Abstract
Background
Circumcision is a painful intervention frequently performed in pediatric surgery. We aim to compare the efficacy of caudal block versus dorsal penile block (DPNB) under general anesthesia for children undergoing circumcision.
Methods
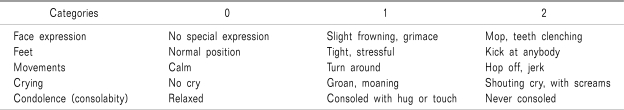
This study was performed between July 1, 2009 and October 16, 2009. Fifty male children American Society of Anesthesiolgists physical status classification I, aged between 3 and 12 were included in this randomized, prospective, comparative study. Anesthetic techniques were standardized for all children. Patients were randomized into 2 groups. Using 0.25% 0.5 ml/kg levobupivacain, we performed DPNB for Group 1 and caudal block for Group 2. Postoperative analgesia was evaluated for six hours with the Flacc Pain Scale for five categories; (F) Face, (L) Legs, (A) Activity, (C) Cry, and (C) Consolability. For every child, supplemental analgesic amounts, times, and probable local or systemic complications were recorded.
Results
No significant difference between the groups (P > 0.05) was found in mean age, body weight, anesthesia duration, FLACC pain, and sedation scores (P > 0.05). However, on subsequent measurements, a significant decrease of pain and sedation scores was noted in both the DPNB group and the caudal block group (P < 0.001). No major complication was found when using either technique.
Circumcision is a painful intervention that is frequently performed in pediatric surgery [1]. It is generally performed under general anesthesia in order to eliminate fear and anxiety [2]. Regional techniques are more effective than systemic opioids, non-steroid anti-inflammatory drugs, and acetaminophene for postoperative analgesia in circumcision [3]. The most preferred techniques are dorsal penile nerve block (DPNB) and caudal block [4].
Caudal block is a cheap, easy, and effective method used in pediatric surgery as a postoperative analgesia and as a sole anesthetic technique [5]. Another safe and effective method is DPNB [6]. For postoperative analgesic purposes, caudal block and DPNB are among many different drugs and techniques [7-9] that can be used.
In this study, we aim to compare postoperative analgesia, sedation status, and complications between caudal block and DPNB with levobupivacaine in elective circumcision cases.
This study was approved by the Institutional Review Board and informed consent was obtained from the parents. Fifty boys aged 3 to 12, American Society of Anesthesiologists physical status classification I undergoing elective day circumcision surgery participated in this prospective, comparative study. They were randomized into two groups. Patients were excluded if they had a severe systemic disease, pre-existing neurological or obvious spinal disease, bleeding diathesis, a history of seizure disorder, or a known hypersensitivity to amide-type local anaesthetics.
A 22-gauge intravenous catheter was inserted into a small vein on the dorsum of the hand in the premedication room. Isodex (3.3% dextrose + 0.3% NaCl, Eczacıbası/Baxter, Istanbul, Turkey) solution (3-5 ml/kg/h) was given intravenously, but no premedication was given. The patients were then taken to the operating room. Children were monitored with a 3 lead electrocardiogram for systolic, diastolic, mean blood pressure, heart rate and peripheral oxygene saturations (Infinity® Vista XL Patient Monitor, Drager, Lübeck, Germany). Anesthesia was delivered with an intravenous bolus of propofol 2-3 mg/kg until loss of eyelash reflex. If the intravenous catheter could not be inserted, inhalational induction was performed with a facemask using 8% sevoflurane in 50% air + 50% O2. Sevoflurane was used for maintenance. After induction, a laryngeal mask, appropriate to the children's age and weight, was put in place.
Patients were randomized by the closed-envelope technique into 2 groups. Drug solutions were prepared by another anesthetist. During anesthetic maintenance, group 1 (n = 25) received a DPNB using a 25 G needle in the supine position, with 0.25% levobupivacaine 0.5 ml/kg. This was given under the superficial fascia to the triangular hiatus (symphysis pubis, membranous layer of superficial fascia, corpus cavernous). Group 2 (n = 25) received a caudal block using a 22 G needle in the lateral decubitus position, with 0.25% levobupivacaine, 0.5 ml/kg. This was inserted into the caudal epidural space. After completion of the surgery, the children were awakened.
