Abstract
A 64-year-old woman visited our pain clinic with the pain of right lateral side of thigh for one year. Her pain always started from knee and was radiated to buttock area when symptom was severe. She showed significant tenderness at knee lateral side and local tightness at lateral thigh. Magnetic resonance image of the knee was performed and we could identify high signal intensity of iliotibial band through coronal and axial view. In spite of medication and physical stretching exercise of iliotibial band for one month, she did not show any improvement of pain. To alleviate her symptom, ultrasound guided local corticosteroid injection targeting beneath the iliotibial band was performed. After the procedure, the reduction of pain was significant and there was no need for further management.
Iliotibial band (ITB) syndrome is a overuse injury usually observed in active athletic population. Most of affected patients complain lateral side knee pain associated with repetitive activities. Based on characteristic history and physical examination, we can diagnose ITB syndrome. Magnetic resonance image study and ultrasound examination are reserved for refractory cases to rule out other pathologic diseases [1,2]. ITB syndrome is known as the common cause of lateral knee pain among runners and cyclists, with a reported incidence ranging from 1.6% to 12% [1,3].
The etiology of ITB syndrome is a matter of controversial and it seems that different subtypes of ITB syndrome exist. They include friction of ITB against the lateral femoral epicondyle during repetitive flexion and extension, compression of the fat and connective tissue deep to the ITB, and chronic inflammation of the ITB bursa. There is less evidence that a pathologic change takes place in the ITB itself [1,2,4].
The mainstay of treatment is the nonsurgical approach for symptom improvement of ITB syndrome. Oral nonsteroidal anti-inflammatory drugs and corticosteroid injection can be used to treat the acute inflammatory response [1,3,5]. Although, Corticosteroid injections compared to placebo injections have shown significant pain improvement [6], there are few studies showing corticosterioid injection by the ultrasound guidance. Therefore, we present one patient with lateral side thigh pain who was diagnosed as ITB syndrome after magnetic resonance imaging evaluation and was treated successfully with corticosteroid injection by the ultrasound guidance. We would like to present the diagnostic feature of ITB syndrome and suggest the ideal location if the corticosteroid injection is performed by the ultrasound guidance.
A 64-year-old woman came to our pain clinic with the symptom of right lateral side thigh pain which occurred from one year ago. Her pain started from knee lateral side and the pain was radiated to buttock area. When she started to walk, the pain was triggered and whenever symptoms aggravated, she could feel the tingling sensation through a whole leg which made her limping. She described her pain as pin pricking or stabbing with her pain severitiy 7-8/10 on the visual analogue scale (VAS).
Before she felt the lateral leg pain, she had the lipoma removing surgery around the lower knee. However, we did not think it is the main problem causing the symptom.
Although her pain always started from knee lateral side, ultimately she could feel severe pain coming from entire thigh. Therefore, we performed straight leg raising and Patrick test to rule out any spine and pelvic problem. She was negative to all these tests and did not show any local tenderness around back or buttock. However, we could check significant local tenderness on right lateral side of knee. Also we performed knee instability test on both side which showed no abnormality. She showed local tightness around the lateral side of thigh compared to nonpainful side.
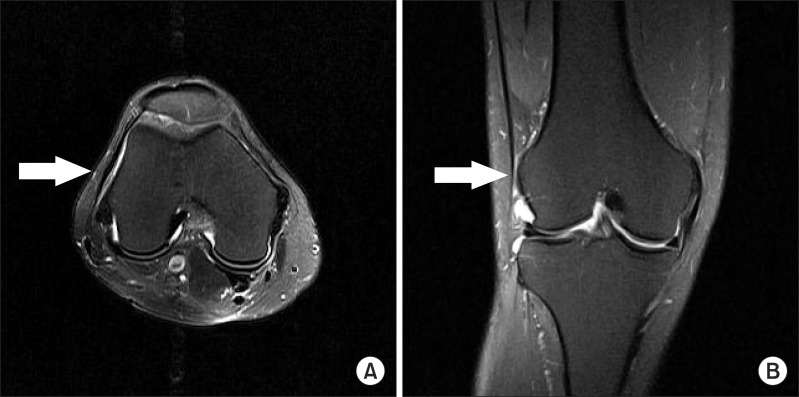
As the pain always started from the knee and aggravated by walking, we suspected some pathologic changes from inside the knee like meniscus or cruciate ligament. We decided to evaluate knee magnetic resonance imaging (MRI) study and simple X-ray. Her MRI study showed slight degenerative change on meniscus which seemed to be unrelated to the current pain. However, we could identify high signal intensity appearing at ITB through coronal and axial image (Fig. 1). We assessed that ITB syndrome is causing the pain.
To alleviate her symptom, we prescribed 37.5 mg tramadol/375 mg acetaminophen combination tablet (Paramacet tab: Donga, Seoul, Korea), 5 mg amitriptyline per os twice daily but had little effect. We educated her about the ITB specific stretching exercise which was known to improve the symptom by lengthening of the ITB. She continued to perform this stretching exercise for a month but the pain relief was not satisfactory.
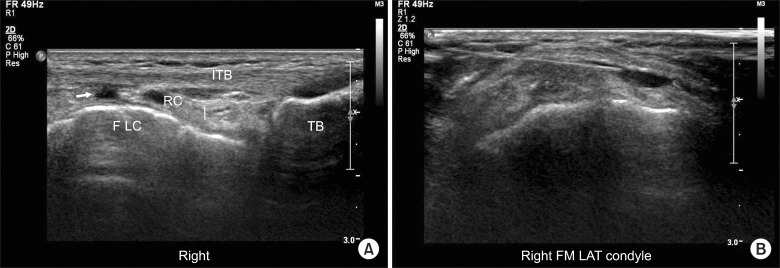
To improve her symptom, we planned local corticosteroid injection by ultrasound guidance. We explained about the procedure, efficacy, and possible side effects of local corticosteroid injection. The skin was aseptically draped with betadine and the ultrasound transducer was covered with a sterile transparent sheath and aseptic gel. We used a 10-12 MHz linear transducer (IU 22, Philips, Netherlands). First, we marked the maximal tenderness area and the transducer was applied longitudinally to the lateral side of the knee. We could easily identify the ITB, femoral lateral condyle, tibia, and recess. Also we could find the local fluid collection under the ITB (Fig. 2A) which should not appear normally. Before injection, we checked whether the transducer was covering the maximal tenderness area. We targeted the needle tip beneath the iliotibial band and confirmed its location by injecting small amount of saline (Fig. 2B). We payed close attention not to inject the medication into ITB itself. Following negative aspiration, 1% lidocaine 1ml and triamcinolone 20 mg was injected.
After one week, the patient was followed up and she was fully recovered from previous pain. She told us that she never felt any kind of pain after injection. One month later, she was followed up again and she could not feel any pain around knee and thigh.
