Eur J Cardiovasc Prev Rehabil. 2007; 14:273–279. PMID: 17446807.

6. Mourad G, Jaarsma T, Hallert C, Strömberg A. Depressive symptoms and healthcare utilization in patients with noncardiac chest pain compared to patients with ischemic heart disease. Heart Lung. 2012; 41:446–455. PMID: 22652167.

7. Pallant J. SPSS survival manual: a step by step guide to data analysis using SPSS for Windows (version 12). 2nd ed. Maidenhead: Open University Press;2005. p. 142–152.
8. Ebadi GH, Motamedin M. The study of factor structure of Jones's irrational beliefs test. Knowl Res Psychol. 2005; 23:73–92.
9. Jensen MP, Karoly P, Harris P. Assessing the affective component of chronic pain: development of the Pain Discomfort Scale. J Psychosom Res. 1991; 35:149–154. PMID: 2046049.





 Citation
Citation Print
Print


 XML Download
XML Download