Dear Editor
Corynebacteria are aerobic, non-spore forming, and gram-positive bacilli that are commensal organisms of skin and mucosal membranes. C. striatum, like other Corynebacterium species, is a part of the normal human skin flora; therefore, it has been frequently dismissed as a blood and airway sample contaminant in the past. However, C. striatum is emerging as a cause of bloodstream infections and endocarditis [1]. Moreover, C. striatum infection outbreaks have been reported in long-stay patients with underlying disease [2]. We report a case of C. striatum bacteremia in a patient who had undergone gastrostomy. To our knowledge, there has been no report of C. striatum bacteremia in Korea so far.
A 64-yr-old quadriplegic man visited the outpatient rehabilitation clinic for gastrostomy tube change. Before visiting our hospital, he was admitted to a secondary hospital and had hypertension and diabetes mellitus. Nine months before this visit, quadriplegia developed because of hypoxic ischemic encephalopathy; he underwent tracheostomy and gastrostomy tube placement. He was admitted to our hospital owing to persistent low-grade fever with blood pressure of 156/89 mmHg. The white blood cell count was 6.02×109/L (86% segmented neutrophils), and C-reactive protein level was 3.34 mg/dL (reference range: <0.30 mg/dL). Three aerobic and anaerobic blood culture sets were incubated in the BacT/Alert 3D system (bioMérieux, Durham, NC, USA). Bacterial growth after 24-hr incubation was noted in three anaerobic culture bottles. The organism was gram-positive diphtheroid type rod and was identified as C. striatum by VITEK 2 (bioMérieux, Marcy l'Etoile, France) anaerobic & corynebacteria identification system (% probability: 99%, confidence level: excellent identification) that was confirmed by 16S rRNA sequencing. All sequences were analyzed by using the basic local alignment search tool (BLAST) and ribosomal database project. Minimal inhibitory concentration (MIC) was determined by using broth microdilution in cation-adjusted Mueller-Hinton broth with lysed horse blood according to the CLSI guidelines [3]. The organism was susceptible to vancomycin (MIC 0.5 µg/mL) and trimethoprim/sulfamethoxazole (2/38 µg/mL), but it was resistant to penicillin (8 µg/mL), cefotaxime (4 µg/mL), ceftriaxone (4 µg/mL), cefepime (4 µg/mL), tetracycline (64 µg/mL), clindamycin (>128 µg/mL), and erythromycin (>128 µg/mL).
At first, the physician assumed that C. striatum was a contaminant and the fever was caused by a urinary tract infection on the basis of the past history. Thus, only intravenous piperacillin/tazobactam was administered for the possible urinary tract infection. Culture for medical devices such as the gastrostomy or tracheostomy tubes was not performed. However, fever did not subside and C-reactive protein level was elevated; follow-up blood cultures performed on the 6th day of admission revealed C. striatum growth. The patient was continuously given intravenous piperacillin/tazobactam. As the fever subsided, he was transferred to a provincial medical center. The patient was readmitted for check-up a month after discharge and showed no sign of infection.
It is difficult to distinguish simple colonization from real infection when Corynebacterium spp. are recovered from specimens [4]. C. striatum are commonly isolated in patients with significant underlying illnesses [2] and has close association with various medical devices such as prosthetic valve/joint and central venous catheter [5] and long hospitalization.
