INTRODUCTION
Since Gagner [
1] first introduced endoscopic parathyroidectomy in 1996, endoscopic thyroidectomy has made much progress and its surgical indications have been widened. It has also gained special popularity in Asian countries, such as Korea and Japan, where there is great cultural sensitivity to anterior neck scars [
2].
Several approaches have been developed to date, such as the cervical, breast, axillo-breast, and chest approaches. Korean surgeons have made many contributions to the development of new approaches and are now a leading group in the endoscopic thyroidectomy field [
3]. However, there is no established consensus regarding surgical indications, contraindications, advantages, or disadvantages. There is also no comparative survey on the various endoscopic thyroidectomy approaches used by head and neck surgeons and endocrine surgeons.
Therefore, we assessed the current status of endoscopic thyroidectomy procedures in Korea in terms of the indications, contraindications, advantages, disadvantages, complications, and limitations of each approach.
MATERIALS AND METHODS
Between May and June 2011, we performed an email survey of 29 experienced endoscopic thyroid surgeons in South Korea. In total, 17 university hospitals and 4 general hospitals participated in the survey. The response rates were 73.3% (11/15) for head and neck surgeons and 71.4% (10/14) for endocrine surgeons.
The survey consisted of 15 questions about the pros and cons of their approach, the advantages and disadvantages of endoscopic surgery relative to conventional thyroidectomy, and the indications, contraindications, complications, limitations, and the future of endoscopic surgery.
The questions in the survey were as follows:
What is your current approach of endoscopic thyroidectomy?
In your opinion, how many cases are required to complete the learning curve for endoscopic thyroidectomy?
What do you consider to be the advantage(s) of your current approach?
What do you consider to be the disadvantage(s) of your current approach?
What do you consider to be the greatest advantage of endoscopic thyroidectomy?
What do you consider to be the greatest disadvantage of endoscopic thyroidectomy?
What are your indications for endoscopic thyroidectomy?
What are your contraindications for endoscopic thyroidectomy?
