INTRODUCTION
Continuous positive airway pressure treatment (PAP) is generally considered to be the best treatment for obstructive sleep apnea (OSA) (
1,
2). Its efficacy depends on the patient's willingness to use the device and wear the nasal mask during sleep. Compliance is the main determinant for success in patients who are prescribed PAP therapy. The American Thoracic Society has indicated that the overall compliance rates approach 50% at best (
1), and it has been reported that most patients who discontinue PAP therapy do so within the first few months. Rolfe et al. (
3) reported that 78% of the treatment interruptions took place within two months and 90% took place within four months of the initiation of treatment.
The influence of the upper airway on PAP therapy has recently been studied. We previously reported a correlation between the pressure level of PAP therapy and upper airway narrowing with the intolerance of patients for a high expiratory pressure from the machine (
4). Patients frequently complain of this discomfort during the early phase of PAP therapy. In addition, Sugiura et al. (
5) reported that nasal resistance has a significant effect on the initial acceptance of PAP therapy. The aim of this study was to investigate whether upper airway narrowing can affect the adherence of patients to PAP therapy.
MATERIALS AND METHODS
The patients who were diagnosed to have OSAS by polysomnography and who had started auto-adjusting positive airway pressure (APAP) treatment from March 2005 to March 2006 were enrolled in this study. The patients were referred to our department with complaints of snoring and sleep apnea. Those patients excluded from the study had undergone prior surgery for OSAS or had reduced cardiac function or chronic obstructive pulmonary disease at the time of the study. The study was approved by the institutional ethics committee, and informed written consents were obtained from all the patients included in this study.
Polysomnography (PSG) was performed before starting therapy and only 36 patients who had apnea-hypopnea index (AHI) higher than 15/hr and agreed to start APAP treatment were included in this study. An ENT otolaryngologist evaluated the upper airway prior to the start of the initial sleep study. The patients were regularly followed at three- to four-week intervals. In this study, adherence was defined by continuation of therapy for more than three months. The patients were divided into two groups, that is, the adherent and non-adherent groups.
Evaluation of the pharyngeal inlet
The degree of palatine tonsilar hypertrophy (PTH) was graded using the Friedman's classification as follows: grade 0, surgically removed tonsils; grade I, tonsils within the pillars; grade II, tonsils extending to the pillars; grade III, tonsils beyond the pillars but not to the midline; and grade IV, tonsils extending to the midline (also known as kissing tonsils) (
6). The shape of the oropharyngeal inlet (Orophx) was evaluated with mouth open and without protrusion of the tongue using a modification of Mallampati's technique and was graded as follows: grade I, tonsils, pillars and soft palate clearly visible; grade II, the uvula, pillars and upper pole of the tonsils visible; grade III, only part of the soft palate visible with the tonsils, pillars and the base of the uvula invisible; finally, grade IV, only the hard palate visible.
Evaluation of the nasal pathway
Acoustic rhinometric measurement was performed using the ECCOVISION Acoustic Rhinometer (Model AR-1003; Hood Laboratories, Pembroke, MA, USA) with the patient in the seated position. The minimal cross-sectional area (MCA) was measured, which corresponds to the narrowing at the head of the inferior turbinate (2 cm from the nasal inlet). We evaluated the MCA at the narrow and wide sides of the nasal cavity, respectively, and we calculated the summation of both MCAs.
Severity of the OSA and the APAP level
Before starting the APAP therapy, overnight polysomnography was performed using the Alice3 (Healthdyne Technologies, Marietta, GA, USA) recorder to monitor the electroencephalogram (C3-A2, C4-A1), the left and right electro-oculograms, the electrocardiogram, the chin and anterior tibialis electromyograms, the abdominal and thoracic movements via inductive plethysmography and the nasal oral airflow and the oxygen saturation via pulse oxymetry (SpO2). Apnea was defined as the cessation of breathing for at least 10 sec, and hypopnea was defined as a decrease in airflow of at least 50% or a decrease in the SpO2 of at least 4%, as compared with the baseline. The AHI was calculated, and we obtained other polysomnographic data such as the apnea index (AI) and the lowest O2 saturation. The AHI, the lowest O2 desaturation (minO2) and the Epworth sleepiness scale (ESS) were determined and compared between the two groups.
