Abstract
Objectives
Spontaneous nystagmus, which has been considered a typical sign of acute vestibulopathy, has recently been reported in benign paroxysmal positional vertigo involving the lateral semicircular canals (LC-BPPV) without unilateral vestibulopathy (pseudo-spontaneous nystagmus, PSN), but research about its clinical application is still limited. Here we investigate the frequency and characteristics of PSN in LC-BPPV patients, and estimate its prognostic value.
Methods
For 95 patients with LC-BPPV, we examined nystagmus in the sitting position in the clinic with video goggles. Patients were categorized as PSN or non-PSN, according to presence of horizontal nystagmus in the sitting position at diagnosis. The duration of vertiginous symptoms before diagnosis and the duration of treatment were compared between the two groups. The results of video-nystagmography test were reviewed when available.
Results
PSN was examined in 16 (16.8%) patients, all of whose symptoms disappeared immediately after successful repositioning therapy. While the duration of symptoms did not differ statistically between groups (P=0.481), the duration of treatment in the PSN group was significantly longer than in the non-PSN group (P<0.001).
When evaluating dizzy patients, the presence of spontaneous nystagmus suggests to the physician an acute vestibular imbalance, either temporary or permanent, such as vestibular neuritis or Meniere's disease [1]. In contrast, a diagnosis of benign paroxysmal positional vertigo (BPPV) is suggested by a position-induced nystagmus that changes its direction according to head position. As such, spontaneous nystagmus while in the sitting position is not considered as a typical sign of BPPV [2].
However, the occurrence of spontaneous nystagmus in lateral semicircular canal BPPV (LC-BPPV) patients has been reported previously, and recently a new physiological mechanism has been suggested [2-6].
The occurrence of spontaneous nystagmus in BPPV cases has been explained by two pathophysiologic mechanisms. First, when otolithic particles jam in the narrow semicircular canals ('canalith jam') [5], the resulting nystagmus does not show characteristic directional changes in different head positions, but rather a constant direction regardless of head position. The affected patients show a typical nystagmus related to unilateral vestibulopathy, and a decreased caloric response on the affected side. Second, recent studies report the occurrence of spontaneous nystagmus in patients with LC-BPPV in the absence of unilateral vestibulopathy-a condition which has been named 'pseudo'-spontaneous nystagmus, based on the physiologic mechanism of its origin [2-4]. However, the reported incidence of this nystagmus in LC-BPPV is widely variable (40-96%), and its clinical importance is still uncertain.
In this study, we analyzed the characteristics of pseudo-spontaneous nystagmus (PSN) observed in the LC-BPPV patients, and determined whether treatment outcome was affected by the presence of this nystagmus.
From November 2008 to February 2011, 109 LC-BPPV patients were identified out of 428 who were diagnosed as BPPV at our dizziness clinic. Patients with the following known prognostic factors were excluded from the analysis: history of head trauma, multi-canal involvement, previous history of other inner ear disorders (sudden deafness, Meniere's disease, vestibular neuritis, etc.), and other neurological disorders. Among these 109 patients, 14 met the exclusion criteria, leaving 95 to be included in the analysis (M:F, 20:75; age mean±SD, 50.9±13.7 years). The involved side and type of LC-BPPV were determined by head roll and bow-and-lean tests performed in the clinic, monitoring eye movements through video Frenzel goggles (Easy-eyes; SLMed, Seoul, Korea). The ear involved in LC-BPPV was the left in 50 patients and the right in 45. The type of LC-BPPV was geotropic in 40 patients and apogeotropic in 55.
The medical records and video recordings of nystagmus obtained in the outpatient clinic were reviewed. When acquired, results of vestibular laboratory tests using video-nystagmograms were also examined. Along with the gender and age of each subject, the medical history was examined for head trauma, otologic disorders and neurological disorders to determine whether the patient met the exclusion criteria.
The presence of PSN was determined by 2 otolaryngologists by examining close up movies of ocular movements through a video monitor, that were acquired by wearing video Frenzel goggles (SLMed) at the clinic. With the patients in a seated position, spontaneous horizontal nystagmus was observed for at least 10 seconds. Following the results of this initial examination, subjects were divided into PSN and non-PSN groups. Video-nystagmograms showing PSN and positional nystagmus from representative cases are depicted in Fig. 1.
