This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
To investigate the aided benefits, speech recognition in quiet and in noise, change in hearing and subjective report of satisfaction on mixed hearing loss adults implanted with Vibrant Soundbridge (VSB) middle ear implant.
Methods
Eight Cantonese speaking adult patients with mixed hearing loss were enrolled in a single-subject, repeated measures prospective study design. Audiometric testing, including air and bone conduction and word recognition under sound-field were conducted before surgery. Device activation was arranged 8 weeks after operation. Audiometric testing was taken to evaluate the change in hearing. Patients were asked to wear the device and come back for fine tuning as needed. Outcome measurements were undertaken at 3 and 6 months after device activation. The outcome measures included sound-field thresholds, Cantonese Hearing in Noise Test (CHINT), Abbreviated Profile of Hearing Aid Benefit (APHAB) and International Outcome Inventory for Hearing Aids (IOI-HA).
Results
The application of the VSB improved the aided thresholds and improved speech intelligibility in quiet and noise without significant changes in hearing thresholds.
Conclusion
VSB is considered as a safe, effective and reliable auditory rehabilitation option for Cantonese speaking adults with mixed hearing loss.
Keywords: Mixed hearing loss, Middle ear implant, Vibrant soundbridge
INTRODUCTION
Although recent conventional hearing devices have improved technically, there are still restraints avoid satisfactory fittings. The limitations may include sound distortion, irritation of the ear canal by ear-mold or tubing, acoustic feedback, occlusion and discomfort due to plugging up of the ear by the device.
The percutaneous Bone Anchored Hearing Aid (BAHA) first introduced in 1977 is an excellent alternative hearing prosthesis for patients who cannot wear a conventional external hearing device (
1). The BAHA hearing system conducts sound directly to the functioning cochlea, bypassing the ear canal and the middle ear system. This allows the cochlea to be stimulated while maintaining ventilation of the external and middle ear system. Over the past decades, the outcomes of BAHA on patients with mixed hearing loss (MHL) have been positively reported worldwide (
2-
4). However, disadvantages of the BAHA hearing system include risk of adverse skin reaction, risk of poor osseo-integration, consistent maintenance and care of the abutment area.
The Vibrant Soundbridge (VSB) manufactured by MED-EL (Innsbruck, Austria) is a partly implantable hearing aid that became available in 2007. The VSB is another feasible rehabilitation option for adults with mixed hearing loss who cannot be fitted with a conventional external hearing aid. Studies results supported that VSB was a promising alternative for this group of patients (
5,
6) However, no previous study has evaluated the efficacy of the VSB on the Chinese population, who speak in tonal language such as Cantonese. The applicability of VSB for this population is important to know, as Cantonese is the 16th most commonly spoken language in the world (
7). Current available results from non-Cantonese speaking subjects may not be applicable to patients who speak in a tonal language such as Cantonese. The aim of the present study was to evaluate the efficacy and benefits of VSB in Cantonese speaking adults with mixed hearing loss.
MATERIALS AND METHODS
Subjects
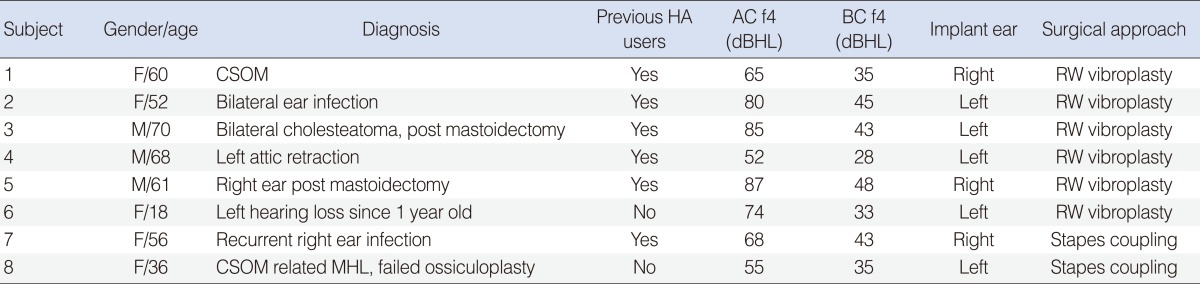
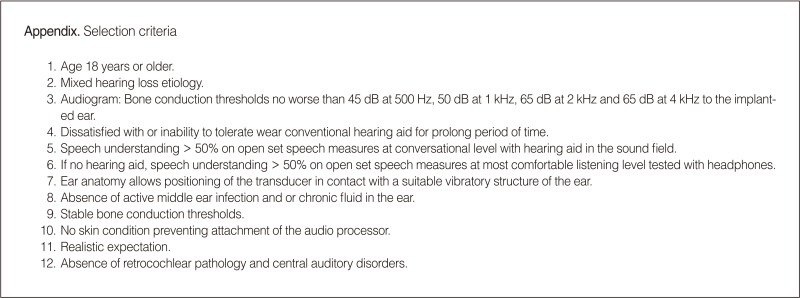
Between June 2010 and February 2011, eight adult patients with mixed hearing loss were implanted with the VSB middle ear implant at the Prince of Wales Hospital, Hong Kong Special Administrative Region of China. Selection criteria for patients used are listed in the
