Abstract
Objectives
Currently established first line therapy of acute (presumed bacterial) rhinosinusitis (ARS) consists of 10 to 14 days of oral amoxicillin or cephalosporins. This study compared the clinical efficacy and tolerance of cefcapene pivoxil (CP) and amoxicillin-clavulanate (AMC) in patients with ARS.
Methods
A randomized, open labeled, double-blinded trial of ARS patients over 15 years of age was performed. Patients diagnosed with ARS received paranasal sinus X-rays and nasal endoscopies and 2 weeks of either CP (150 mg, 3 times/ day) or AMC (625 mg, amoxicillin 500 mg, 3 times/day). All patients revisited the clinic on days 7, 14, and 28 for evaluation of changes in symptoms, endoscopy, and monitoring of any adverse reactions. Demographics, clinical characteristics and drug efficacy were also compared between the two groups.
Results
Among the 60 initially enrolled patients (CP 30, AMC 30), 5 patients in the CP group and 6 in the AMC group were excluded due to poor compliance. There were no significant differences in demographic data including age, sex, initial signs and symptoms, endoscopic and X-ray findings between the two groups. Rates of improvement after 2 weeks were 96% and 95.8% in the CP and AMC group, respectively. Sinus symptoms were changed significantly after 2 and 4 weeks, however, there was no difference between groups (P=0.41). The most common adverse reaction was gastrointestinal complication, diarrhea occurred in 1 patient in the CP group and 6 in the AMC group (P=0.04).
Acute (presumed bacterial) rhinosinusitis (ARS) is one of the most common disease for prescribing antibiotics in general practice (1). Although antibiotic prescription should be based on standard bacteriologic studies, this takes additional time causing delay in treatment and clinicians are often confronted to prescribe antibiotics empirically. The most common bacterial pathogens involved in ARS are Streptococcus pneumonia, Haemophilus influenza, and Moraxella catarralis (1, 2). Empirically chosen antibiotics should target these organisms and loco-regional bacterial resistance pattern, disease severity, progression of the disease and recent antibiotic exposure should be considered.
The goal of antibiotic therapy is to eradicate the bacterial pathogens to alleviate symptoms, prevent complications and finally aid in recovering normal sinus physiology.
Cefcapene pivoxil (CP) is a broad spectrum oral ester cephalosporin that has been developed in Japan (3). A recent study showed that 5-day treatment with oral CP was safe and effective for treating group A β-hemolytic streptococcus infection resulting in microbiological and clinical improvement which were equal to a 10-day treatment with oral amoxicillin (3). In clinical setting, concerning about the potential impact of antibiotics on bacterial resistance, selection of antibiotics is the question pressing for serious consideration.
In Korea, many physicians tend to prescribe the amoxicillin/clavulanate or cephalosporin as a first line therapy instead of amoxicillin due to bacterial resistance. To our knowledge, there is no data comparing the clinical efficacy of CP and amoxicillin-clavulanate (AMC) for the treatment of ARS. Therefore, we designed a randomized, open labeled, double-blinded study to compare CP with AMC in terms of clinical efficacy and safety.
A randomized, open labeled, double-blinded study was designed. Patients were randomly assigned to either CP or AMC groups using the table of random sampling numbers: the former received 150 mg tablet three times daily (450 mg/day) and the latter 625 mg tablet three times daily (4:1 form of AMC, Amoxicillin 1,500 mg/day) for 14 days. Usually, 100-150 mg of CP three times a day is prescribed for these cases in our institution. So, we administrated 150 mg of CP three times a day. The patients were blinded to treatment which was allocated by a randomization schedule. Use of antibiotics other than the study drugs was prohibited throughout the study. However, there was no restriction to other symptomatic medications including antihistamines, decongestants, and mucolytics. Any patients who had hypersensitivity to penicillin, cephalosporin and beta-lactam lineage antibiotics or had been on antibiotics 2 weeks before enrollment were excluded from this study. Patients who experienced orbital cellulitis or intracranial extension of the infection or who were required to be hospitalized are considered to have severe disease and are excluded.