We prescribed an APAP device that could adjust the PAP level on a minute-by-minute basis within certain ranges around the titration pressure. At every visit after starting the therapy, we checked the data of the patients' use of the device, which had been recorded in the APAP device. The effective pressure levels that eliminated 95% of the apnea and hypopnea events (effPr) were also compared between the two groups.
Statistical analysis
The Mann-Whitney's U test was performed with SPSS ver. 10.0 (SPSS Inc., Chicago, IL, USA) to compare the variables of the two groups. The gender ratios of the two groups were compared with chi-square test. The significance level was set at P<0.05 in all the analyses.
RESULTS
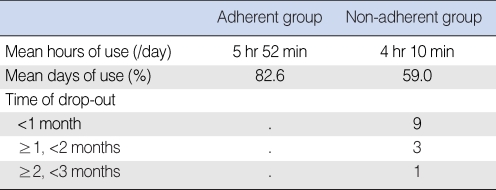
Among the 36 patients, 23 continued the APAP therapy (the adherent group) and 13 discontinued it (the non-adherent group) within three months. The mean hours of use a day was 5 hr and 52 min in the adherent group and 4 hr and 10 min in the non-adherent group (
Table 1). In the non-adherent group, 69.2% of the patients discontinued therapy within one month and 92.3% discontinued therapy within two months (
Table 1).
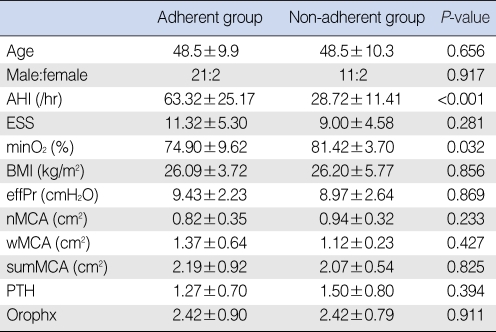
There was no significant difference in the patients' age and the gender distribution. The severity of the OSA was an important factor for determining the adherence to APAP therapy. The mean AHI was 63.32 in the adherent group and it was significantly higher than the mean AHI (28.72) in the non-adherent group (
P<0.001). The MinO
2 was significantly lower in the adherent group (
P=0.032). The ESS was higher in the adherent group than that in the non-adherent group, but this was without statistical significance. There was no significant difference in the effPr, the MCAs, the PTH, the Orophx and the body mass index (BMI) between the two groups (
Table 2).
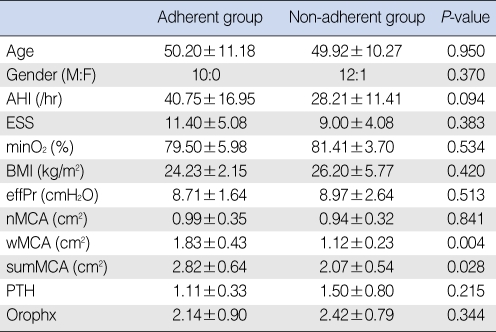
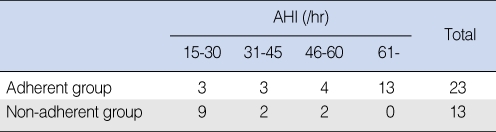
The AHI was a factor associated with compliance with APAP therapy. However, the difference between the AHI distributions between the two groups was very large in this study. There was no patient with an AHI more than 60 in the non-adherent group (
Table 3). Therefore, we limited the subjects to those with an AHI lower than 60/hr (range, 15 to 60/hr). For the 23 patients with an AHI 15 to 60/hr, the mean MCA at the wide side of the nasal cavity was 1.83 cm
2 in the adherent group, which was significantly greater than that (1.12 cm
2) in the non-adherent group (
P=0.004), while the MCAs at the narrow sides of the two groups were not significantly different. The sum of both MCAs was significantly greater in the adherent group (2.82 cm
2) than that in the non-adherent group (2.07 cm
2;
P=0.028). There was no significant difference in the age and gender distribution, the AHI, the ESS, the MCA at the narrow side, the APAP level (effPr), the grade of tonsilar hypertrophy (PTH), the grade of oropharynx inlet (Orophx) and the BMI between the two groups (
Table 4).