Appendix. The eight patients were three males and five females with range from 18 to 70 years (mean±SD, 52.7±17.5 years). The average air conduction and bone conduction hearing thresholds across the implanted side at 500 Hz, 1 kHz, 2 kHz, and 4 kHz were 71 dBHL and 39 dBHL respectively. Six patients were experienced hearing aid users with an average hearing aid experience of 5.3±3.0 years. Five and three patients received left ear and right ear implants, respectively. The floating mass traducer (FMT) was coupled on the round window vibroplasty for six patients and was clipped on the stapes for two patients. The demographics and pathologic cause are listed in
Table 1.
Ethics approval
The investigational plan was approved by the local ethics committee (Ref No, CRE-2009.252). Informed consent was obtained from the patients and the principles outlined in the Declaration of Helsinki were followed.
Study design and statistical analyses
Each subject served as his/her own control in this prospective, single subject repeated measures study design. Wilcoxon matched-pairs signed-ranks test was used to test for significant differences at the 0.05 level on pre- and post bone conduction thresholds, sound field thresholds, speech reception thresholds (SRT) both in quiet and in noise prior to the operation, and 3 months and 6 months after device activation. In this paper, the preoperative data and 3 months and 6 months post-fitting interval data was used for statistical analyses.
Equipment
VSB middle ear implant
The system comprised of two parts, the external audio processor (AP) and an internal Vibrating Ossicular Prosthesis (VORP), which together convert sound in the environment into a vibratory signal delivered to the inner ear. The AP contains a microphone, which picks up sound and speech from the environment and converts it into a signal that can be transmitted across the skin to be received by the implanted internal receiver of the VSB. The implantable part consists of an internal coil, a magnet to hold the audio processor over the implant, a demodulator, a conductor link and a FMT. The FMT can be coupled to either the ossicular bones or to the round window.
Procedure
Preoperative assessment
Preoperatively, all subjects underwent comprehensive audiological and medical evaluations, including pure tone audiometry, sound field audiometry (with warble tones), speech audiometry, computed tomography of temporal bones and magnetic resonance imaging. All audiometric testing was performed in a standard audiometric booth at the Audiology Centre of the Prince of Wales Hospital. Air conduction thresholds were obtained at 0.25, 0.5, 1, 2, 4, and 8 kHz and bone conduction thresholds at 0.5, 1, 2, and 4 kHz. Speech recognition in quiet and in noise was measured by the Cantonese Hearing in Noise Test (CHINT) (
8). Unaided speech thresholds were evaluated in quiet in three conditions: speech front (SF), speech implant side or speech ipsilateral (SI) and speech at non-implant side or speech contralateral (SC). The speech tests were also evaluated at a fixed level of 65 dB (A) of noise in three different noise conditions. The speech signal was always presented from the front (0
0 azimuths). The noise was presented either in the front (NF), or from the implant side or noise ipsilateral (NI) or noise from the non-implant side or noise contralateral (NC). If a patient had better hearing in the non-implant ear, the non-implant ear would be occluded during testing to minimize the involvement of the non-test ear via air conduction. The equipment used included the GSI clinical audiometer (Grason-Stadler, Eden Prairie, MN, USA) with telephonic headphones and the Maico HINT system (the non-test ear via air conduction). The equipment used included the GSI clinical audiometer. During sound field testing and the speech testing, the subjects were positioned one meter away from the speaker. Apart from above measures, all subjects who were hearing aid users were also asked to fill in the Chinese version of the Abbreviated Profile of Hearing Aid Benefit (APHAB-CH) and the International Outcome Inventory of Hearing Aid (IOI-HA) to compare the performance between hearing aid and VSB.