ITB syndrome causes pain in the area of the lateral femoral epicondyle or slightly below to it, which occurs after repetitive flexion and extension of the knee, typically in a runner, cyclist, or other athlete. An important finding of physical examination is local tenderness of the lateral knee below to the epicondyle and superior to the joint line. Three provocative tests are availiable for the assessment of ITB. The noble test is performed with the patient lying supine; beginning with the affected knee flexed at 90°, the leg is extended with direct pressure over the lateral femoral epicondyle, with reproducible pain near 30° of knee flexion. The ober test for distensibility of the ITB is most commonly used to assess tightness of the ITB. The Thomas test is used to check the tightness of iliopsoas muscle, rectus femoris muscle, and ITB [1,5].
The differential diagnosis includes lateral meniscus tear, lateral compartment degenerative joint disease, biceps femoris tendinopathy, stress fracture, patellofemoral syndrome and lateral collateral ligament pathology [1].
Most of patients diagnosed as ITB syndrome typically present symptoms localized to lateral side of the knee. However, the pain is not always localized to the lateral side of knee in which case our patient has shown, therefore, the diagnosis can be challenging in some cases. Before she came to our pain clinic, she visited several other local clinics and has been heard that the thigh pain is coming from the spine disease like disc herniation or spinal stenosis. She has got spine injections several times with no improvement. As the thigh pain is aggravated by walking or repetitive exercice, it can be considered as neurogenic intermittent claudication which is observed in spinal stenosis. The patients of ITB syndrome can possibly complain thigh pain when we think the anatomical orientation of ITB. The ITB is a lateral thickening of the fascia latae of the thigh. The ITB is formed proximally at the level of the greater trochanter as a coalescence of the tensor fascia latae and the gluteus maximus and medius muscles. Anatomic reports have demonstrated that the ITB is a dense fibrous connective tissue that passes distally along the thigh [7-9]. Proximal to the knee joint, the ITB has attachments to the intermuscular septum and the supracondylar tubercle of the femur. It continues inferiorly to insert on the Gerdy tubercle at the anterolateral side of the tibia [8,9]. The contact is formed at the level of the lateral femoral condyle between the ITB and the underlying epicondyle and origin of the lateral collateral ligament, helping provide lateral stability to the knee joint [1,8,9].
The proposed etiology of ITB syndrome is multifactorial [1,3]. Most of ITB syndrome is a nontraumatic overuse injury which is caused by friction and rubbing of the distal portion of the ITB over the lateral femoral epicondyle [1,3,5]. Orchard et al. [10] proposed that an impingement zone occurs near 30° of knee flexion during foot strike and early stance phase. The ITB passes over and posterior to the lateral femoral epicondyle at approximately 30° and greater of knee flexion. While this impingement happens, eccentric contraction of the tensor fascia lata and gluteus maximus is formed to exert great tension through the ITB. The pathogenesis of ITB syndrome involves inflammatory process and irritation of the posterior fibers of ITB and lateral synovial recess [3,5].
In cases of refractory ITB syndrome, MRI can be used as a diagnostic tool. ITB syndrome can be diagnosed with the appearance of high-intensity signal on T2 weighted image which appears over the lateral epicondyle deep to the ITB, and marked thickening of the distal ITB [3,11]. Ultrasonography can also be used as a diagnostic tool and it demonstrates thickening of ITB in case of patients. The normal thickness of healthy volunteers is around 1.1 ± 0.2 mm [1,12]. Monitoring the thickness of ITB might be a useful variable in the diagnosis of ITB syndrome, moreover, to evaluate the evolution of this condition.
Nonsurgical management is the mainstay of treatment for symptom improvement. Oral nonsteroidal anti-inflammatory drugs and corticosteroid injections can be used to reduce the acute inflammatory response [1]. Gunter and Schwellnus [6] reported that local corticosteroid infiltration around ITB (1 ml 1% lidocaine plus 40 mg methylprednisolone) compared with control group effectively decreased pain during running in the first two weeks of treatment in patients with recent onset ITB syndrome. However, they performed the injection by blind technique after identifying the maximal tenderness area. Therefore, their report does not suggest any ideal location for corticosteroid injection.
For symptom improvement of our patient, we decided to use the ultrasound guidance for the injection of ITB. The main benefit of ultrasound guidance during corticosteroid injection is the ability to identify vascular structures and nerves located in the needle pathway in order to avoid these structures and be sure to inject the medication into the most optimal location [13]. Ultrasonography enables real time examination, which promotes dynamic evaluation of various tendons, and continuous monitoring during any type of injection. In contrast to the fluoroscopy, ultrasound does not produce any harmful reaction to both physician and patient. Moreover, ultrasound guided accurate injection can result in significantly greater clinical improvement in pain and function over blind (landmark guided) injections [14].
For corticosteroid injection, initially, we identified several anatomical structure including the ITB, lateral synovial recess and femoral epidcondyle. We targeted the potential space between the ITB and overlying lateral femoral epicondyle because most of inflammatory and irritation process occurs here.
The injection was successfully performed at this site without any event and the patient showed excellent recovery from pain. If the ultrasound guided corticosteroid injection of ITB should be performed, we suggest that our method can be a useful option.
References
1. Strauss EJ, Kim S, Calcei JG, Park D. Iliotibial band syndrome: evaluation and management. J Am Acad Orthop Surg. 2011; 19:728–736. PMID: 22134205.

