Abstract
Vegetable granuloma or pulse granuloma results from the implantation of food particles of vegetable origin. Pulse granulomas have mainly been reported in association with lung aspirations, the oral cavity with a history of oral procedures and less frequently in gastrointestinal tracks. We report a 31-year-old woman who presented with right nasal obstruction and was found to have a firm mass in the right nasal cavity. Paranasal sinus computerized tomography scans identified a calcified ring lesion in her right nasal cavity. Endoscopic sinus surgery was performed, and pathology examination revealed a lesion consistent with a pulse granuloma that contains starch granules with cellulose envelopes appearing as hyaline rings surrounded by inflammation cells and concentrically arranged delicate connective tissue. Pulse granuloma is a well described entity with distinct histopathology. However, pulse granulomas are rare, and especially extraoral pulse granulomas are extremely rare. We found that pulse granuloma can be occurred in the nasal cavity through regurgitation.
Pulse granuloma or vegetable granuloma results from the implantation of food particles of plant or vegetable origin. Pulse granuloma is an unusual reaction to vegetable matter that is characterized by aggregates of thin, variably sized hyaline rings [1,2]. They have mainly been reported in association with lung aspirations, the oral cavity with a history of oral procedures and less frequently in intestinal fistulae or stomach ulcers [2,3,4,5]. They are exceedingly rare elsewhere. Histological characteristics may differ, possibly related to the length of time in the tissue. We recently experienced a case involving a pulse granuloma in the nasal cavity. To our knowledge this is the first reported case of a pulse granuloma in the nasal cavity, and we report this case with an appropriate review.
A 31-year-old female attended with a 1 year history of right sided nasal obstruction, purulent discharge and pain. She underwent endonasal rhinoplasty at local plastic surgery clinic 10 years ago and didn't have other recent history of nasal surgery or trauma. During nasal endoscopic examination a firm mass adhering to the right inferior turbinate, middle turbinate and the nasal septum was seen in her right nasal cavity with purulent discharge (Fig. 1). The paranasal sinus computed tomography scans identified a calcified ring lesion in the right nasal cavity and bilateral maxillary sinusitis (Fig. 2).
We performed endoscopic sinus surgery under general anaesthesia. The surface of calcified mass was hard, but inner part was fragile. The mass was completely removed in several fragments. Uncinectomy and middle meatal antrostomy was also carried out for maxillary sinusitis. The bleeding was controlled with a coagulation-suction device as well as with a light packing, which was removed 2 days later without recurrence of bleeding.
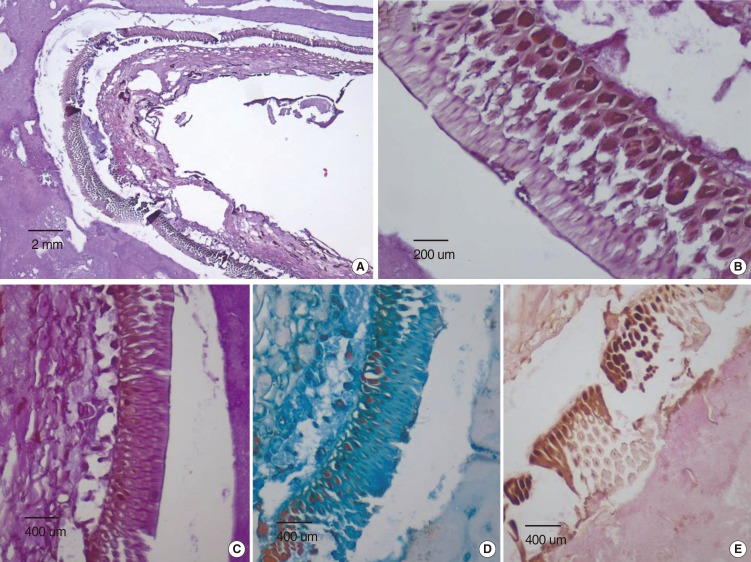
The microscopic examination revealed an interesting finding, the presence of homogenous, pale, eosinophilic material resembling vegetable matter in the calcified wall. It was a double layered refractile hyaline membrane surrounded with calcified amorphous material (Fig. 3A, B). A degenerated wall of plant is positive for both periodic acid Schiff (PAS) and alcian blue pH 2.5 stains, but negative for Van Gieson stain (×200, respectively) (Fig. 3C-E). The diagnosis of nasal pulse granuloma was made. Healing was uneventful, and the patient was symptom-free after 6 months of follow up. There was also no recurrence of the granuloma.
Pulse granulomas are rare, odd reactions to vegetable matter characterized by clusters of eosinophilic hyaline rings admixed with inflammation, and usually occupy the oral region [1]. The hyaline rings ultrastructurally resemble cellulose or collagen. Occasionally, there may be presence of small round calcified bodies within the amorphous hyaline material.