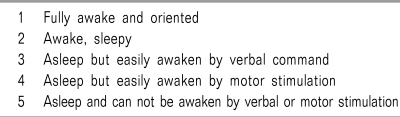
In the recovery room, all children were observed and recorded for pain, sedation, and side effects (nausea, vomit, agitation, penile hematoma, bleeding, motor block, urinary retention) at 5, 15, and 30 minutes. Then, the children were transferred to wards. They were observed and recorded for the same parameters at 1, 3, and 6 hours. The first analgesic demand time was measured from the time the DPNB and caudal block were applied to the first dose of tramadol. Probable local or systemic complications were recorded. For follow-up of postoperative pain, the FLACC Pain Scale [10] (FLACC: A behavioral scale for scoring postoperative pain in young children) (Table 1) was used, and, for the sedation follow-up, the Ramsey sedation scale [11,12] (Table 2) was used. If the FLACC pain score was 5 or over, 1 mg/kg of intravenous tramadol (Contromal®, Abdi İbrahim, Istanbul, Turkey) as a supplemental analgesic was administered postoperatively and recorded. In the 12-hours period after discharge from the hospital, the children's parents or guardians were questioned by telephone about any postoperative pain, adverse events, nausea, vomiting, pruritus, or urinary retention.
A power analysis was performed using the NCSSPASS 2007 packet program. It is found that Power = 0.93. The SPSS 12.0 software program was used for statistical analysis. Data are given as mean ± standard deviation. The Mann-Whitney U test was used to compare the two groups. The Friedman test was performed for repeated measurements at consecutive time intervals.
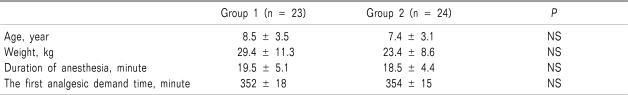
The study included 50 boys undergoing circumcision. Two patients in group 1 and 1 patient in group 2 were excluded from the study. The remaining 47 patients were divided into group 1 (n = 23) and group 2 (n = 24). No significant differences existed between the groups with respect to age, weight, or duration of anesthesia (Table 3).
On evaluation of the FLACC pain scores at different time intervals within groups, a significant decrease in pain scores was found. However, a comparison of FLACC pain score measurements of the two different groups at all the time intervals revealed no significant variation (Fig. 1).
Patients of both groups had similar pain scores. No opioid was used in either group, intraoperatively. Three patients were excluded from the study because they needed extra analgesic immediately at the beginning of the postoperative period. Therefore their blocks were considered as unsuccessful. The first analgesic demand time of the groups was 352 ± 18 min for group 1 and 354 ± 15 min for group 2. There was no statistically significant difference for the first analgesic demand time between group1 and group 2.
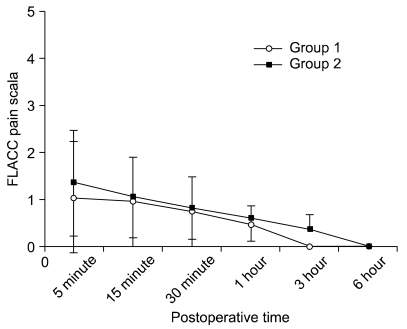
An in-Group comparison of Ramsey sedation scores versus time revealed that sedation scores decreased significantly over time. Comparing the measurements at all time intervals found no significant difference between the groups (Fig. 2).
No major complication (arrhythmia, hypotension, shock, or seizures) after DPNB or caudal block was noted. In group 1, blood was aspirated in one patient before local anesthetic injection and minor bleeding was detected in another patient from the injection site. No edema, hematoma, postoperative agitation, motor block, or urinary retention were seen in either group. Nausea-vomit was seen only in 2 patients of group 2. No severe bleeding occurred during surgery. During the telephone follow-up, parents reported no need for any extra analgesics and no adverse events.
In this study, we compared the efficacy of DPNB and caudal block with levobupivacain for circumcision cases under general anesthesia. Postoperative analgesic efficacy and supplementary analgesic needs of DPNB and caudal block were found to be similar. Ideal method of postoperative analgesia after circumcision requires very low complication rates and high success rates. In the literature, the studies mostly compared penile block with different techniques and non-invasive methods [2,13]. No prospective randomized study comparing DPNB and caudal blocks in children exist [1].