Next, the Dix-Hallpike maneuver was performed to confirm the presence of posterior semicircular canal BPPV, and the supine roll test was conducted. The patient was placed in the supine position with the head centered and the neck muscles relaxed. The examiner then rotated the head 90° to one side, looked for the presence of nystagmus, and returned the head to the central position. After the patient's dizziness ceased, the presence of nystagmus on the other side was examined by rotating the patient's head to the opposite direction. When LC-BPPV was confirmed, the direction of nystagmus in the supine roll test denoted the type of BPPV: geotropic or apogeotropic. The nystagmus directions for the supine position with the head centered (lying-down nystagmus or leaning nystagmus) and for the head bowing position (bending-over nystagmus or bowing nystagmus) were used to confirm the side of involvement according to the relative strength of nystagmus for right and left head turns in the supine roll test [7,8].
The bithermal caloric tests were performed in 9 of the 16 cases in the PSN group. For all nine, canal paresis was less than 20% in both affected and unaffected sides. The remaining 7 patients of the PSN group did not undergo the caloric tests, because the PSN disappeared immediately after the canalith repositioning maneuver and vertiginous symptoms improved dramatically.
For all patients, the barbecue maneuver was performed and instructed about the forced prolonged position with minimal restriction. For cases of the apogeotropic type, the barbecue maneuver was done with the application of vibration on the mastoid tip of the affected side. Subsequently, patients were followed up twice a week with a repetition of the barbecue maneuver (with or without vibrator) until the positional nystagmus completely disappeared. Symptom duration is defined here as the period from the date when the first symptom was self-reported to the date of diagnosis. Treatment duration was taken as the period from the date of diagnosis to the date when positional nystagmus completely disappeared.
Statistical analyses were performed using SPSS ver. 12 (SPSS Inc., Chicago, IL, USA) to compare the gender, age, symptom duration, and treatment duration between groups. The Mann-Whitney U-test and linear regression (stepwise) analysis were used to assess significance, and the criterion for significance was P<0.05.
Among the 95 patients, PSN was observed in 16 (PSN group, 16.8%, 3 men and 13 women), among these, 6 were of the geotropic type and 10 were of the apogeotropic type. The involved side was the left in 6 and the right in 10 patients of the PSN group. The other 79 cases did not reveal PSN (non-PSN group, 17 men and 62 women). Of these, the distribution of BPPV type was geotropic in 34 and apogeotropic in 45. The involved side was the left in 44 and the right in 35 cases. Sex (P=0.085) and the ratio of geotropic to apogeotropic type (P=0.555) did not differ significantly between the two groups. The mean age (±standard deviation) was 57.81±10.80 in the PSN group and 49.53±13.87 in the non-PSN group. The age difference between these groups was significant (P=0.023).
Symptom duration prior to the first visit was 8.00±9.36 days in the PSN group and 7.52±11.73 days in the non-PSN group; these differences were not significant (P=0.481) (Table 1). However treatment duration, which was 10.18±6.34 days in the PSN group and 6.53±6.35 days in the non-PSN group, did differs significantly (P<0.001) as shown in Table 1. When treatment duration was compared in subgroups by BPPV type, a significant difference between PSN and non-PSN groups was revealed for both geotropic and apogeotropic subtypes (P=0.018 and P=0.013, respectively).
For 10 of the 16 cases with PSN, the direction of PSN was concordant with that determined from examination in the lying-down position (supine with head centered). The direction of PSN was discordant with lying-down nystagmus in 3 cases, and 3 patients did not show nystagmus in either lying-down or bending-over positions.
Mean symptom duration and treatment duration were calculated for the 13 patients of the PSN group for which concordance or discordance with the lying-down nystagmus could be determined. The duration of symptoms and duration of treatment were, respectively 7.9 and 10.3 days for the 10 patients showing concordant lying-down nystagmus, and 12.7 and 13.0 days for the 3 discordant patients. These difference were not statistically different among subpopulations (P=0.302 for symptom duration and 0.338 for treatment duration).