APHAB-CH
The APHAB-CH is a Chinese self assessment inventory first described in 1995 to evaluate the disability associated with hearing loss and the reduction of the disability with amplification (
9). The validated Chinese version of APHAB was used in the present study (
10). The APHAB comprises 24 items in four subscales: ease of communication (EC), background noise (BN), reverberation (RV) and aversiveness of sound (AV). All items are statements about communication difficulties in daily life and respondents are asked to indicate their agreement with each statement on a seven-point scale. The mean rating for the six items in each subscale constitutes the subscale score, and the global APHAB score is computed by taking the mean of EC, BN, and RV subscales. Subjects were asked to complete the inventory at baseline, before implantation based on their experience with their hearing aid if any and then after 3 months and 6 months of use of the VSB.
IOI-HA-Chinese version
IOI-HA is a brief seven-item questionnaire designed to evaluate the effectiveness of hearing aid treatment in everyday life. The aspects examined are: 1) hearing aid use (Use), 2) benefit (Ben), 3) residual limitation in activity (RAL), 4) satisfaction (Sat), 5) residual participation restriction (RPR), 6) impact on others (Ioth) and 7) quality of life (QoL). The validated Chinese version of the IOI-HA was used in the present study (
11). The IOI-HA questionnaire involved the performance rating on a five-point scale.
Operation
Vibroplasty technique
This approach is suitable for patients without a working ossicular chain. We performed the operation under general anesthesia with facial nerve monitoring. Post-auricular incision was employed. For patients with wall-down mastoidectomy done before the surgery, we carefully elevated the meatal flap and exposed the round window by adequate inferior canal drilling. For patients without wall-down mastoidectomy done before the surgery, we approached the round window by posterior tympanotomy approach as stated above. When the round window niche was identified, the overhanging bony lip of the round window niche was removed by drilling. A small bony well was drilled at the hypotympanium region next to the round window area to harbor the FMT. A layer of perichondium was placed on the round window membrane, then the FMT was placed on the perichondrium and coupling with the round window. The coupling system was stabilized by addition perichondrium packing around the FMT. The VORP was fixed into the bony well created in the temporal region by non-absorbable stitches.
Stapes coupling technique
This approach is suitable for patients with functioning stapes and the anatomy of stapes allows a safe and stable coupling. We performed the surgery under general anaesthesia via the posterior tympanotomy approach. Left cortical mastoidectomy was first performed. The facial recess was opened with preservation of chorda tympani and facial nerve. Intra-operation facial nerve monitoring was needed throughout the drilling to prevent facial nerve injury. The facial recess was gradually enlarged by a diamond burr until the whole stapes suprastructure and the round window niche were visible. The tympanic membrane was kept intact throughout the surgery. Copious irrigation was needed to remove the retained blood clot and bone dust. The normal mobility of stapes was confirmed with the gentle needle palpation and the presence of round window reflex. The claw of the FMT was fashioned so as to allow secure crimpling onto the stapes head. The stability of the whole FMT-stapes system was confirmed with gentle needle palpation. VORP was fixed into the bony well created in the temporal region by non-absorbable stitches.
For both surgical techniques, intraoperative electrocochleography (ECochG) was performed using a GSI Audera evoked potential system (Grason-Stadler). Electrodes were placed on the promontory and measurements were performed before closing up. Alternating tone pips at 2 kHz were delivered to the implant via a custom-made audio processor. A series of ECochG was measured to ensure that the ECochG threshold was matched with the subject's pure tone bone-conduction threshold at 2 kHz.
The average surgery time for each patient was 3.3 hours (200±63.4 minutes). There were no intra-operative and postoperative surgical complications encountered for any patient. The device was activated 8 weeks after surgery and the Amade audio processor (MED-EL) was programmed with CONNEXX 6.1.1 software equipped with the Symfit database Rev. 5.0. The default Desired Sensation Level (DSL) amplification strategy was applied during first fit and the patients returned for a review and fine-tune twice at 2 week intervals until the most comfortable self-evaluated listening level was reported by the patients.
Postoperative assessment
Three months and 6 months after activation of the implant, patients were asked to come back for postoperative assessment. They underwent pure tone audiometry, sound field testing and CHINT testing with the device turned on. The same test equipment and materials as those employed in the preoperative assessment were used during testing.