The study was approved by the institutional review board of Seoul National University Hospital. All patients were provided with written informed consent before initiation of study.
Between June 2007 and January 2010, patients over 15 years of age with a clinical diagnosis of ARS were recruited from the outpatient clinic of Seoul National University Hospital, Seoul, Korea. The diagnosis of ARS (presumed bacterial) was made based on the guidelines provided by the American Academy of Otolaryngology-Head and Neck Surgery (4). Diagnosis required symptoms consistent with ARS plus objective findings.
Patients with symptoms of ARS that showed the following patterns were included; symptoms present for at least 10 days and up to 28 days; patients with severe disease with presence of nasal purulence for 3-4 days with high fever; and patients whose symptoms initially regress but then worsen within the first 10 days. Symptoms of ARS included at least 2 major symptoms or 1 major plus 2 minor symptoms. Major symptoms consisted of facial pressure/pain, facial congestion, nasal obstruction, purulent nasal discharge, post nasal drip, hyposmia/anosmia and fever, while minor symptoms included headache, mouth odor, fatigue, tooth pain, cough and ear fullness or pain.
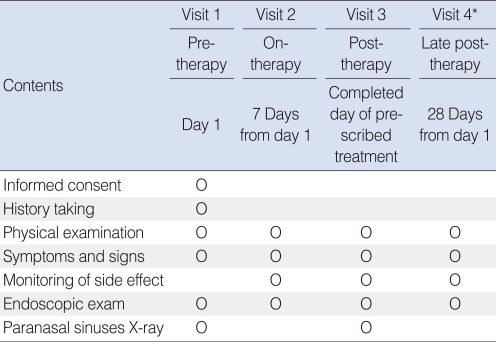
The patients' symptoms were assessed using a scale from 0 to 3 (0=absent, 1=improvement but remained, 2=same as before, 3=aggravated). Nasal endoscopy and paranasal sinuses X-rays (Waters and Caldwell views) were also performed in every patient during the initial visit day for confirmation of the diagnosis and follow up images were performed to monitor progress and check effectiveness. Endoscopic examinations were performed on days 1, 7, and 14 and paranasal sinus X-rays on days 1 and 14 (Table 1). The presence of colored nasal discharge on nasal endoscopy was assigned a score of 3 and 0 if absent. As for sinuses X-rays, presence of air fluid level or partial opacification was scored as 1 and 2 if total opacification.
On each visit, we evaluated symptom improvement, compliance and adverse effects. All patients were instructed to visit the clinic on days 7, 14, and 28 after initial treatment.
Clinical response was classified as remission, improvement, same as before or aggravation. Remission was defined as resolution of symptoms of ARS and no requirement for additional antibiotics for the treatment of ARS. Improvement was considered to have occurred when all signs and symptoms of ARS present at enrollment were decreased significantly. Same as before was defined when all signs and symptoms of ARS continued without change and aggravation was the status when all signs and symptoms were more deteriorating, thus required for additional antibiotics for the treatment.
At visit 3 (day 14), the overall clinical response was grouped as success (cases with remission or improvement) or failure (cases with same as before or aggravation of symptoms). At visit 4 (day 28), the clinical response was also defined as success (continued remission or improvement) or failure (same as before or reappearance of signs and symptoms and need for antibacterial therapy). Relapse was defined as the reappearance of clinical signs and symptoms at day 21 or 28 in a patient who showed improvement till day 14 and persistent infection was defined as sinus symptoms continuing at day 21 or 28 without experiencing the improvement of symptoms.
The primary end point was determined based on the symptoms and endoscopic finding on the second and fourth week. The secondary end point was based on adverse reaction.
Demographics and clinical characteristics of the study groups were compared using the Fisher exact test or the Mann-Whitney U test. The Fisher exact test was used to compare radiographic findings, adverse effects and the use of concomitant medications between groups. Differences in treatment duration and outcomes between groups were analyzed using the Mann-Whitney U test. Values were considered statistically significant if P<0.05. All analyses were performed using SPSS ver. 12 (SPSS Inc., Chicago, IL, USA).
Of the 60 enrolled patients, 49 patients (81.7%) completed the trial. 5 patients in the CP group and 6 in the AMC group were excluded due to poor compliance, self discontinuation or adverse reactions. There was no significant difference regarding treatment compliance (83.3% vs. 80.0%).
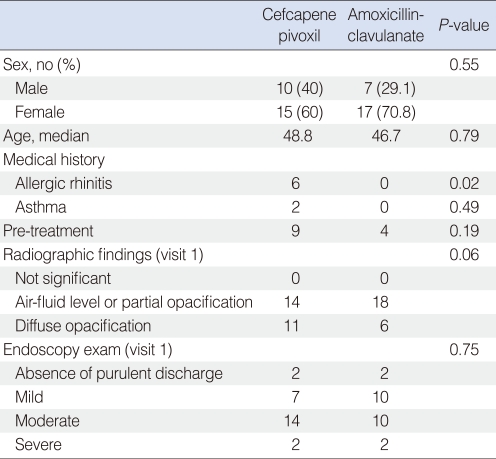