To confirm the significance of PSN as a treatment outcome variable, a linear regression analysis was performed using treatment duration as its dependent variable. As independent variables, gender, age, BPPV type and the presence of PSN were chosen for stepwise regression analysis. Among these variables, only the presence of PSN had a significant effect on treatment duration (P=0.040), but gender (P=0.703), age (P=0.440) and BPPV type (P=0.151) were excluded from the variables. When the coefficient of determination is calculated, the adjusted R squared value is 0.036, showing that the impact of PSN on treatment duration is significant but small.
In 2001, Bisdorff and Debatisse [6] first reported spontaneous nystagmus in LC-BPPV patients without canalith jam from 2 cases of the cupulolithiasis type. Towards the end of that decade, its occurrence in both geotropic and apogeotropic types of LC-BPPV had been reported and studies investigating its clinical value performed to a limited extent [2,4,6]. The mechanism of spontaneous nystagmus in LC-BPPV was explained by the fact that maintaining the vertical axis of one's head earth-vertical in a seated posture causes the lateral semicircular canal to be upwardly inclined by about 30°, which results in movement of otolith particles according to the direction of gravity. Since this nystagmus is developed by the specific head position that evokes gravitational movement of otolith particles, and not by imbalance of spontaneous discharge from vestibular afferents, it was called "pseudo"-spontaneous nystagmus [3,4]. The reason why PSN is observed in BPPV involving only the lateral semicircular canal lies in the anatomical features of the canals. While otolith particles within the vertical semicircular canals hardly produce endolymphatic flow in a seated position, endolymph movement within the lateral semicircular canal can be easily obtained by changing the degree of head inclination.
In diagnosing peripheral vestibular disorders, spontaneous nystagmus has been considered the characteristic feature of acute vestibular imbalance, such as in vestibular neuritis and the ictal phase of Meniere's disease. In rare cases of BPPV, spontaneous nystagmus has been observed when a canalith jam occurs. Canalith jam is the state in which otolith particles directly block the endolymphatic flow in the canal, or attached to the cupula causing a fixed position of the cupula regardless of gravity [5,9]. Differently from PSN, spontaneous nystagmus observed due to canalith jam may occur for jams of any semicircular canal, regardless of a change in posture. However, the PSN discussed here is limited to only BPPV involving the lateral semicircular canal. PSN refers to the ocular movement only while in the seated position, and the nystagmus can disappear or change direction according to head posture.
In theory, the direction of PSN is toward the contra-lesional side in the geotropic type and directed ipsi-lesionally in the apogeotropic type, which is the same for lying-down nystagmus. This is because the physiologic mechanism of PSN is identical to that of lying-down nystagmus, and it is only differentiated by the inclination of the lateral semicircular canal [7,8]. Direction of PSN and other positional nystagmus in LC-BPPV is summarized in Table 2. The PSN should disappear with the patient's head inclined forward at 30°, and the direction of the nystagmus change to the opposite side if the head is inclined further forwardly in the pitch plane. Consequently, PSN has been proposed as a clinical sign to determine the involved side of LC-BPPV [3,4]. As the direction of PSN examined in a seated position is always opposite to the direction of the bending-over nystagmus (Table 2), authors suggests to examine nystagmus in the head bowing position when encountering dizzy patients with spontaneous nystagmus to rule out the possibility of LC-BPPV, especially when the patient appeals aggravation/relief of dizziness by positional changes.
In previous studies, the frequency of PSN in LC-BPPV has been reported to vary from 40.1% to 76%, and to increase to 56.2-96% after mild head shaking [3,4,10]. In the present study, this ratio for patients showing PSN was only 16.8%, which is considerably lower than in previous reports. Two situations at the outpatient clinic can account for this difference. First in the present study, the time devoted at the clinic to examining spontaneous nystagmus was relatively short, although it was sufficient to detect apparent nystagmus (minimum 10 seconds). Second, and more important, the head position of the patients was not precisely controlled. The existence and direction of PSN were observed immediately after a patient sat on a chair with his/her head roughly earth vertical. Patients with LC-BPPV naturally prefer to bend their head slightly forward, since this posture minimizes movement of otolith particles in the lateral semicircular canal. Otherwise, patients favor at least having the head fixed in the pitch plane. The occurrence of PSN and its direction were probably affected by head position immediately before and during the examination, which was not precisely controlled in this study. The discordant direction of PSN with lying down nystagmus in three cases might be attributed to this uncontrolled head inclination during the examination. Previous research also supports the idea that the frequency of PSN is subject to head position and movement during the examination [3,4]. Considering the busy clinical setting in medical institutes, we consider the current result more realistic.