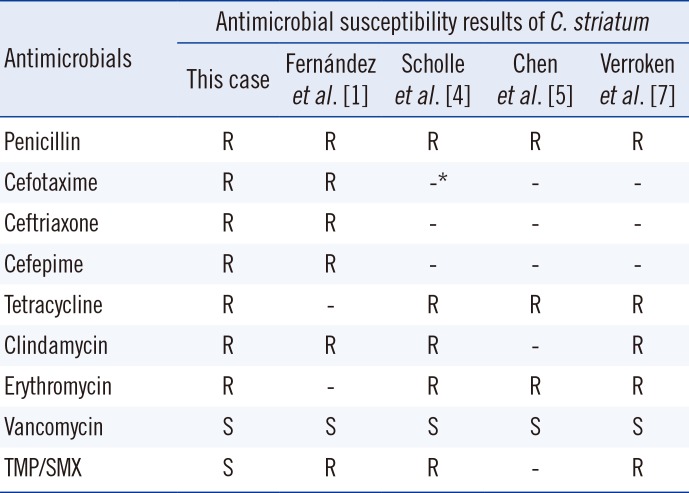
In this case, the patient suffered from diabetes, hypertension, tracheostomy, and gastrostomy. Additionally, he had stayed at a secondary health care center before being admitted to our hospital. These factors probably increased the patient's risk of C. striatum infection. Additionally, each of the blood culture sets was collected at regularly spaced intervals with adequate blood volumes, and turned positive within 24 hr. One of the recent issues related to C. striatum is the emergence and spread of multidrug resistance. Generally, most of the reported C. striatum isolates were susceptible to a wide range of antibiotics [6]; however, recent studies showed the emergence of multi-drug resistant strains with increasing use of broad-spectrum antibiotics (Table 1) [1, 4, 6, 7]. When invasive C. striatum infection is suspected, most initial therapies should include vancomycin, because in vitro resistance to vancomycin has not been reported in any of the Corynebacterium species [5]. If the patient is allergic to vancomycin, daptomycin may be an alternative. Fernandez et al. [1] reported successful treatment of a case of multidrug-resistant C. striatum endocarditis with daptomycin.
In conclusion, with increasing numbers of immunosuppressed patients and indwelling medical devices, C. striatum infections will be more commonly found and should never be overlooked as a contaminant. This report suggests the need to increase awareness of C. striatum as a pathogen causing bloodstream infections.
References
1. Fernández Guerrero ML, Molins A, Rey M, Romero J, Gadea I. Multidrug-resistant Corynebacterium striatum endocarditis successfully treated with daptomycin. Int J Antimicrob Agents. 2012; 40:373–374. PMID: 22817918.
2. Renom F, Garau M, Rubí M, Ramis F, Galmés A, Soriano JB. Nosocomial outbreak of Corynebacterium striatum infection in patients with chronic obstructive pulmonary disease. J Clin Microbiol. 2007; 45:2064–2067. PMID: 17409213.
3. Clinical and Laboratory Standards Institute. Methods for antimicrobial dilution and disk susceptibility testing of infrequently isolated or fastidious bacteria; approved guideline-second edition, M45-A2. Wayne, PA: Clinical and Laboratory Standards Institute;2010.
4. Scholle D. A spontaneous joint infection with Corynebacterium striatum. J Clin Microbiol. 2007; 45:656–658. PMID: 17151206.
5. Chen FL, Hsueh PR, Teng SO, Ou TY, Lee WS. Corynebacterium striatum bacteremia associated with central venous catheter infection. J Microbiol Immunol Infect. 2012; 45:255–258. PMID: 22154992.
6. Martínez-Martínez L, Suárez AI, Ortega MC, Rodríguez-Jiménez R. Fatal pulmonary infection caused by Corynebacterium striatum. Clin Infect Dis. 1994; 19:806–807. PMID: 7803665.
7. Verroken A, Bauraing C, Deplano A, Bogaerts P, Huang D, Wauters G, et al. Epidemiological investigation of a nosocomial outbreak of multidrug-resistant Corynebacterium striatum at one Belgian university hospital. Clin Microbiol Infect. 2014; 20:44–50. PMID: 23586637.
Table 1
Multidrug resistant Corynebacterium striatum in the literature
| Antimicrobials | Antimicrobial susceptibility results of C. striatum | ||||
|---|---|---|---|---|---|
| This case | Fernández et al. [1] | Scholle et al. [4] | Chen et al. [5] | Verroken et al. [7] | |
| Penicillin | R | R | R | R | R |
| Cefotaxime | R | R | -* | - | - |
| Ceftriaxone | R | R | - | - | - |
| Cefepime | R | R | - | - | - |
| Tetracycline | R | - | R | R | R |
| Clindamycin | R | R | R | - | R |
| Erythromycin | R | - | R | R | R |
| Vancomycin | S | S | S | S | S |
| TMP/SMX | S | R | R | - | R |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download