What do you consider to be the advantages of robotic thyroidectomy over endoscopic thyroidectomy?
What do you consider the complication rate to be, such as recurrent laryngeal nerve (RLN) injury and parathyroid gland (PTG) preservation, between endoscopic and conventional thyroidectomy?
What do you consider to be the most serious complication related to endoscopic thyroidectomy?
Do you have any tip to avoid postthyroidectomy syndrome (PTS)?
Do you feel that a total thyroidectomy can be performed completely with endoscopic thyroidectomy?
Do you feel that a central compartment neck dissection (CND) can be carried out completely with endoscopic thyroidectomy?
What do you think the future holds for endoscopic thyroidectomy?
RESULTS
Currently used endoscopic thyroidectomy approach
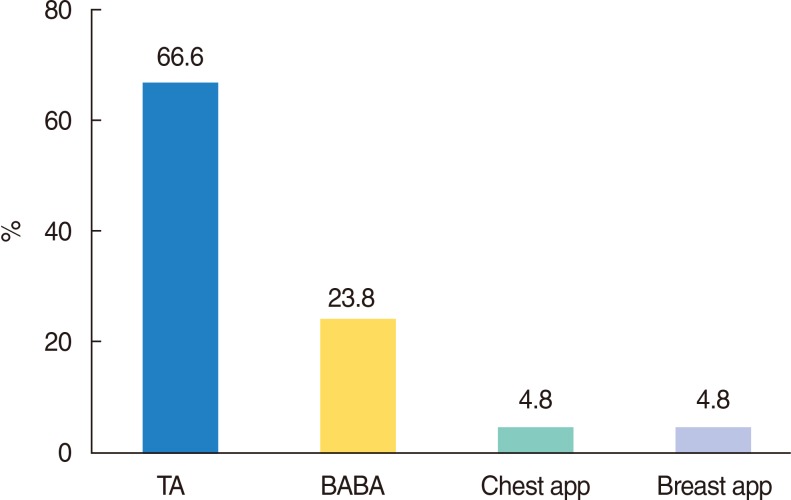
In terms of the preferred approach for endoscopic thyroid surgery, the gaseless transaxillary approach (TA) was most frequently used (66.6%), followed by the bilateral axillo-breast approach (BABA) with gas insufflation (23.8%) (
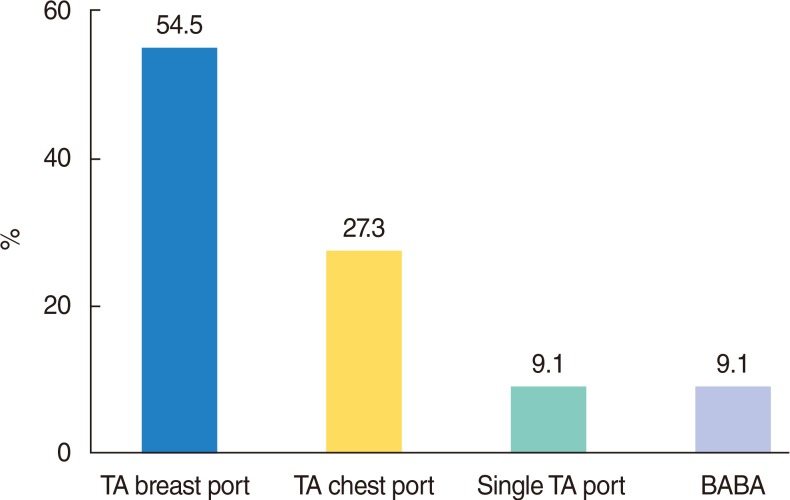
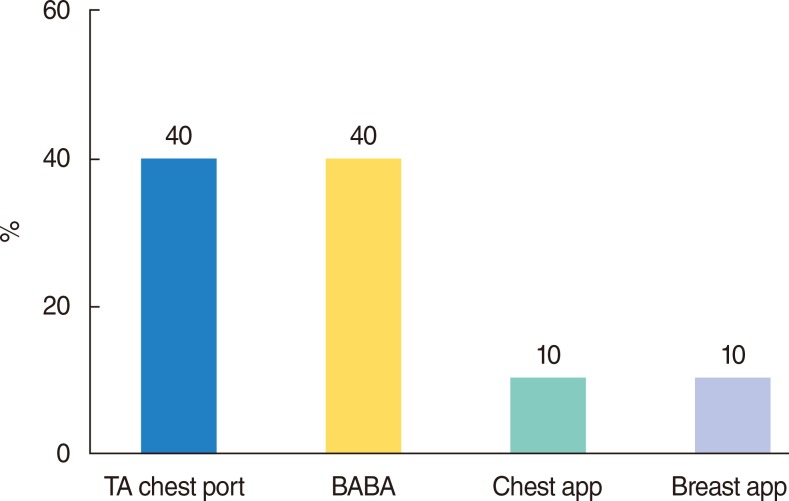
Fig. 1). More specifically, most head and neck surgeons used the TA (91%) and its variants (e.g., TA with breast port, 54.5%; TA with chest port, 27.3%; and single-port TA, 9.1%). In contrast, endocrine surgeons used each approach equally (44.4% used each approach) (
Figs. 2,
3).
Learning curve for endoscopic thyroidectomy
In response to the question about how many surgeries were required to complete the learning curve for endoscopic thyroidectomy, 35% responded that 30-50 cases were sufficient, 35% of surgeons responded that 10-30 cases were required, 25% indicated that more than 50 cases were required, and 5% responded that fewer than 10 cases was enough.
Advantages and disadvantages of endoscopic thyroidectomy procedure
Advantages of endoscopic thyroidectomy included not producing a scar (57.1%), being less expensive than robotic thyroidectomy (28.6%), being innovative (11.4%), and preserving the RLN/PTG (2.9%). The disadvantages included being more invasive than conventional thyroidectomy (49.9%), being difficult for total thyroidectomy (25.0%), the fact that its safety has not been proven (17.9%), the possibility of PTS (3.6%), and being more expensive than conventional thyroidectomy (3.6%).