Results of the present study confirm that PSN can accompany LC-BPPV, and the presentation of PSN may be associated with longer follow-up duration before cure. Previously reported factors resulting in poorer treatment outcome of BPPV are a history of head trauma, inner ear disorders (e.g., Meniere's disease, vestibular neuritis), gender and age [11,12]. After correcting for these outcome variables, we find that the presence of PSN extended treatment duration. One possible explanation for this is that patients who developed PSN might have relatively more otolithic load in the lateral semicircular canal than those without PSN. In this context, abnormal endolymphatic flow might be produced in patients with PSN with enough strength to evoke nystagmus, even with a small degree of inclination of the head in a seated position. More lithiasis particles might require longer treatment duration to be cleared out from the lateral semicircular canal. Though this explanation is plausible, the small adjusted R-square from the linear regression analysis suggests caution in attributing any prognostic value to this observation, particularly since a previous study revealed no effect of PSN on treatment outcome [10].
In conclusion, horizontal nystagmus in the upright position can be examined in patients with LC-BPPV, and this can possibly be misinterpreted as spontaneous nystagmus representing acute vestibular imbalance. When spontaneous nystagmus is observed in patients suspected to have peripheral vertigo, performing the positional test immediately in the clinic would help provide a correct diagnosis of the cause. Examination of positional nystagmus only in the pitch plane would suffice for screening purposes, and will save time and money by avoiding further vestibular laboratory testing. The prognostic importance of PSN suggested by the current study is still an issue to be clarified in future research.
ACKNOWLEDGMENTS
This work was supported by the Hallym University Medical Center Research Fund (grant no. 01-2008-05).
References
1. Hamid M. Medical management of common peripheral vestibular diseases. Curr Opin Otolaryngol Head Neck Surg. 2010; 10. 18(5):407–412. PMID: 20827085.

2. Asprella Libonati G. Diagnostic and treatment strategy of lateral semicircular canal canalolithiasis. Acta Otorhinolaryngol Ital. 2005; 10. 25(5):277–283. PMID: 16602326.
3. Califano L, Melillo MG, Mazzone S, Vassallo A. "Secondary signs of lateralization" in apogeotropic lateral canalolithiasis. Acta Otorhinolaryngol Ital. 2010; 4. 30(2):78–86. PMID: 20559477.
4. Asprella-Libonati G. Pseudo-spontaneous nystagmus: a new sign to diagnose the affected side in lateral semicircular canal benign paroxysmal positional vertigo. Acta Otorhinolaryngol Ital. 2008; 4. 28(2):73–78. PMID: 18669071.
5. Epley JM. Human experience with canalith repositioning maneuvers. Ann N Y Acad Sci. 2001; 10. 942:179–191. PMID: 11710460.

6. Bisdorff AR, Debatisse D. Localizing signs in positional vertigo due to lateral canal cupulolithiasis. Neurology. 2001; 9. 57(6):1085–1088. PMID: 11571338.

7. Koo JW, Moon IJ, Shim WS, Moon SY, Kim JS. Value of lying-down nystagmus in the lateralization of horizontal semicircular canal benign paroxysmal positional vertigo. Otol Neurotol. 2006; 4. 27(3):367–371. PMID: 16639276.

8. Choung YH, Shin YR, Kahng H, Park K, Choi SJ. 'Bow and lean test' to determine the affected ear of horizontal canal benign paroxysmal positional vertigo. Laryngoscope. 2006; 10. 116(10):1776–1781. PMID: 17003735.

9. von Brevern M, Clarke AH, Lempert T. Continuous vertigo and spontaneous nystagmus due to canalolithiasis of the horizontal canal. Neurology. 2001; 3. 56(5):684–686. PMID: 11245729.

10. De Stefano A, Kulamarva G, Citraro L, Neri G, Croce A. Spontaneous nystagmus in benign paroxysmal positional vertigo. Am J Otolaryngol. 2011; May-Jun. 32(3):185–189. PMID: 20392532.