2. van der Worp MP, van der Horst N, de Wijer A, Backx FJ, Nijhuis-van der Sanden MW. Iliotibial band syndrome in runners: a systematic review. Sports Med. 2012; 42:969–992. PMID: 22994651.
3. Ellis R, Hing W, Reid D. Iliotibial band friction syndrome--a systematic review. Man Ther. 2007; 12:200–208. PMID: 17208506.

4. Meardon SA, Campbell S, Derrick TR. Step width alters iliotibial band strain during running. Sports Biomech. 2012; 11:464–472. PMID: 23259236.

5. Lavine R. Iliotibial band friction syndrome. Curr Rev Musculoskelet Med. 2010; 3:18–22. PMID: 21063495.

6. Gunter P, Schwellnus MP. Local corticosteroid injection in iliotibial band friction syndrome in runners: a randomised controlled trial. Br J Sports Med. 2004; 38:269–272. PMID: 15155424.

7. Muhle C, Ahn JM, Yeh L, Bergman GA, Boutin RD, Schweitzer M, et al. Iliotibial band friction syndrome: MR imaging findings in 16 patients and MR arthrographic study of six cadaveric knees. Radiology. 1999; 212:103–110. PMID: 10405728.

8. Vieira EL, Vieira EA, da Silva RT, Berlfein PA, Abdalla RJ, Cohen M. An anatomic study of the iliotibial tract. Arthroscopy. 2007; 23:269–274. PMID: 17349469.

9. Fairclough J, Hayashi K, Toumi H, Lyons K, Bydder G, Phillips N, et al. The functional anatomy of the iliotibial band during flexion and extension of the knee: implications for understanding iliotibial band syndrome. J Anat. 2006; 208:309–316. PMID: 16533314.

10. Orchard JW, Fricker PA, Abud AT, Mason BR. Biomechanics of iliotibial band friction syndrome in runners. Am J Sports Med. 1996; 24:375–379. PMID: 8734891.

11. Vasilevska V, Szeimies U, Stäbler A. Magnetic resonance imaging signs of iliotibial band friction in patients with isolated medial compartment osteoarthritis of the knee. Skeletal Radiol. 2009; 38:871–875. PMID: 19484234.

12. Gyaran IA, Spiezia F, Hudson Z, Maffulli N. Sonographic measurement of iliotibial band thickness: an observational study in healthy adult volunteers. Knee Surg Sports Traumatol Arthrosc. 2011; 19:458–461. PMID: 20890700.

13. Molini L, Mariacher S, Bianchi S. US guided corticosteroid injection into the subacromial-subdeltoid bursa: technique and approach. J Ultrasound. 2012; 15:61–68. PMID: 23396761.

14. Soh E, Li W, Ong KO, Chen W, Bautista D. Image-guided versus blind corticosteroid injections in adults with shoulder pain: a systematic review. BMC Musculoskelet Disord. 2011; 12:137. PMID: 21702969.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download