DISCUSSION
Compliance with PAP therapy is reported to be 50% at best. However, no specific factor associated with PAP compliance has been identified. Generally, the severity of OSA is considered to be the most important factor for predicting compliance. In a prospective cohort study of 163 patients, Pelletier-Fleury et al. (
7) found that the female gender, a low BMI, a low AHI (<30/hr), a low ESS score and a high CPAP level (>12 cm H
2O) were predictive factors for non-compliance (
7). McArdle et al. (
8), in a prospective study of 1,211 patients, showed that the ESS score and the AHI were the significant independent predictors of long-term use of PAP.
Nasal side effects are believed to account for 30-50% of the patients who are unable to tolerate PAP (
9,
10). Therefore, the influence of upper airway narrowing on PAP therapy has recently been studied. First, it has been reported that in patients with nasal obstruction, the PAP level decreased after surgical procedures for nasal obstruction (such as septoplasty and turbinoplasty) (
11,
12). In addition, it was reported that in patients with a BMI < 25, there was no significant correlation between the nasal cross sectional area and the APAP level, and this was independent from nasal surgery (
3,
13).
A reduced or lower PAP level is thought to reduce the nasal discomfort of PAP therapy and to improve the use of PAP. However, any correlation between the PAP level and PAP compliance has not been clearly identified. Several studies on PAP therapy have not found any correlation between these two parameters (
14-
17).
Consequently, the correlation between narrowing of the nasal airway and PAP compliance is uncertain. Sugiura et al. (
5) reported that the AHI and the nasal resistance evaluated by rhinomannometry were significant factors for predicting the compliance with PAP at one month. Furthermore, Morris et al. (
17) reported that the nasal cross-sectional area was a significant factor for PAP compliance after 18 months and that age, gender, the BMI, the PAP level or the AHI had no influence on compliance. However, Schechter et al. (
18) showed that PAP compliance after one month was not affected by the nasal cross-sectional area, as evaluated by acoustic rhinometry. In this study, age, gender and the BMI also had no influence; the AHI was the only significant factor associated with PAP compliance.
These differences between study results might have been caused by the different characteristics of the study population. For example, in some studies, the AHIs in the study group and the control group were too variable, while in other studies, the AHIs of all the patients were in a narrow range and they were almost the same. Comparison of groups with widely variable AHI distributions that can have an influence on other factors may be subject to a confounding bias. In addition, different definitions of compliance and the length of the follow-up may also contribute to the conflicting results. Furthermore, the small sizes of the various study groups could make the results variable and statistically insignificant.
In the present study, the AHI was the significant parameter that was associated with adherence, which was defined as still using APAP after three months. However, the distributions of the AHIs in the adherent and non-adherent groups were quite different; in the adherent group, the mean AHI was 63.32/hr with a standard deviation of 25.17, while in the non-adherent group, the mean was 28.72/hr with a standard deviation of 11.41. After limiting the AHI level of the two groups, the nasal MCA was found to be a significant factor for initial adherence to APAP therapy.
Furthermore, in the present study, the MCA results from the adherent group of the total subjects were different from that of the limited subjects after excluding the patients with very severe OSAS (AHI >60/hr). We don't know the exact cause of this difference. However, some authors reported that nasal resistance is associated with AHI (
19). Furthermore, the compliance of the patients with very severe OSAS is very high (
4,
20), and the subjective gain from using PAP in this group may conceal the difference of other variables.
Last, in the present study, we used the term 'adherence' that was defined as still using APAP after the research period. There is a lack of a standard definition of compliance or adherence with PAP use in the medical literature. In general, adequate compliance is defined as at least 4 hr of use per night on at least 70% of the nights, and compliance is a word that is often used interchangeably with adherence. We used the term 'adherence' according to the suggestion of Dr. Collard, who defined adherence as pursuing PAP treatment after having been provided with a treatment apparatus (
21).
AHI is a significant factor of APAP adherence and this finding is consistent with that of many previous studies. In addition, the dimension of the nasal cavity hasan influence on initial APAP adherence in the patients with a limited range of the AHI, that is, not too high or not too low.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download