Advantages and disadvantages of the TA and BABA
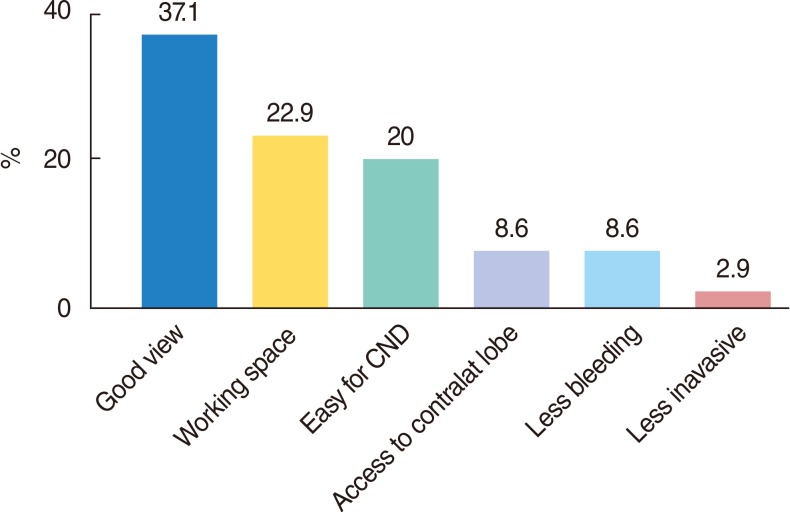
Advantages of the TA included providing a good surgical view, like conventional thyroidectomy (37.1%), having enough work space (22.9%), the ease of ipsilateral CND (20.0%), and miscellaneous reasons (
Fig. 4). The disadvantages included being difficult to complete total thyroidectomy (44.4%), being invasive (22.2%), assistant dependency (16.7%), not providing enough work space (11.1%), and providing a poor surgical view (5.6%).
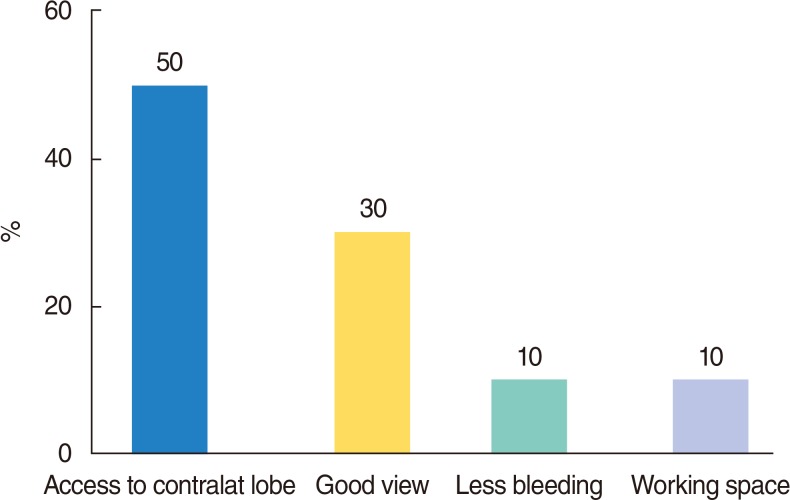
Advantages of the BABA included its ease of access to the contralateral lobe (50.0%), providing a good surgical view (30.0%), being associated with less bleeding (10.0%), and provide enough work space (10.0%) (
Fig. 5). Disadvantages included being invasive (40.0%), assistant dependency (40.0%), and being associated with CO
2-related complications (20.0%).
Advantages of robotic thyroidectomy over endoscopic thyroidectomy
Advantages of robotic thyroidectomy over endoscopic thyroidectomy included having one more arm than endoscopic thyroidectomy (32.7%), not requiring an assistant (20.4%), the ease of contralateral lobe removal (18.4%), the fact that a smaller work space is needed (18.4%), and no differences between endoscopic thyroidectomy for micropapillary thyroid cancer (10.1%).