King first used the term "oral pulse granuloma" for lesion of hyaline ring as structures originating from fragments of pulses (edible seeds of legumes) during his presentation at Annual Meeting of the American Academy of Oral Pathology in 1978 [3]. Various theories had been proposed for the composition and origin of the hyaline rings, including degenerated blood vessels related to vasculitis, hence a previous name, "giant-cell hyaline angiopathy" [6,7]. Most research suggest that pulse granulomas represent unique reactions to vegetable matter, hence the alternate name, "vegetable granuloma," and that the hyaline rings are related to cellulose and collagen [1,2,3,4,5].
The vast majority of pulse granulomas have been reported as occurring in the oral region, some reports have dealt with extraoral, in particular, pulmonary lesions in infants or severely debilitated persons caused by aspirated fragments of pulses [3]. Several authors reported pulse granulomas in the gastrointestinal track such as peridiverticular colon or rectum [8,9]. Rhee and Wu [10] demonstrated that pulse granulomas can occur outside the digestive tract and lungs in association with passage of gastrointestinal contents through fistulae. The cases involved the gallbladder, fallopian tube and skin. Nambudripad et al. [2] recently reported a highly unusual pulse granuloma that occupied periprostatic soft tissue and that was iatrogenically caused by prostatic core biopsies. Lastly, Karamurzin et al. [4] reported not only periprostatic pulse granuloma but also mesocolonic lymph node and gastric subserosa. We recently detected a nasal pulse granuloma that occurred at a previously unreported site.
Pulse granuloma is rarely diagnosed clinically and it remains largely a microscopic diagnosis. Histologically, the pulse granuloma contains starch granules with cellulose envelopes that appear as hyaline rings surrounded by foreign body giant cells and concentrically arranged delicate connective tissue [1,3,5]. Hyaline rings in the present case stained strongly for PAS as demonstrated by various authors [1,5]. Additionally, alcian blue showed positivity for vegetable material. Vegetable cell walls contain acidic group such as carboxyls which are stained by alcian blue, while Van Gieson was negative, which was in accordance with other authors [1,5].
Interestingly, our case showed a definite vegetable matter stained strongly for PAS and alcian blue, but no severe chronic inflammation. Instead, the vegetable matter was totally encircled with thick calcified walls. Pulse granuloma may be surrounded by spherical calcification and show different histological characteristics, possibly related to the length of time in the tissue [2,3]. In addition, our case was formed not in the nasal mucosa, but in the nasal cavity, in other words, in the narrow nasal passage. For this reason, it might appear to be a little mucosa reaction, such as foreign body giant cells.
Based on the regular use of leguminous foods (pulses) in the human diet, it is surprising that intake of legumes is extremely rarely, if ever, reported associated with the development of a pulse granuloma, apart from the occurrence of vegetable aspiration or lentil pulse pneumonia in debilitated patients and children [3]. Our patient also did not have any preference for leguminous food, but she had a habit of vomiting drinking too much. This habit might have provided the entry of vegetable matter in her nasal cavity.
Extraoral pulse granulomas are extremely rare, are usually markers of serious pathology and may be easily misdiagnosed as other entities. In addition, they can be surrogate markers of serious pathology that enables vegetable matter to escape the alimentary canal. Our case showed that it could occur in the nasal cavity. Thus, even though benign nonneoplastic lesions or disorders of the nasal cavity represent a diverse group of disorders, pulse granuloma is one of the lesions considered in the nasal cavity.
We presented the first pulse granuloma in the nasal cavity. Pulse granuloma is a well described entity with distinct histopathology. However, pulse granulomas are rare, and especially extraoral pulse granulomas are extremely rare. We found that pulse granuloma can be occurred in the nasal cavity through regurgitation.
References
1. Talacko AA, Radden BG. Oral pulse granuloma: clinical and histopathological features. A review of 62 cases. Int J Oral Maxillofac Surg. 1988; 12. 17(6):343–346. PMID: 2464044.