RESULTS
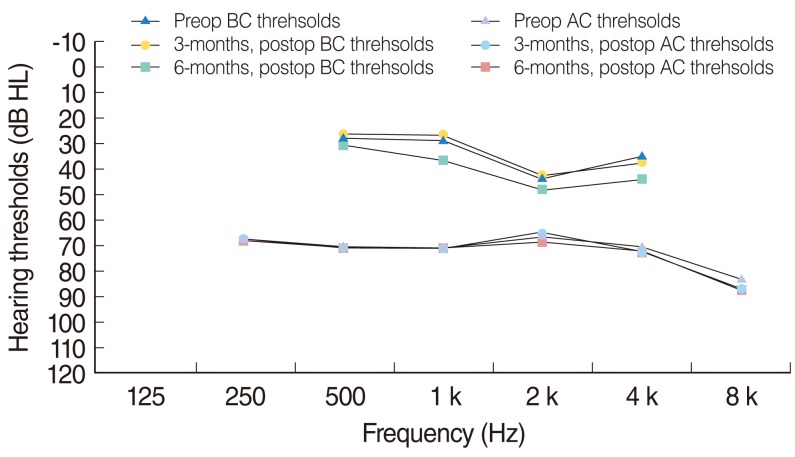
Pre- and postoperative bone conduction thresholds
Preoperative mean bone conduction thresholds at 0.5, 1 and 2 kHz were 27.5 dB. Postoperative mean bone conduction and bone conduction thresholds evaluated at 3 months and 6 months after activation of the implant were 26.3 dB and 30.6 dB, respectively (
Fig. 1). The preoperative and postoperative bone conduction thresholds are shown in
Fig. 1. There was no obvious change in any frequency.
Drop out case
Subject 2 suddenly experienced no sound from the VSB 2 months after activation of the implant. The Amade audio processor was checked and confirmed to be functioning properly. An indirect Vibrogram test and reverse transfer function (RTF) were carried out. The results were not conclusive and a revision surgery is under consideration to examine the positioning of the FMT. Thus, the results of seven patients are presented hereafter.
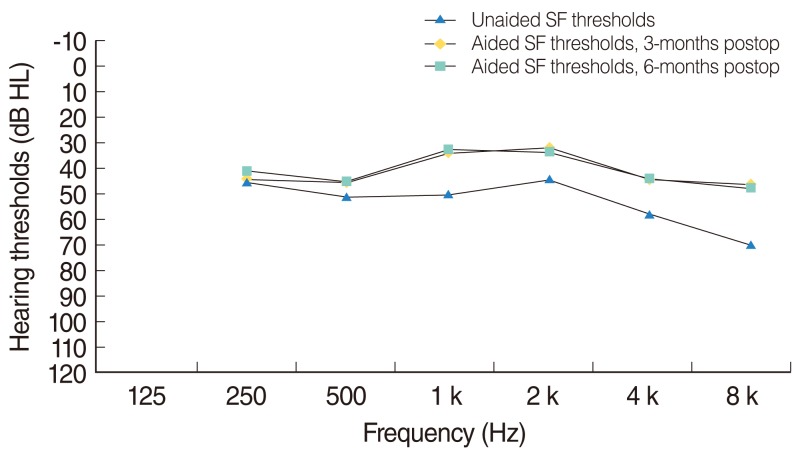
Functional gain improvement
Fig. 2 shows the functional gain at the frequencies 250 Hz to 8 kHz. The functional gain produced by the VSB was determined by differences of the aided thresholds (VSB on) and the unaided thresholds (VSB off) obtained in the sound field with warble tones. The non-implant side was plugged and muffed during testing. The average functional gain at 0.5, 1, and 2 kHz were both about 11 dB evaluated at 3 and 6 months after activation of the implant.