11. Brandt T, Huppert D, Hecht J, Karch C, Strupp M. Benign paroxysmal positioning vertigo: a long-term follow-up (6-17 years) of 125 patients. Acta Otolaryngol. 2006; 2. 126(2):160–163. PMID: 16428193.

12. Del Rio M, Arriaga MA. Benign positional vertigo: prognostic factors. Otolaryngol Head Neck Surg. 2004; 4. 130(4):426–429. PMID: 15100638.

Fig. 1
Video nystagmograms showing pseudo-spontaneous nystagmus (PSN) and positional nystagmus in representative cases of LC-BPPV. (A) A case of geotropic type involving the right ear. Left-beating PSN (7 degree/second) is recorded. In supine roll test, geotropic nystagmus is recorded in the head right (18 degree/second, directing to the right side) and head left (13 degree/second, direction to the left side) position. When the positional test is performed in the pitch plane, lying-down nystagmus and bending-over nystagmus are directed to the same (left-beating, 8 degree/second) and to the opposite direction (right-beating, 8 degree/second) as the PSN, respectively. (B) A case of apogeotropic type involving the left ear. Left-beating PSN (8 degree/second) is recorded. Apogeotropic type nystagmus is examined in the supine roll test (left-beating, 146 degree/second with the head turned to the right; right-beating, 57 degree/second to the left). In the pitch plane, the direction of evoked nystagmus was the same as the direction for PSN