Abstract
Intramuscular hemangioma (IMH) is a rare, benign vascular lesion that frequently develops within skeletal muscles. Preoperatively, accurate diagnosis of IMH is often extremely difficult because of nonspecific clinical findings and the inaccuracy of fine-needle aspiration cytology. IMH is suspected in only 8% of preoperative diagnoses before surgical exploration. Here, we report a case of a 44-year-old man with a huge IMH in the anterior scalene muscle that was preoperatively diagnosed using ultrasonography-guided core needle biopsy, and was successfully treated based on preoperative clinical information.
Intramuscular hemangioma (IMH) is a rare, benign vascular lesion that frequently develops within skeletal muscles [1]. Head and neck involvement is considered unusual, and most IMH cases originate from the masseter and trapezius [234]. Only four cases of IMH in cervical scalene muscle have been described in three English language reports [567].
IMHs of the scalene musculature present a significant diagnostic challenge [7]. The preoperative diagnosis of head and neck IMH is rendered difficult by its rarity and nonspecific radiologic findings [8]. Preoperatively, the accurate diagnosis of an IMH is often extremely difficult because of nonspecific clinical findings and the inaccuracy of fine-needle aspiration cytology (FNAC). Particularly, FNAC results in a misdiagnosis or no diagnosis due to an excessively bloody specimen. Here, we present a case of IMH in the anterior scalene muscle that was diagnosed using ultrasonography (US)-guided core needle biopsy, and was successfully treated based on preoperative clinical information.
A 43-year-old male presented with a huge mass in the right side of his neck that had been present for 1 year. He had no history of trauma prior to the appearance of swelling. Upon examination of the neck, painless diffuse swelling was noted. A neck computed tomography (CT) revealed a hypervascular mass, approximately 8.5 cm in size, at the right posterior cervical space. CT showed that the right common carotid artery (CCA) was anteriorly displaced, and the mass showed isosignal intensity relative to muscle (Fig. 1A). Magnetic resonance imaging (MRI) was diagnostic, and revealed a well-defined mass with slightly increased signal intensity on gadolinium-enhanced T1-weighted fat-saturated imaging (Fig. 1B), and increased signal intensity on T2-weighted imaging (Fig. 1C) in the right anterior scalene muscle.
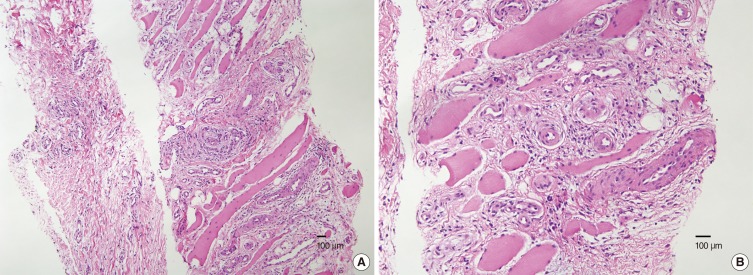
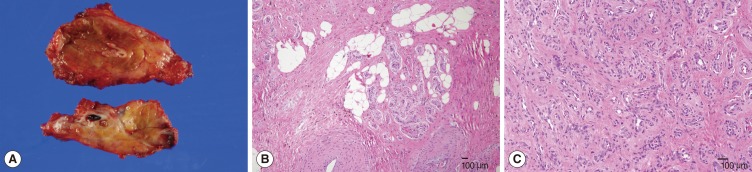
The radiologist suggested angiomyolipoma, a neurogenic tumor, or paraganglioma as differential diagnoses based on the CT and MRI scans. US showed a hypoechogenic and hypervascular mass involving the right parapharyngeal space posterolateral to the right CCA (Fig. 2). US-guided core needle biopsy was performed without complications. The pathologic findings suggested that the specimen had increased vasculature and adipose tissue, and was consistent with IMH (Fig. 3).
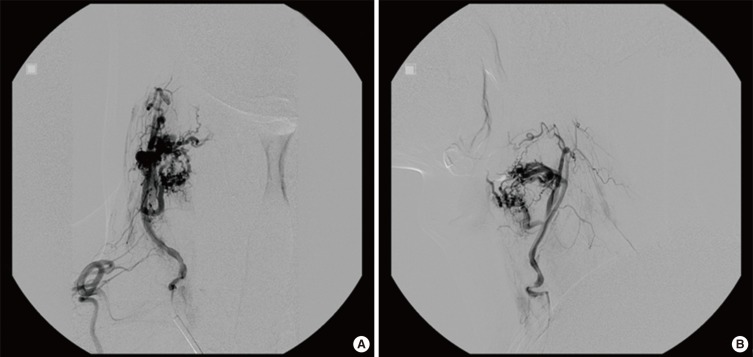
To prevent massive intraoperative bleeding, an angiography and tumor embolization were planned 2 days before the elective operation. The angiography demonstrated a hypervascular mass fed by a branch of the right thyrocervical artery, and the mass was successfully embolized (Fig. 4).
The patient underwent surgical exploration under general anesthesia. Intraoperatively, the mass bled profusely but was easily controlled. It was firmly attached to the adjacent muscles, but was dissected without bleeding. The great vessels (CCA, internal jugular vein) and important nerves (vagus nerve, spinal accessory nerve, phrenic nerve) were not injured, and the main mass was completely excised, including the surrounding normal musculature. The size of the mass was about 9 cm×6 cm×3 cm, and immediate postoperative bleeding was moderate. Histopathologic examination of the surgical specimen was compatible with IMH (Fig. 5). Postoperative courses were uneventful, and the patient was discharged without complications.