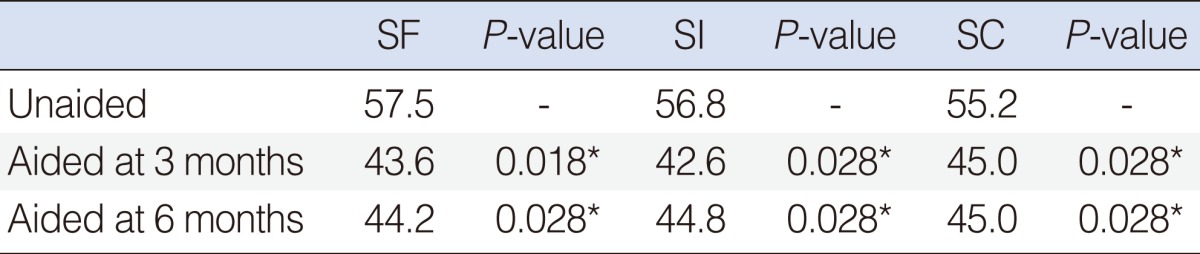
Speech reception threshold (SRT) in quiet
Table 2 represented the SRTs of the adults in quiet when the speech presented in front, implant side and non-implant side. A decrease in SRT reflected an improvement in speech recognition and was defined as a positive outcome. As shown in
Table 2, the use of VSB evaluated at 3 months and 6 months after implant activation produced a significant improvement of over 10 dB on speech recognition thresholds in quiet at different speech locations when compared with unaided conditions (
Table 2). However, the change in SRT at all conditions was all statistically not significant between aided at 3 months and aided at 6 months conditions.
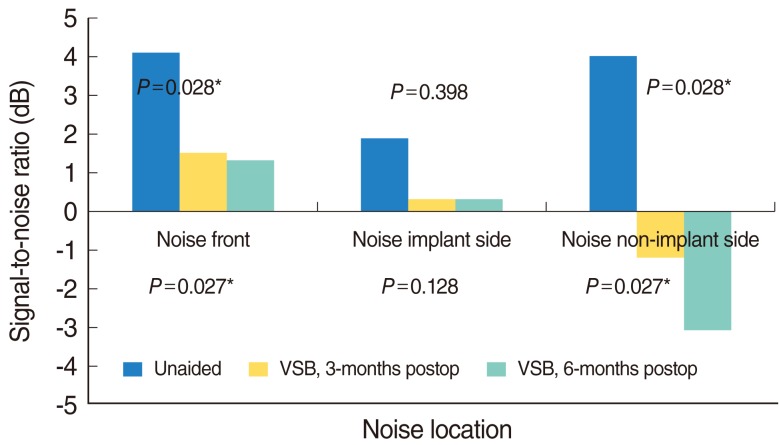
Speech reception threshold (SRT) in noise
Fig. 3 summarizes data concerning SRT in noise, presented on the implant side and non-implant side, as signal-to-noise ratios (SNRs). The speech recognition in noise using the VSB was significantly better in comparison to the unaided conditions at noise front and noise at non-implant side conditions in comparison to unaided mode (Wilcoxon signed rank test,
P=0.028 at 3 months and
P=0.027 at 6 months). All subjects demonstrated an increase in speech understanding with the VSB, the SNR improvement of maximum 2.8 dB at noise front, 1.6 dB at noise ipsilateral and 7.1 dB at noise contralateral conditions evaluated 6 months after device activation.
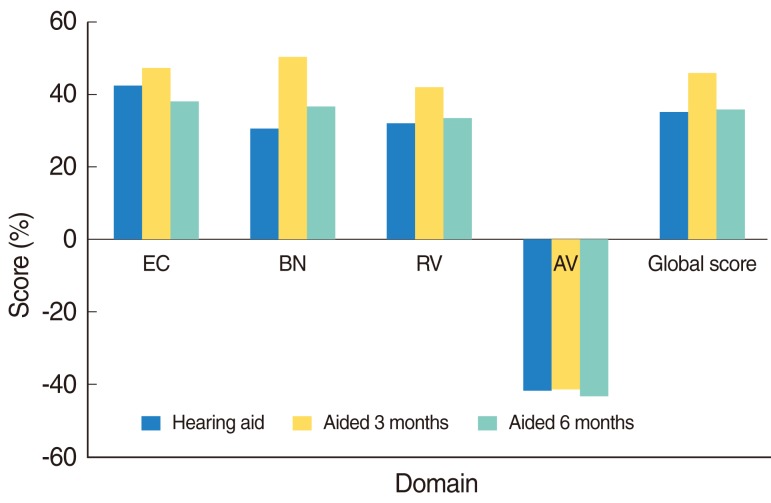
APHAB
The average scores on the four domains (EC, BN, RV, and AV) for VSB are given in
Fig. 4. The global score for the APHAB with hearing aid and VSB at 3 months and 6 months were 45%, 34%, and 36% respectively. The Wilcoxon signed rank test revealed statistically no significant difference between the results (
Fig. 4).