2. Nambudripad R, Narula N, Wu ML. Iatrogenic pulse granuloma detected at prostatectomy. Int J Surg Pathol. 2008; 1. 16(1):96–100. PMID: 18203796.

3. Philipsen HP, Reichart PA. Pulse or hyaline ring granuloma: review of the literature on etiopathogenesis of oral and extraoral lesions. Clin Oral Investig. 2010; 4. 14(2):121–128.

4. Karamurzin YS, Narula S, Khanifar E, Kim YS, Wu ML. Pulse granulomas in highly unusual sites. Histopathology. 2009; 1. 54(2):268–269. PMID: 19207957.

5. Harrison JD, Martin IC. Oral vegetable granuloma: ultrastructural and histological study. J Oral Pathol. 1986; 7. 15(6):322–326. PMID: 2428961.

6. Dunlap CL, Barker BF. Giant-cell hyalin angiopathy. Oral Surg Oral Med Oral Pathol. 1977; 10. 44(4):587–591. PMID: 71674.

7. Hase MP, Radden BG, Reade PC. Torulopsis glabrata infection in the oral cavity. J Oral Pathol. 1976; 1. 5(1):8–16. PMID: 814222.

8. Zhai J, Maluf HM. Peridiverticular colonic hyaline rings (pulse granulomas): report of two cases associated with perforated diverticula. Ann Diagn Pathol. 2004; 12. 8(6):375–379. PMID: 15614745.

9. Pereira TC, Prichard JW, Khalid M, Medich DS, Silverman JF. Rectal pulse granuloma. Arch Pathol Lab Med. 2001; 6. 125(6):822–823. PMID: 11371241.

10. Rhee DD, Wu ML. Pulse granulomas detected in gallbladder, fallopian tube, and skin. Arch Pathol Lab Med. 2006; 12. 130(12):1839–1842. PMID: 17149960.

Fig. 1
A firm mass (arrow) adhering to the right inferior turbinate, middle turbinate and the nasal septum in right nasal cavity with purulent discharge on nasal endoscopic finding.
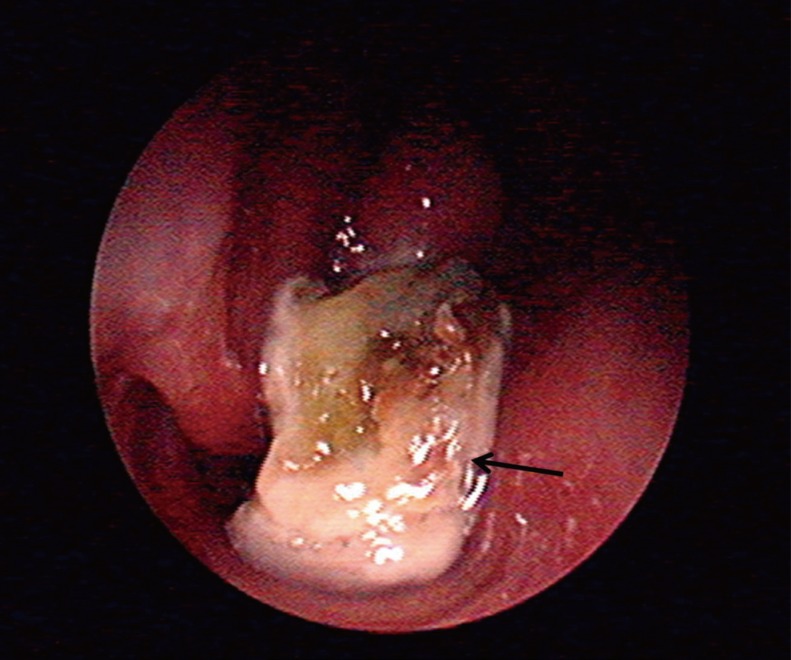
Fig. 2
The axial (A) and coronal (B) paranasal sinus computed tomography scans showing calcified ring lesion (arrow) in the right nasal cavity and bilateral maxillary sinusitis.
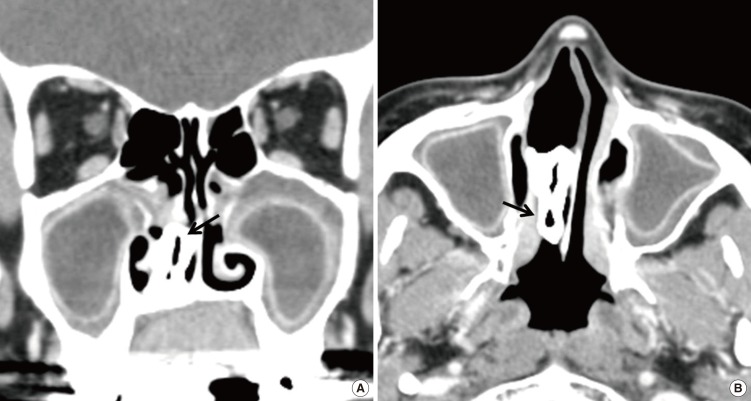
Fig. 3
The microscopic findings. (A, B) A degenerated wall of plant (vegetable matter) is surrounded by calcified amorphous material (H&E, ×40 and ×400, respectively). (C-E) The wall of plant is positive for both periodic acid Schiff and alcian blue pH 2.5 stains, but negative for Van Gieson stain (×200, respectively).




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download