In 1843, Liston [9] first described benign and congenital neoplasms localized to the muscle of the lower extremity as IMH. IMH accounts for about 1% of all hemangiomas, and 14%-21% of IMHs develop in the head and neck [7]. The masseter and trapezius muscles are the most common sites in the head and neck, followed by the sternocleidomastoid, mylohyoid, temporalis, and orbital muscles [5]. Excluding our case, only four cases of IMH originating from the scalene musculature have been reported in the English literature [567]. One case [6] was located in the middle scalene, another [5] in the posterior, and the others [7] were located in unspecified scalene musculatures. IMH involving the anterior scalene muscle is very rare; to the best of our knowledge, this study is the first report of such a case.
Clinically, these tumors present as localized, rubbery swellings with smooth surfaces and distinct margins that are noncompressible. There are no associated vascular findings on examination due to surrounding muscular fibrosis. The lesions of IMH lack typical vascular signs such as thrills, bruits, or color changes in superficial hemangioma. Pain may be present due to compression by the growing mass; however, despite the huge and firm mass, our patient did not complain of pain and tenderness in his neck.
The preoperative diagnosis of IMH is difficult due to its rarity and nonspecific clinical manifestations. In fact, IMH is suspected in only 8% of preoperative diagnoses before surgical exploration [5]. Its diagnosis is based on imaging data, because physical examination is imprecise and FNAC frequently results in misdiagnosis or indeterminate results due to an excessively bloody specimen. The association between US and/or CT of a hyper-vascularized mass and characteristic vascular lacunae, and repeated US-guided FNAC showing the presence of a purely bloody specimen may be considered strongly suggestive of IMH [1]. Nevertheless, FNAC can result in misdiagnosis or no specific diagnosis for IMH [7].
US-guided core needle biopsy is widely performed in numerous sites, and is commonly used in the diagnoses of head and neck lesions. Saltzman et al. [10] successfully performed a US-guided core needle biopsy in a case of IMH in the posterior belly of the digastric muscle, and the histology was preoperatively confirmed. There is a widespread perception that US-guided core needle biopsy is contraindicated in hemangiomas due to a high risk of bleeding. However, Saltzman et al. [10] explained the feasibility of US-guided core needle biopsy as follows. In contrast to other hemangiomas, IMHs contain variable amounts of nonvascular tissue such as fat, smooth muscle, and fibrous tissue. These nonvascular elements with compression by surrounding structures may prevent stagnation of blood within the tumor, and may reduce the possibility of bleeding or hematoma that can occur in cutaneous or liver hemangiomas during core needle biopsy. We also tried preoperative US-guided core needle biopsy and were able to diagnose IMH preoperatively. We did not note any complications, such as bleeding or hematoma with proper compression after core needle biopsy.
Unlike cutaneous hemangioma, spontaneous regression generally does not occur in IMH [11]. No cases of malignant transformation of IMH have been reported [12]. However, treatment for IMH might be necessary if there are specific symptoms, cosmetic problems, or the possibility of other malignancy [7]. Local recurrences ranging from 9% to 28%, even after wide resection of a cuff of normal muscle around IMHs, have been described [1]. The treatment of choice is complete en bloc resection, including the cuff of surrounding muscle because IMH tends to infiltrate adjacent tissues. On the other hand, in our case and in four cases of cervical scalene IMHs, no recurrence was found with a preoperatively correct diagnosis using imaging tests such as CT or MRI and complete resection [17]. Some authors have suggested that radiation therapy should be contraindicated for IMH due to its low curability and the risk of malignant transformation [13].
In conclusion, IMH originating from the anterior scalene muscle is rare. The preoperative diagnosis of IMH is difficult, but US-guided core needle biopsy is a safe and confirmatory tool for diagnosis. Surgical resection is the treatment of choice for IMH, and preoperative angiography and embolization could be helpful for the control of intraoperative bleeding.
References
1. Giudice M, Piazza C, Bolzoni A, Peretti G. Head and neck intramuscular haemangioma: report of two cases with unusual localization. Eur Arch Otorhinolaryngol. 2003; 10. 260(9):498–501. PMID: 12748867.