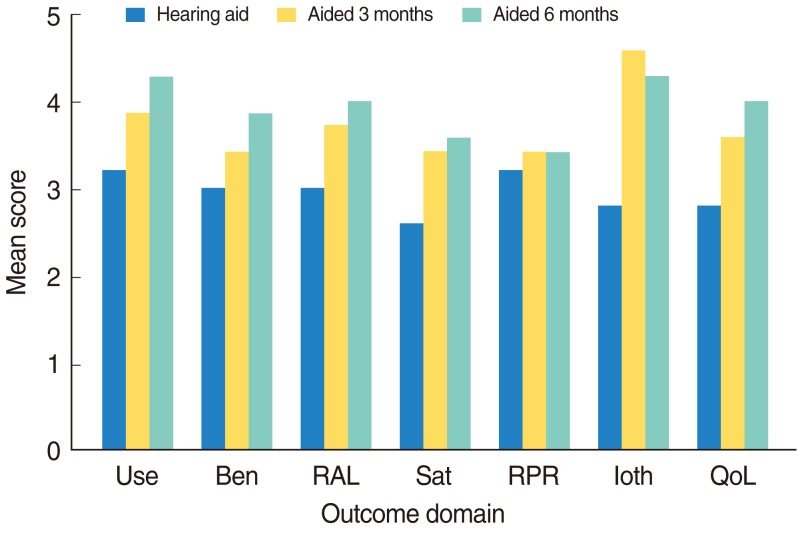
IOI-HA questionnaire
For the seven IOI-HA questions, a score of five indicated the best result and a score of one indicated the worst. The group means score with the conventional hearing aid; VSB at 3 months and VSB at 6 months were 2.9, 3.7, and 3.9, respectively. However, the Wilcoxon signed rank test revealed statistically no significant difference between the results (
Fig. 5).
DISCUSSION
To our knowledge, this is the first report of application of middle ear implant on Chinese adults with mixed hearing loss in Asia. The purpose of the study was to evaluate the efficacy and benefits of VSB case on Cantonese speaking mixed hearing loss adults. Preliminary data from the existing patients suggest that VSB is a safe and effective treatment option for adults with moderately severe mixed hearing loss etiologies. This was evident from the well-preserved hearing thresholds after the middle ear implant surgery and lack of intraoperative or postoperative complications.
From the surgical point of view, the round window vibroplasty approach is the only solution for those patients without functioning ossicles. This is especially common in patients with chronic suppurative otitis media (CSOM) and post mastoidectomy. These disease-related hearing losses are extremely common in Hong Kong and Mainland China. The application of round window vibroplasty in treating these patients has proven to be a cost effective and reliable option in addition to the traditional ossicular surgeries and amplification devices. Moreover, in selected cases, coupling to the functioning and anatomically normal stapes is effective in providing adequate inner ear stimulation. Intraoperation monitoring plays a vital role to ensure the correct FMT-stapes coupling. In a partial eroded stapes or angulated stapes, round window placement will be the first choice.
The performance of the VSB was evaluated by audibility, speech recognition in quiet and in noise and the subjective reports from the subjects. Regarding audibility, VSB provided approximately a maximum 11 dB gain on average. If we take into account the preoperative hearing loss of approximately 70 dBHL, the 11 dB gain offered by VSB improves the perception of the conversational speech. Furthermore, the results indicate that the aided thresholds exceed the bone conduction thresholds by 15 dB at 2 kHz, consistent with previous findings (
12). This means that VSB is not only able to close up the air bone gap, but to provide additional amplification at this particular frequency.
Regarding the speech recognition score, the SRT in quiet was in general 10-14 dB better with the VSB application. The improvement in SRT in quiet is considered robust and significant in the present study. In terms of speech understanding in noise, all subjects demonstrated an increase in speech understanding with the VSB, the SNR improvement of maximum 2.8 dB at noise front, 1.6 dB at noise ipsilateral and 7.1 dB at noise contralateral conditions. Clinically, the relationship between speech intelligibility and SNR is estimated to be 10% speech intelligibility improvement for every 1 dB improvement of SNR, which equates to a 28%, 16%, and 71% speech intelligibly improvement at noise front, noise ipsilateral and noise contralateral conditions, respectively. Thus, the subjects benefit from additional speech understanding provided by VSB.