DPNB is sometimes used as a sole anesthetic technique for circumcision and sometimes used in conjunction with a general anesthesia. Penile block is a safe, easy, and effective intervention used to reduce postoperative pain. At the same time, it reduces the adrenocortical stress response and behavioural distress. After successful blocks, postoperative analgesia can be provided for up to 12 hours. Possible affirmative effects include a faster recovery, earlier micturition, and earlier discharge from the hospital [3,8].
In this study, we used levobupivacain because of its longer sensorial block duration without motor block under DPNB or caudal block techniques [14]. In a caudal block study performed with levobupivacain 2.5 mg/kg dosage was found to have a faster onset and provided sufficient surgical anesthesia with postoperative analgesia [15].
We found similar postoperative pain scores for 6 hours in both DPNB and caudal block groups. Both techniques are easy, simple, and safe. They provide a comfortable postoperative period with the same doses. Weksler et al. [16] reported a similar analgesic efficacy of two techniques (penile and caudal block) using 1 ml/kg 0.25% bupivacain. Other studies comparing caudal block and penile block show similar postoperative analgesic efficacy which are in accordance with our results [17,18]. Decreasing pain scores for both groups with time are normal. However, low pain scores at all measurement intervals are important as they reflect near-perfect analgesia (5 minute FLACC pain score of the groups are mean ± standard deviation 1.05 ± 2.39, 1.35 ± 1.73). This data shows a nearly perfect analgesia level.
Limited studies were done to detect which anesthetic technique is ideal to use during the postoperative period for circumcision. Weksler et al. [16] reported a similar analgesic efficacy for caudal block and penile block for 100 children undergoing circumcision. The literature contains studies which reveal results that are similar to ours. However, some studies which reveal superiority of both techniques to each other [9,18,19].
No significant difference was found in sedation scores in the recovery room between the groups. All patients were fully awake in the 30 minutes while they are transferred (Fig. 2). We found that the first analgesic demand times were 352 ± 18 min in group 1 and 354 ± 15 min in group 2 . In a study of penile block with levobupivacain, postoperative analgesia duration was reported to be over 300 minutes [20].
We did not encounter any technical difficulties, major complications, or neurological sequele during DPNB or caudal block. In additon, no major complications after DPNB and caudal block were found in different studies [3,6,9,14,18]. Nevertheless, 2 patients in each group had minor complications. A study by Telgarsky et al. [3] of DPNB used on 96 boys reported a minor complication rate of 8.3%. In another study, edema occurred in 10 patients of 63 who had DPNB [1]. Serour et al. [2] indicated that edema occurred in 31 patients (12.4%), hematoma in twelve patients (4.8%) and vomiting in sixteen patients (6.4%). The incidence of minor complications in this study was smaller than that of this studies [1-3]. The most important limitation of this study was that the postoperative follow-up was only for 6 hours and that the number of patients in the group was small (only 25). If the children were followed longer, more precise results on postoperative analgesia duration would have been obtained.
In conclusion, DPNB and caudal block provide similar pain scores and painless postoperative periods. We did not encounter any major complications during these two techniques and our minor complication rate was small. In light of these data, we suggest that both techniques, in experienced hands, using levobupivacain, are effective, safe, simple, and easy to perform under general anesthesia. Both techniques are good for long-term postoperative analgesia after circumcision. Supplementary analgesic need is also minimalized. Thus, anesthesiologist might prefer these techniques considering all these factors.
References
1. Choi WY, Irwin MG, Hui TW, Lim HH, Chan KL. EMLA cream versus dorsal penile nerve block for postcircumcision analgesia in children. Anesth Analg. 2003; 96:396–399. PMID: 12538184.