With the exception of history of allergic rhinitis, the two groups did not show any difference in terms of sex, age, number of days with rhinosinusitis-related symptoms, pre-treatment duration, prescribed medications before enrollment, initial radiographic findings and clinical findings for purulent discharge from the ostiomeatal unit from endoscopic findings, initial symptoms, and the additional use of concomitant medication (Table 2).
The most common symptoms in both groups were nasal discharge/postnasal drip (100% in both groups), nasal obstruction (96% vs. 86%), cough (64% vs. 75%), and hyposmia (72% vs. 58%).
The most common findings on sinus radiographs taken during the first visit were 'air-fluid level or partial opacification' in both groups and there were no statistically significant differences in the initial radiographic findings between the two groups. Six patients from the CP group and 1 patient from the AMC group used concomitant medications which included mucolytics, antihistamines, oral decongestants or intranasal corticosteroid sprays.
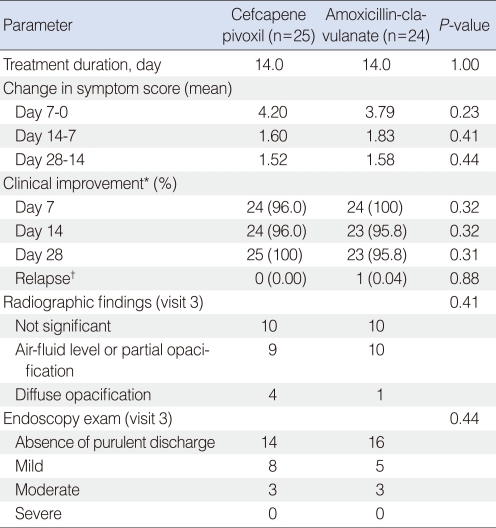
On their second visit (day 7), complete remission of symptoms or partial improvement of symptoms was seen in 96.0% and 100.0% of patients in the CP and AMC groups, respectively; on the third visit (day 14), 96.0% and 95.8% of the patients in each group showed improvement; and on the fourth visit (day 28), 100% and 95.9% showed improvement compared to pretreatment. The change of symptom scores was statistically significant on days 7, 14, and 28 in both groups (P<0.001), however there was no difference between the two groups in any visit period. Relapse was seen in 1 patient in the AMC group (Table 3).
The most common findings on sinus radiographs taken during the third visit were 'not significant' in both groups and most of the patients having diffuse opacification on X-ray initially showed improvement on follow up X-ray.
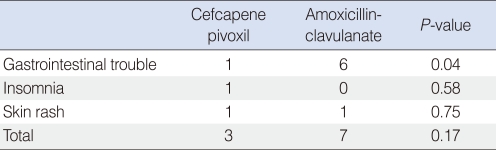
The most commonly reported adverse event in the CP and AMC groups was GI trouble, especially diarrhea (4.0% vs. 25.0%, respectively; P=0.04) (Table 4). Other adverse reactions included insomnia, rash and itching in the CP group and epigastric pain, constipation and rash in the AMC group. No major side effects were identified during the study.
Extended-spectrum cephalosporins (e.g., cefuroxime azetil, cefpodoxime prozetil, and cefdinir) have been demonstrated to be effective against organisms isolated in ARS (Streptococcus pneumonia, Haemophilus influenza, and Moraxella catarrhalis) (1, 2).
The reasons why we compared the efficacy of AMC to CP is that the key offending organism is commonly amoxicillin-resistant (5). In our randomized, double-blinded, open label trial, we aimed to compare the efficacy of CP and AMC in the treatment of ARS.
Our results regarding frequent nasal symptoms were similar with those of Tantimongkolsuk et al. (6), although it was performed in children with rhinosinusitis, in which rhinorrhea (95.0%), cough (91.0%), and nasal blockage (74.0%) were the most frequent presenting symptoms. A study regarding the signs and symptoms of ARS suggested that patient-reported symptoms such as a previous common cold or facial pain do not help to distinguish a bacterial infection from a viral infection, thus it could not be a reliable marker to warrant the prescription of antibiotics. Moreover, they have reported the presence of purulent nasal discharge is also insufficient to justify antibiotic treatment (4, 7). Thus, in our study, the diagnosis of ARS was based on clinical symptoms and signs together with radiographic imaging.
Most of the patients in both groups were improved with 2-week antibiotic medication and there was no statistical significance in improvement rate between groups (P=0.88). One patient in AMC group showed improvement at the day 7 and 14 day follow-ups, after which his symptoms became aggravated at the day 28 follow-up. Interpreting clinical efficacy demands caution because distinguishing patients with relapse from those with persistent infection can be difficult. In this case, being categorized as 'relapse' seems to be justified based on the fact that having taken improvement period before aggravation of symptom.
According to previous published guideline on ARS, radiographic imaging is not routinely recommended in patients who meet the diagnostic criteria for acute rhinosinusitis (8). This is because clinical criteria itself has comparable accuracy to sinus radiography, and therefore radiographs are reserved to patients with co-morbidities that predisposes them to complications including diabetes, immune compromised state, or past history of facial trauma.