Regarding the self assessment questionnaires, as only five out of seven patients were previous hearing aid users, the reasons for the preference between hearing aid and VSB were elusive. Surprisingly, even though VSB demonstrated a significant speech intelligibility improvement compared with unaided condition, the subjects reported similar performance between VSB and their own hearing aid. Further research to compare the audiological performance between hearing aid and VSB using more subjects is warranted.
To conclude, this is the first available data in Asia to investigate the efficacy of VSB on Cantonese speaking Chinese adults with mixed hearing loss. The present study results indicate that VSB is a safe and reliable auditory rehabilitation option for adults with mixed hearing loss etiologies. The audiological data demonstrated a significant speech intelligibility improvement of Cantonese tonal languages in both quiet and noise in seven out of eight patients (88%) with the VSB compared with preoperative unaided condition. Further research should heed the suggestion of Sterker et al. (
13) and identity the potential predicators that may affect the satisfaction of the VSB for Chinese patients.
ACKNOWLEDGMENTS
The work was in part funded by MED-EL Hong Kong, Asia Pacific Headquarters. The authors are grateful to Miss Zoe Chan for data collection. The authors alone are responsible for the content and writing of the paper.
References
1. Tjellstrom A, Lindstrom J, Hallen O, Albrektsson T, Branemark PI. Osseointegrated titanium implants in the temporal bone. A clinical study on bone-anchored hearing aids. Am J Otol. 1981; 4. 2(4):304–310. PMID:
6894824.
2. Macnamara M, Phillips D, Proops DW. The bone anchored hearing aid (BAHA) in chronic suppurative otitis media (CSOM). J Laryngol Otol Suppl. 1996; 21:38–40. PMID:
9015447.

3. Soo G, Tong MC, Tsang WS, Wong TK, To KF, Leung SF, et al. The BAHA hearing system for hearing-impaired postirradiated nasopharyngeal cancer patients: a new indication. Otol Neurotol. 2009; 6. 30(4):496–501. PMID:
19415040.
4. Flynn MC, Sadeghi A, Halvarsson G. Baha solutions for patients with severe mixed hearing loss. Cochlear Implants Int. 2009; 10(Suppl 1):43–47. PMID:
19195004.

5. Baumgartner WD, Boheim K, Hagen R, Muller J, Lenarz T, Reiss S, et al. The vibrant soundbridge for conductive and mixed hearing losses: European multicenter study results. Adv Otorhinolaryngol. 2010; 69:38–50. PMID:
20610913.

6. Colletti V, Soli SD, Carner M, Colletti L. Treatment of mixed hearing losses via implantation of a vibratory transducer on the round window. Int J Audiol. 2006; 10. 45(10):600–608. PMID:
17062502.

7. Bauer RS, Benedict PK. Modern Cantonese phonology. 1997. Berlin: Mouton de Gruyter.
8. Wong LL, Soli SD. Development of the Cantonese Hearing In Noise Test (CHINT). Ear Hear. 2005; 6. 26(3):276–289. PMID:
15937409.

9. Cox RM, Alexander GC. The abbreviated profile of hearing aid benefit. Ear Hear. 1995; 4. 16(2):176–186. PMID:
7789669.

10. Kam AC, Tong MC, van Hasselt A. Cross-cultural adaptation and validation of the Chinese abbreviated profile of hearing aid benefit. Int J Audiol. 2011; 5. 50(5):334–339. PMID:
21271802.

11. Cox RM, Stephens D, Kramer SE. Translations of the International Outcome inventory for Hearing Aids (IOI-HA). Int J Audiol. 2002; 1. 41(1):3–26. PMID:
12467365.
12. Beltrame AM, Martini A, Prosser S, Giarbini N, Streitberger C. Coupling the Vibrant Soundbridge to cochlea round window: auditory results in patients with mixed hearing loss. Otol Neurotol. 2009; 2. 30(2):194–201. PMID:
19180678.
13. Sterkers O, Boucarra D, Labassi S, Bebear JP, Dubreuil C, Frachet B, et al. A middle ear implant, the Symphonix Vibrant Soundbridge: retrospective study of the first 125 patients implanted in France. Otol Neurotol. 2003; 5. 24(3):427–436. PMID:
12806295.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download