2. Serour F, Cohen A, Mandelberg A, Mori J, Ezra S. Dorsal penile nerve block in children undergoing circumcision in a day-care surgery. Can J Anaesth. 1996; 43:954–958. PMID: 8874914.

3. Telgarsky B, Karovic D, Wassermann O, Ogibovicova E, Csomor D, Koppl J, et al. Penile block in children, our first experience. Bratisl Lek Listy. 2006; 107:320–322. PMID: 17125067.
4. Ivani G, Mosseti V. Pediatric regional anesthesia. Minerva Anestesiol. 2009; 75:577–583. PMID: 19798014.
5. Silvani P, Camporesi A, Agostino MR, Salvo I. Caudal anesthesia in pediatrics: an update. Minerva Anestesiol. 2006; 72:453–459. PMID: 16682915.
6. Brady-Fryer B, Wiebe N, Lander JA. Pain relief for neonatal circumcision. Cochrane Database Syst Rev. 2004; CD004217. PMID: 15495086.

7. De Negri P, Ivani G, Tirri T, Favullo L, Nardelli A. New drugs, new techniques, new indications in pediatric regional anesthesia. Minerva Anestesiol. 2002; 68:420–427. PMID: 12029257.
8. Cyna AM, Middleton P. Caudal epidural block versus other methods of postoperative pain relief for circumcision in boys. Cochrane Database Syst Rev. 2008; CD003005. PMID: 18843636.

9. Uguralp S, Mutus M, Koroglu A, Gurbuz N, Koltuksuz U, Demircan M. Regional anesthesia is a good alternative to general anesthesia in pediatric surgery: Experience in 1,554 children. J Pediatr Surg. 2002; 37:610–613. PMID: 11912520.

10. Voepel-Lewis T, Malviya S, Tait AR, Merkel S, Foster R, Krane EJ, et al. A comparison of the clinical utility of pain assessment tools for children with cognitive impairment. Anesth Analg. 2008; 106:72–78. PMID: 18165556.

11. Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974; 2:656–659. PMID: 4835444.

12. Humphries Y, Melson M, Gore D. Superiority of oral ketamine as an analgesic and sedative for wound care procedures in the pediatric patient with burns. J Burn Care Rehabil. 1997; 18:34–36. PMID: 9063785.

13. Metzelder ML, Kuebler JF, Glueer S, Suempelmann R, Ure BM, Petersen C. Penile block is associated with less urinary retention than caudal anesthesia in distal hypospadia repair in children. World J Urol. 2010; 28:87–91. PMID: 19466428.

14. Sanford M, Keating GM. Levobupivacaine: a review of its use in regional anaesthesia and pain management. Drugs. 2010; 70:761–791. PMID: 20394458.
15. Frawley GP, Downie S, Huang GH. Levobupivacaine caudal anesthesia in children: a randomized double-blind comparison with bupivacaine. Paediatr Anaesth. 2006; 16:754–760. PMID: 16879518.

16. Weksler N, Atias I, Klein M, Rosenztsveig V, Ovadia L, Gurman GM. Is penile block better than caudal epidural block for postcircumcision analgesia? J Anesth. 2005; 19:36–39. PMID: 15674514.

17. Stolik-Dollberg OC, Dollberg S. Bupivacaine versus lidocaine analgesia for neonatal circumcision. BMC Pediatr. 2005; 5:12. PMID: 15907216.

18. Margetts L, Carr A, McFadyen G, Lambert A. A comparison of caudal bupivacaine and ketamine with penile block for paediatric circumcision. Eur J Anaesthesiol. 2008; 25:1009–1013. PMID: 18652709.

19. Sandeman DJ, Reiner D, Dilley AV, Bennett MH, Kelly KJ. A retrospective audit of three different regional anaesthetic techniques for circumcision in children. Anaesth Intensive Care. 2010; 38:519–524. PMID: 20514962.

20. Faraoni D, Gilbeau A, Lingier P, Barvais L, Engelman E, Hennart D. Does ultrasound guidance improve the efficacy of dorsal penile nerve block in children? Paediatr Anaesth. 2010; 20:931–936. PMID: 20849498.

Fig. 1
Comparison of FLACC pain scores at different time intervals of Group 1 and Group 2. No significant difference was found between the groups. Group 1: DPNB group, Group 2: caudal block group. Data are expressed as mean ± SD.
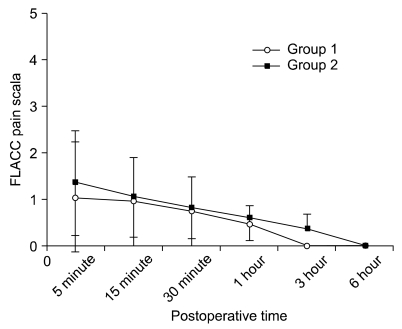
Fig. 2
Intergroup comparison of postoperative Ramsey sedation scores. Ramsey sedation scores versus time revealed that sedation scores decreased significantly over time (P < 0.001), but there was no significance difference between groups. Group 1: DPNB group, Group 2: caudal block group. Data are expressed as mean ± SD.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download