Abstract
Vertebroplasty (VP) can effectively treat pain and immobility caused by vertebral compression fracture. Because of complications such as extravasation of bone cement (polymethylmethacrylate, PMMA) and adjacent vertebral fractures, some practitioners prefer to inject a small volume of PMMA. In that case, however, insufficient augmentation or a subsequent refracture of the treated vertebrae can occur. A 65-year-old woman visited our clinic complaining of unrelieved severe low back and bilateral flank pain even after she had undergone VP on the 1st and 4th (L1 and L4) lumbar vertebrae a month earlier. Radiologic findings showed the refracture of L1. We successfully performed the repeat VP by filling the vertebra with a sufficient volume of PMMA, and no complications occurred. The patient's pain and immobility resolved completely three days after the procedure and she remained symptom-free a month later. In conclusion, VP with small volume cement impaction may fail to relieve fracture-induced symptoms, and the refracture of an augmented vertebral body may occur. In this case, repeat VP can effectively resolve both the persistent symptoms and problems of new onset resulting from refracture of the augmented vertebral body due to insufficient volume of bone cement.
Vertebral compression fractures (VCFs) cause severe pain and spinal instability, devastating patients' quality of life [1]. Vertebroplasty (VP) is a very effective treatment modality that lessens fracture-induced pain and spinal instability, and enables patients to return to their normal activities [2,3]. However, VP can result in complications such as direct nerve damage, pulmonary embolism, and adjacent vertebral fractures [4,5].
Adjacent fractures are particularly bothersome for practitioners because they can occur even after a successful procedure. Adjacent fractures are thought to be caused by an excessive increase in the rigidity of augmented vertebrae [6], and some doctors insist that injecting only a small volume of bone cement (polymethylmethacrylate, PMMA) can prevent adjacent fractures. However, there is not yet a consensus on the optimal volume of PMMA to inject. Furthermore, a volume of injected cement that is too small can be ineffective in controlling pain, and refracture of the augmented vertebra can occur.
In our practice, we encountered a patient with persistent pain and immobility after VP and subsequent refracture of the treated vertebral body. We performed an additional VP with sufficient PMMA to fill the fractured area, which resulted in significant pain relief and resolution of the patient's immobility. We present this case here, along with a review of the literature.
A 65-year-old female presented to our pain clinic complaining of low back pain. A month earlier she had experienced pain in the low back and right flank area, and was diagnosed with osteoporotic VCF in the first and fourth lumbar vertebral bodies (L1 and L4). Unipedicular VPs were performed with the injection of 2 ml and 2.5 ml of PMMA into each vertebra, respectively (Fig. 1). After the procedure, the visual analogue scale (VAS) reduced from 10 to 8, and her flank pain subsided. This state continued without additional pain relief.
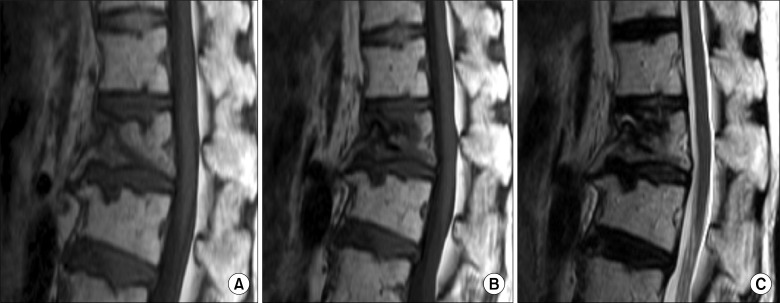
Several days before her visit to our clinic, the patient's back pain worsened and became aggravated when sitting, standing up, or changing her posture (VAS 10). She was also unable to stand or walk unassisted. On physical examination, only tenderness of the L1 spinous process was present and there were no neurological abnormalities. An interval progression of anterior wedging in the L1 vertebral body was detected on lumbar plain radiograph, and MR images showed findings consistent with the refracture of L1 (Fig. 2). Based on these results, we concluded that the previous VP in L1 had failed to relieve her pain and that refracture of L1 worsened the symptoms. We therefore proceeded to repeat VP in the L1 vertebra.
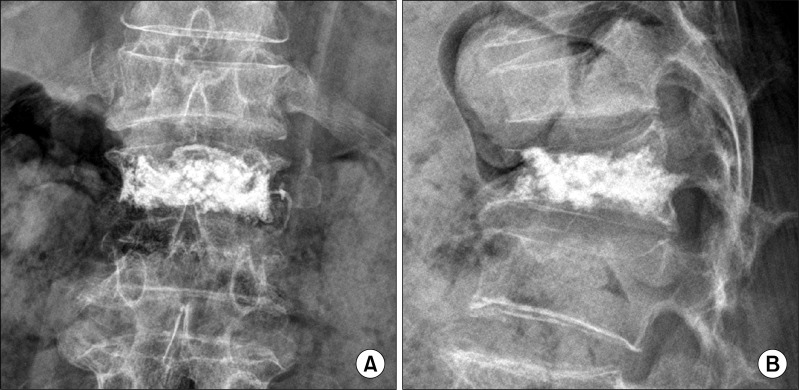