It is well known that the time needed for outstanding changes to occur in plain film is likely to be much longer than the time of symptomatic improvement. Therefore, following up the patient with plain sinus films, although certainly less costly, do have limitations and are generally less reliable than CT or MR images. Nevertheless, it might be adequate for an ARS study in terms of confirmation of the diagnosis with definite air fluid level and partial or diffuse opacification, detection of any abnormality located in paranasal sinuses roughly, comparability of the films taken during different time.
The most common finding present in the paranasal sinus radiographs performed on the first visit was 'air-fluid level' or 'partial opacification' in both CP and AMC groups (56% vs. 58.3%, CP vs. AMC). However, 2 weeks later, the most common radiographic finding was 'not significant' in both groups (40% in CP group and 41.7% in AMC group). While 44% of patients in the CP and 25% of the AMC group showed diffuse opacification on radiography on the first visit (day 1), only 16% and 4% of patients showed diffuse opacification on the third visit (day 14). There were no significant differences in terms of radiographic findings between the two groups at any given time point. Among the 11 patients with diffuse opacification on X-rays taken during visit 1 in the CP group, a total of 7 patients showed radiological improvement as 'partial opacification' or 'not significant,' and those were combined with clinical improvement. In the AMC group, all 6 patients having diffuse opacification showed improvement to normal or partial opacification. While improvement of X-ray findings was accompanied by decreased symptoms and signs of ARS in 4 patients, 2 patients failed to go together.
By chance, all patients who had asthma or allergic rhinitis were assigned to one group. Patients used symptomatic medication, 6 patients in CP group and 1 patient in AMC group, which would affect clinical outcomes. Therefore, whether asthma or allergic rhinitis can influence the recovery from ARS could not be evaluated exactly in this study. Even though it is true, since these patients was on the CP treated group in present study, the similar therapeutic results of both drugs suggest that the effectiveness of CP is not inferior to that of the AMC as the first line recommended drug in treatment of ARS.
The most common adverse effect that occurred in this study was GI trouble including diarrhea, epigastric soreness and constipation. A common side effect of antibiotics is diarrhea, which may be caused by the elimination of beneficial bacteria normally found in colon. According to the previous studies, the frequency of diarrhea of patients treated with AMC was reported from 10.9% to 21.0% (9-12). Patients treated with different kind of cephalosporin had a lower rate of adverse clinical events compared to those with amoxicillin-clavulanate (3, 13). In present study, the incidence of diarrhea during treatment with AMC, although it was numerically lower than the previous report, was higher than that with CP.
The limitations of this study include absence of bacteriologic study and small sample size recruited from a single hospital may limit the generalization of the finding. Bacterial cultures are strongly recommended for studies of antibiotic treatment and provide valuable information for any therapeutic trial of ARS, however, there are limitations of bacterial culture that prevent the routine use for antibiotic trials. There is a difficulty in getting the patients to agree with the invasive procedure and many culture methods such as blind nasal swab, nasopharyngeal swab, endoscopically directed cultures of the middle meatus and maxillary sinus tapping have been evaluated and debated whether that method is promising or not to identify the pathogens (14).
This study provides evidence suggesting that CP is as effective as AMC for the treatment of ARS in adults in terms of symptom improvement and relapse. In addition, CP treatment showed superiority to AMC in terms of GI adverse effects.
References
1. Anon JB, Jacobs MR, Poole MD, Ambrose PG, Benninger MS, Hadley JA, et al. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngol Head Neck Surg. 2004; 1. 130(1 Suppl):1–45. PMID: 14726904.