2. Chaudhary N, Jain A, Gudwani S, Kapoor R, Motwani G. Intramuscular haemangioma of head and neck region. J Laryngol Otol. 1998; 12. 112(12):1199–1201. PMID: 10209624.

3. Okabe Y, Ishikawa S, Furukawa M. Intramuscular hemangioma of the masseter muscle: its characteristic appearance on magnetic resonance imaging. ORL J Otorhinolaryngol Relat Spec. 1991; 53(6):366–369. PMID: 1784478.

4. Welsh D, Hengerer AS. The diagnosis and treatment of intramuscular hemangiomas of the masseter muscle. Am J Otolaryngol. 1980; 2. 1(2):186–190. PMID: 7446838.

5. Scott JE. Haemangiomata in skeletal muscle. Br J Surg. 1957; 3. 44(187):496–501. PMID: 13510618.
6. Ferlito A, Nicolai P, Gale N. Intramuscular haemangioma of the middle scalene muscle. Acta Otorhinolaryngol Belg. 1980; 34(3):345–349. PMID: 7234376.
7. Van Abel KM, Carlson ML, Janus JR, Torres-Mora J, Moore EJ, Olsen KD, et al. Intramuscular hemangioma of the scalene musculature masquerading as a paraganglioma: a case series. Am J Otolaryngol. 2013; Mar-Apr. 34(2):158–162. PMID: 23159015.

8. Itoh K, Nishimura K, Togashi K, Fujisawa I, Nakano Y, Itoh H, et al. MR imaging of cavernous hemangioma of the face and neck. J Comput Assist Tomogr. 1986; Sep-Oct. 10(5):831–835. PMID: 3745555.

9. Liston R. Case of erectile tumour in the popliteal space.-removal. Med Chir Trans. 1843; 26:120–132.

10. Salzman R, Buchanan MA, Berman L, Jani P. Ultrasound-guided core-needle biopsy and magnetic resonance imaging in the accurate diagnosis of intramuscular haemangiomas of the head and neck. J Laryngol Otol. 2012; 4. 126(4):391–394. PMID: 22258504.

11. Moumoulidis I, Durvasula VS, Jani P. An unusual neck lump: intramuscular haemangioma of the sternocleidomastoid muscle. Eur Arch Otorhinolaryngol. 2007; 10. 264(10):1257–1260. PMID: 17593381.

12. Stofman GM, Reiter D, Feldman MD. Invasive intramuscular hemangiomas of the head and neck. Ear Nose Throat J. 1989; 8. 68(8):612–616. PMID: 2583030.
13. Wolf GT, Daniel F, Krause CJ, Kaufman RS. Intramuscular hemangioma of the head and neck. Laryngoscope. 1985; 2. 95(2):210–213. PMID: 3968956.

Fig. 1
Neck computed tomography (CT) revealed a hypervascular mass, approximately 8.5 cm in size, at the right posterior cervical space (A). On CT, the right carotid artery was anteriorly displaced, and the mass showed isosignal intensity relative to muscle. Magnetic resonance imaging (MRI) was diagnostic and revealed a well-defined mass with slightly increased signal intensity on gadolinium-enhanced T1-weighted fat-saturated imaging (B) and slight increased signal intensity on T2-weighted imaging (C) within the right anterior scalene muscle.
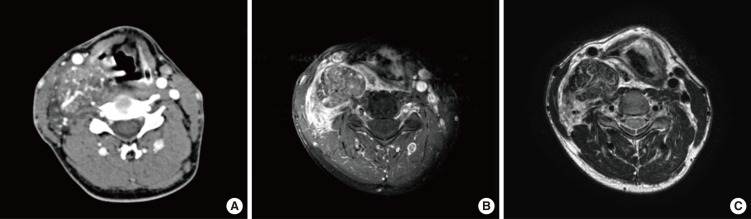
Fig. 2
Ultrasonography (US) showed a hypoechogenic and hypervascular mass involving the right parapharyngeal space posterolateral to the right common carotid artery. US-guided core needle biopsy was performed without complications.
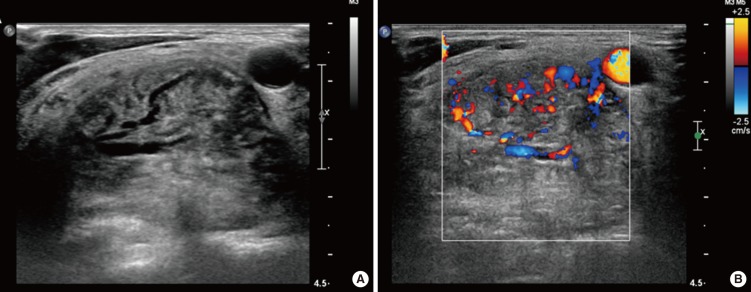
Fig. 3
The core needle biopsy specimen revealed skeletal muscle fragments with increased vasculature and adipose tissue that was diagnosed as intramuscular hemangioma (H&E: A, ×100; B, ×200).




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download