After obtaining informed consent from the patient and her family, repeat VP was performed in the L1 vertebral body using a bipedicular approach with the patient in the prone position. When the bone fillers reached the fractured cavity of the L1 vertebral body, we then slowly injected 3.5 ml of PMMA bone cement on each side under real-time C-arm fluoroscopic guidance to prevent cement leakage and to ensure even dispersion of cement in the fractured lesion (Fig. 3). No cement leakage or dislocation of the previous injectate was detected. During the VP procedure, blood pressure, EKG, and mixed venous oxygen saturation were monitored, and oxygen was supplied via nasal cannula. In addition, a total of 100 mcg fentanyl was administered intravenously for analgesia.
The day after the procedure, the patient's VAS dropped from 10 to 4, and she reported only discomfort in the procedure area. She was also able to walk unassisted, and was therefore discharged on that day. When she visited our clinic a month after the repeat VP, her pain and immobility had resolved completely.
VP is effective for managing pain and immobility caused by vertebral compression fractures. However, pain can recur in 1.8-15.6% of patients after VP, which is attributable to rib fracture, infection, non-healing bone-cement interface, or new symptomatic compression fractures [7]. In addition, inadequate impactions of bone cement can make the unfilled intravertebral spaces collapse or the injectates loosen after procedures [6].
Currently, there is no consensus on the adequate volume of bone cement to inject during VP. Some practitioners prefer to inject a small volume of bone cement. Belkoff et al. reported that 2 ml of bone cement is enough to recover the strength of fractured vertebrae [8]. In a biomechanical study using cadavers, a small volume of injected bone cement normalized the distribution of compressive stress on the fractured and adjacent vertebrae [9]. Other researchers have also reported finding no correlation between the injected cement volume and the degree of pain relief [10,11]. In addition, injection of a large volume of PMMA increases the risk of adjacent fractures and cement leakage from the vertebral body, leading to complications such as epidural hemorrhage, spinal cord injury, and acute respiratory distress [4,5,10,12].
On the other hand, He et al. performed additional VPs for 15 patients whose pain persisted after VP, and commented that a sufficient volume of injected PMMA was the most important factor predicting patient prognosis [13]. Kim et al. reported that cement volume was not related to the incidence of subsequent vertebral compression fractures and recommended injecting the largest possible volume of bone cement [14].
In our case, previous VP with small volume PMMA impaction failed to relieve the patient's symptoms, and subsequent refracture of the vertebra on which the procedure was performed worsened her problems. The results of our case clearly confirmed that small volume VP can be ineffective, and the patient's pain and immobility worsened as a result of subsequent refracture to the augmented vertebra.
The optimal volume of PMMA to inject into fractured vertebrae remains controversial. In addition, further studies are needed to investigate long-term patient prognosis and the biomechanics of fractured vertebral bodies. However, in our opinion, it seems appropriate to fill fractured vertebral bodies with a sufficient volume of bone cement that is within the limits of leakage, rather than a small volume of PMMA, in order to improve the patient's prognosis.
In conclusion, VP with small volume bone cement impaction may fail to relieve fracture-induced symptoms and to prevent refracture of an augmented vertebral body. Also, in case of refracture of procedure vertebra, repeat VP can effectively treat unresolved symptoms.
References
1. Silverman SL. The clinical consequences of vertebral compression fracture. Bone. 1992; 13(Suppl 2):S27–S31. PMID: 1627411.