in the lying down position (left-beating, 79 degree/second), and to the opposite direction in the bending over position (right-beating, 47 degree/second). LC-BPPV, benign paroxysmal positional vertigo involving the lateral semicircular canal; LH, horizontal component of nystagmus measured on the left eye; LB, nystagmus of which fast component directing to the left side of the patient; RB, nystagmus of which fast component directing to the right side of the patient.
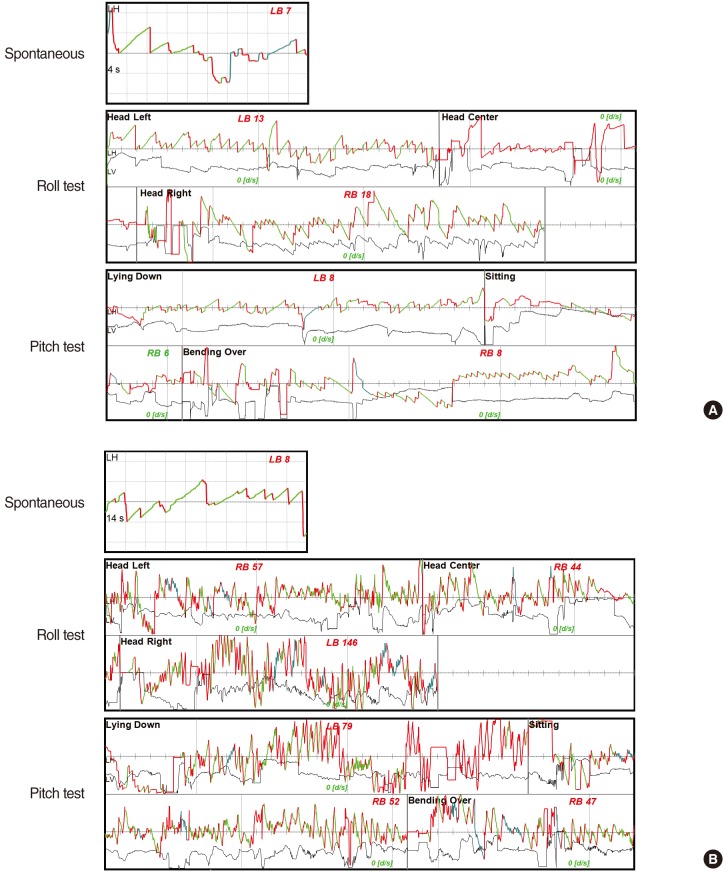
Table 1
Symptom duration and treatment duration in LC-BPPV patients according to the existence of PSN
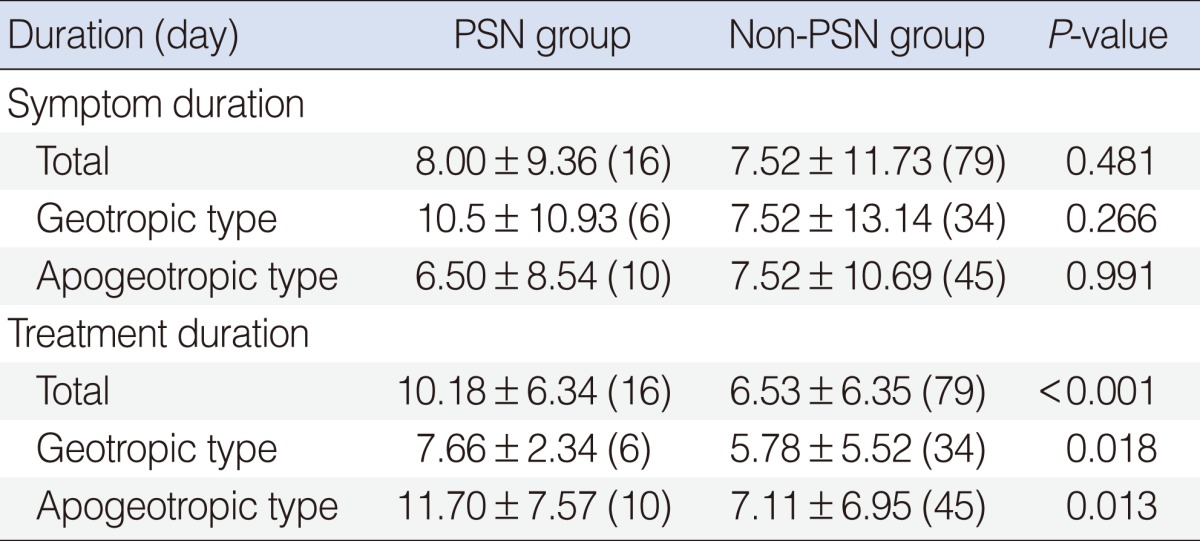
Table 2
Direction of PSN and positional nystagmus in LC-BPPV
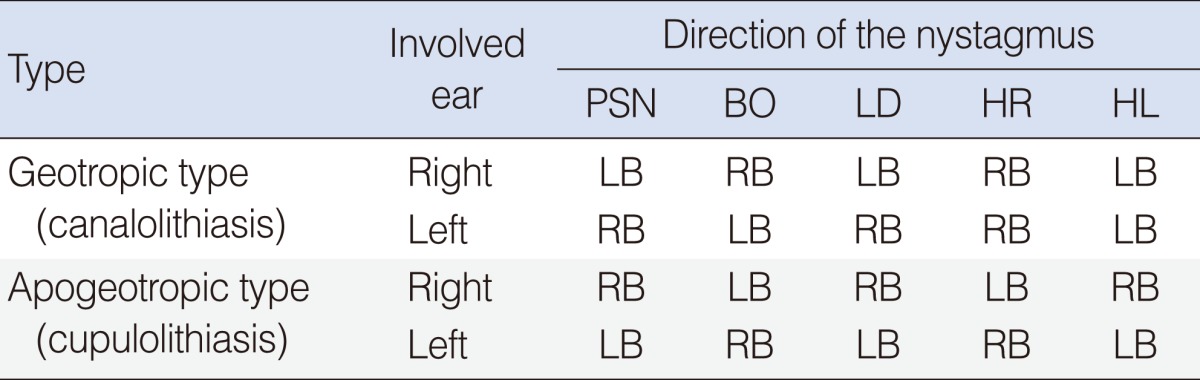
PSN, pseudo-spontaneous nystagmus; LC-BPPV, benign paroxysmal positional vertigo involving the lateral semicircular canal; BO, bending-over nystagmus examined in the head bowing position; LD, lying-down nystagmus examined in the supine position with the head centered; HR, nystagmus examined in the supine position with head turned to the right; HL, nystagmus examined in the supine position with head turned to the left; RB, nystagmus of which fast component directing to the right side of the patient; LB, nystagmus of which fast component directing to the left side of the patient.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download