2. Wald ER. Microbiology of acute and chronic sinusitis in children. J Allergy Clin Immunol. 1992; 9. 90(3 Pt 2):452–456. PMID: 1527336.

3. Sakata H. Comparative study of 5-day cefcapene-pivoxil and 10-day amoxicillin or cefcapene-pivoxil for treatment of group A streptococcal pharyngitis in children. J Infect Chemother. 2008; 6. 14(3):208–212. PMID: 18574656.

4. Lanza DC, Kennedy DW. Adult rhinosinusitis defined. Otolaryngol Head Neck Surg. 1997; 9. 117(3 Pt 2):S1–S7. PMID: 9334782.

5. Anon JB, Berkowitz E, Breton J, Twynholm M. Efficacy/safety of amoxicillin/clavulanate in adults with bacterial rhinosinusitis. Am J Otolaryngol. 2006; Jul-Aug. 27(4):248–254. PMID: 16798401.

6. Tantimongkolsuk C, Pornrattanarungsee S, Chiewvit P, Visitsunthorn N, Ungkanont K, Vichyanond P. Pediatric sinusitis:symptom profiles with associated atopic conditions. J Med Assoc Thai. 2005; 11. 88(Suppl 8):S149–S155. PMID: 16856435.
7. Young J, De Sutter A, Merenstein D, van Essen GA, Kaiser L, Varonen H, et al. Antibiotics for adults with clinically diagnosed acute rhinosinusitis: a meta-analysis of individual patient data. Lancet. 2008; 3. 15. 371(9616):908–914. PMID: 18342685.

8. Rosenfeld RM, Andes D, Bhattacharyya N, Cheung D, Eisenberg S, Ganiats TG, et al. Clinical practice guideline: adult sinusitis. Otolaryngol Head Neck Surg. 2007; 9. 137(3 Suppl):S1–S31. PMID: 17761281.

9. Garbutt JM, Goldstein M, Gellman E, Shannon W, Littenberg B. A randomized, placebo-controlled trial of antimicrobial treatment for children with clinically diagnosed acute sinusitis. Pediatrics. 2001; 4. 107(4):619–625. PMID: 11335733.

10. Bottenfield GW, Burch DJ, Hedrick JA, Schaten R, Rowinski CA, Davies JT. Safety and tolerability of a new formulation (90 mg/kg/day divided every 12 h) of amoxicillin/clavulanate (Augmentin) in the empiric treatment of pediatric acute otitis media caused by drug-resistant Streptococcus pneumoniae. Pediatr Infect Dis J. 1998; 10. 17(10):963–968. PMID: 9802654.

11. Poachanukoon O, Kitcharoensakkul M. Efficacy of cefditoren pivoxil and amoxicillin/clavulanate in the treatment of pediatric patients with acute bacterial rhinosinusitis in Thailand: a randomized, investigator-blinded, controlled trial. Clin Ther. 2008; 10. 30(10):1870–1879. PMID: 19014842.

12. Kafetzis DA. Multi-investigator evaluation of the efficacy and safety of cefprozil, amoxicillin-clavulanate, cefixime and cefaclor in the treatment of acute otitis media. Eur J Clin Microbiol Infect Dis. 1994; 10. 13(10):857–865. PMID: 7889960.

13. Henry DC, Kapral D, Busman TA, Paris MM. Cefdinir versus levofloxacin in patients with acute rhinosinusitis of presumed bacterial etiology: a multicenter, randomized, double-blind study. Clin Ther. 2004; 12. 26(12):2026–2033. PMID: 15823766.

14. Benninger MS, Payne SC, Ferguson BJ, Hadley JA, Ahmad N. Endoscopically directed middle meatal cultures versus maxillary sinus taps in acute bacterial maxillary rhinosinusitis: a meta-analysis. Otolaryngol Head Neck Surg. 2006; 1. 134(1):3–9. PMID: 16399172.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download