2. Cortet B, Cotten A, Boutry N, Flipo RM, Duquesnoy B, Chastanet P, et al. Percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fractures: an open prospective study. J Rheumatol. 1999; 26:2222–2228. PMID: 10529144.
3. Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine (Phila Pa 1976). 2000; 25:923–928. PMID: 10767803.

4. Choi Y, Han HC, Lim KJ. Pulmonary embolism after percutaneous vertebroplasty with polymethylmethacrylate: a case report. J Korean Pain Soc. 2002; 15:190–193.
5. Kim DH, Kim KH, Kim YC. Minimally invasive percutaneous spinal techniques. 2011. Pennsylvania: Elsevier;p. 259–276.
6. Lin WC, Lee YC, Lee CH, Kuo YL, Cheng YF, Lui CC, et al. Refractures in cemented vertebrae after percutaneous vertebroplasty: a retrospective analysis. Eur Spine J. 2008; 17:592–599. PMID: 18204942.

7. Lin CC, Shen WC, Lo YC, Liu YJ, Yu TC, Chen IH, et al. Recurrent pain after percutaneous vertebroplasty. AJR Am J Roentgenol. 2010; 194:1323–1329. PMID: 20410421.

8. Belkoff SM, Mathis JM, Jasper LE, Deramond H. The biomechanics of vertebroplasty. The effect of cement volume on mechanical behavior. Spine (Phila Pa 1976). 2001; 26:1537–1541. PMID: 11462082.
9. Luo J, Daines L, Charalambous A, Adams MA, Annesley-Williams DJ, Dolan P. Vertebroplasty: only small cement volumes are required to normalize stress distributions on the vertebral bodies. Spine (Phila Pa 1976). 2009; 34:2865–2873. PMID: 20010394.
10. Kaufmann TJ, Trout AT, Kallmes DF. The effects of cement volume on clinical outcomes of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2006; 27:1933–1937. PMID: 17032870.
11. Al-Ali F, Barrow T, Luke K. Vertebroplasty: what is important and what is not. AJNR Am J Neuroradiol. 2009; 30:1835–1839. PMID: 19713320.

12. Han IH, Chin DK, Kuh SU, Kim KS, Jin BH, Yoon YS, et al. Magnetic resonance imaging findings of subsequent fractures after vertebroplasty. Neurosurgery. 2009; 64:740–744. PMID: 19349832.

13. He SC, Teng GJ, Deng G, Fang W, Guo JH, Zhu GY, et al. Repeat vertebroplasty for unrelieved pain at previously treated vertebral levels with osteoporotic vertebral compression fractures. Spine (Phila Pa 1976). 2008; 33:640–647. PMID: 18344858.

14. Kim DJ, Kim TW, Park KH, Chi MP, Kim JO. The proper volume and distribution of cement augmentation on percutaneous vertebroplasty. J Korean Neurosurg Soc. 2010; 48:125–128. PMID: 20856660.

Fig. 1
AP (A) and lateral (B) radiographs showing augmented 1st and 4th lumbar vertebral bodies filled with 2 ml and 2.5 ml of PMMA, respectively. The small volume injectates were unevenly distributed into the small portion of fractured vertebrae.
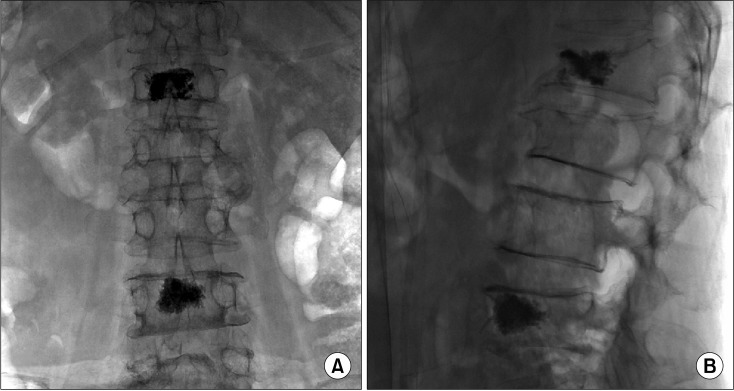
Fig. 2
In the pre-VP image (A), the collapse of vertebral body and the low-signal intensity in the anterior part of L1 represented the acute vertebral compression fractures. Comparing to the pre-VP image, the T1 and T2 weighted images a month after the first VP (B and C, respectively) showed slightly increased vertebral collapse and kyphotic angle, and an increase in low-signaled area to the posterior part of the L1 vertebral body, which are viewed as the refracture of L1.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download