Indications and contraindications for endoscopic thyroidectomy
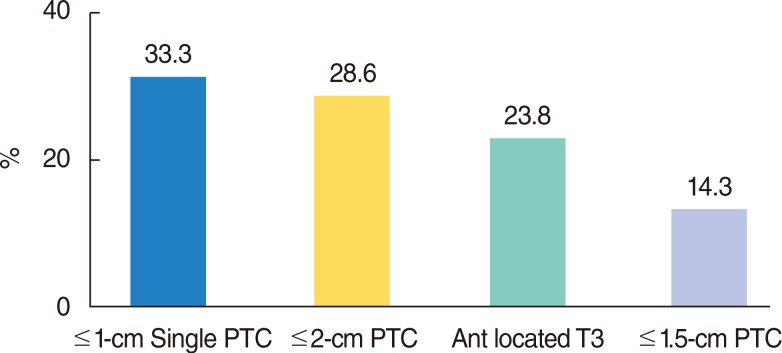
The most common response for indications for endoscopic thyroid surgery was cases of single papillary thyroid cancer (PTC) less than 1 cm (33.3%), followed by PTC of less than 2 cm (28.6%), anterior-located T3 disease (23.8%), and cancer less than 1.5 cm (14.3%) (
Fig. 6).
For benign thyroid tumors, 36.4% of surgeons responded that there was no size limit (36.4%), and 36.4% thought that less than 5 cm and 27.3% thought that less than 4 cm were the appropriate sizes.
Contraindications for endoscopic thyroidectomy included Graves' disease (25.0%), inferior extended goiter (21.2%), PTC with capsule invasion (19.2%), PTC in the adjacent trachea (17.3%), and miscellaneous (
Fig. 7).
Complications of endoscopic thyroidectomy
When asked to compare complications, such as RLN injury and postoperative hypoparathyroidism, between conventional and endoscopic thyroidectomy, the most frequent response was that there is no difference (55.0%). Others indicated that endoscopic thyroidectomy has more frequent complications (30.0%) and the remainder thought that conventional thyroidectomy has more complications (15.0%).
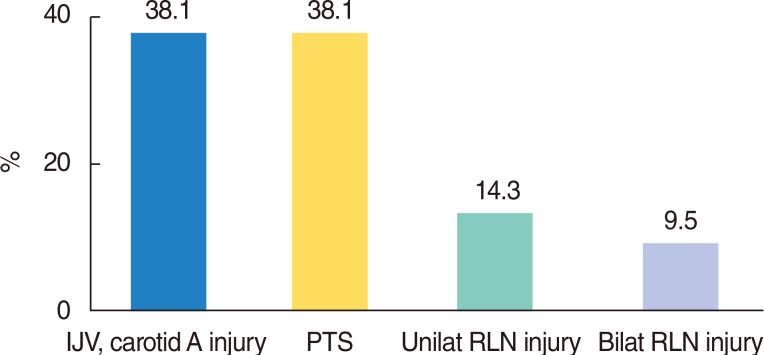
The most serious complication of endoscopic thyroidectomy reported by the respondents was injury to a major vessel (38.1%) such as the internal jugular vein and carotid artery, followed by PTS (38.1%), unilateral RLN injury (14.3%), and bilateral RLN injury (9.5%) (
Fig. 8).
Advice for avoiding postthyroidectomy syndrome
To avoid PTS, 45.1% of surgeons responded that adequate dissection was important. Other responses included doing stretching exercises following surgery (29.0%) and having an antiadhesive barrier (19.4%). The remainder indicated that PTS is inevitable (6.5%).
Completeness of endoscopic thyroidectomy and central CND
As to whether complete total thyroidectomies could be carried out through endoscopic thyroidectomy alone, 71.4% responded positively. However, 19.0% of surgeons responded that complete total thyroidectomy could not be accomplished, and 9.5% of responders believed that endoscopic procedures were only enough for a hemithyroidectomy.
Regarding complete CND, 52.4% of surgeons responded that a complete ipsilateral CND could be performed through an endoscopic procedure, and 19.0% thought that even a bilateral CND would be possible. However, 28.6% of responders thought that it could be used only for a sentinel lymph node biopsy.
Future role of endoscopic thyroidectomy
Regarding the future role of endoscopic thyroidectomy, 34.8% of surgeons responded that it is a novel approach itself and will play a role in the future, 34.8% responded that the approach is only a transient technique that will eventually lead to robotic thyroidectomy, and 30.4% responded that it will play a limited role in the future.
DISCUSSION
Although endoscopic thyroidectomy has shown much progress since its introduction, there are no guidelines regarding indications, contraindications, or operative techniques [
4]. Several approaches have been developed to date, such as the cervical, breast, axillo-breast, and chest approaches. Among endocrine surgeons, Kim et al. [
5], Park et al. [
6], Yoon et al. [
7], and Choe et al. [
8] have been instrumental in developing the chest approach, the breast approach, the BABA with gas insufflation, and the TA without gas insufflation, respectively. Among head and neck surgeons, Koh et al. [
9] developed the unilateral axillo breast approach and Tae et al. [
10] developed the gasless unilateral axillo breast approach.
However, there is much debate and conflict about these procedures. Moreover, there is no consensus for surgical indications, contraindications, advantages, or disadvantages. There has also been no comparative study of the various endoscopic thyroidectomy approaches involving both head and neck surgeons and endocrine surgeons.
Thus, it is important to collect and analyze data from experienced surgeons to understand the current situation, the differences between the approaches. Today, there tends to be a focus on the TA and BABA, in particular BABA with CO
2 gas insufflation (Yoon et al. [
7]) and TA without CO
2 gas insufflation (Choe et al. [
8]). According to our survey, the TA is the most preferred approach; 66.7% of the surgeons preferred to use it for endoscopic thyroidectomy. Another 23.8% of surgeons prefer the BABA, and only 4.8% reported using the chest and breast approaches (
Fig. 2).
There was a strong preference among head and neck surgeons to use the TA (91%) and its variants (TA with breast port, TA with chest port, and single-port TA) versus the BABA (9%). However, among endocrine surgeons, the percentages for the TA (44.4%) and the BABA (44.4%) were the similar. We assumed that these phenomena may be due to no familiarity with gas insufflation, relative familiar anatomy on pectoralis major muscle through pectoral myocutaneous flap experiences, and familiar knowledge about sternocleidomastoid muscle through neck dissection experiences of head and neck surgeons.
The main reported advantages of the TA were providing a good surgical view (37.1%) and enough working space (22.9%), similar to an open thyroidectomy. The main disadvantage was difficulty removing the contralateral lobe (44.4%) because it could access the thyroid gland unilaterally.
The BABA was considered to have good access to the contralateral lobe, compared to the TA because it could access the thyroid gland bilaterally.
For the indications and contraindications of endoscopic thyroidectomy, 33.3% responded that less than 1-cm single PTC (33.3%) was an adequate indication for endoscopic surgery, and 28.6% responded that less than 2-cm PTC was a possible indication. However, 23.8% responded that if the tumor was located anteriorly, even T3 PTC could be a possible indication for an endoscopic thyroidectomy. These results suggest that location is a more important factor in determining whether endoscopic thyroidectomy is possible.
For complications, such as RLN injury and hypoparathyroidism, most surgeons thought that there were not significant differences between conventional and endoscopic approaches (55.0%). However, in terms of serious complications of endoscopic thyroidectomy, many surgeons (38.1%) worried about injury to major vessels, such as the internal jugular vein and carotid artery during the dissection and PTS following thyroidectomy (38.1%) [
11].
Of the surgeons, 71.4% believed it was feasible to perform a complete thyroidectomy endoscopically. However, for CND, 81.0% thought that an endoscopic approach was not as effective for bilateral complete CND as a conventional CND [
12]. Interestingly, the survey showed that endoscopic thyroidectomy approaches were thought to be good for cosmetic results but more invasive than a conventional thyroidectomy.
To survive as a new approach, it is important to assemble strong evidence of endoscopic thyroidectomy's efficacy and there is a need for practical, consensus-based guidelines. The role of endoscopic thyroidectomy has still not been established; some consider it a novel approach in and of itself (34.8%) and others consider it part of a transition to robotic thyroidectomy (34.8%). In the long term, endoscopic thyroidectomy has to compete with both conventional thyroidectomy and robotic thyroidectomy to survive as a new procedure.
This survey of a nationwide sample of endoscopic thyroidectomy surgeons provides clues for the establishment of a general consensus about certain aspects of endoscopic thyroidectomy.
In conclusion, according to this nationwide survey of surgeons, the TA and BABA are the current major endoscopic thyroidectomy approaches in Korea, and their advantages and disadvantages overlap. Our results shed light on a possible general consensus regarding aspects of endoscopic thyroidectomy, such as its advantages, disadvantages, complications, and limitations.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download