Abstract
Purpose
To evaluate prognostic factors affecting silicone tube intubation outcomes in Asian patients with lacrimal drainage system stenosis.
Methods
A retrospective review was conducted on the medical records of 822 patients (1,118 eyes) who had undergone silicone tube intubation to treat lacrimal drainage system stenosis between January 2011 and December 2012. Patients were divided into two groups: a success group and a failure group. Success was defined as the disappearance of epiphora symptoms, normalization of tear meniscus height, and the easy passage of fluid without resistance on the postoperative syringing test. Patient and ocular parameters were compared between the success and failure groups.
Results
A total of 994 eyes of 727 patients were included in analyses. Patients had a mean follow-up period of 34.11 ± 18.70 weeks. Silicone tube intubation was successful in 67.2% of participants. Significant differences between the success and failure groups were found for age (p < 0.001), history of ipsilateral facial palsy (p = 0.028), follow-up period (p < 0.001), and degree of passage on the preoperative syringing test (p = 0.001). Only age (p < 0.001) and degree of passage on the preoperative syringing test (p = 0.002) remained significantly associated with silicone tube intubation success in multivariate analysis.
Conclusions
Age was negatively associated with silicone tube intubation success in patients with lacrimal drainage system stenosis. The success rate was higher in patients who showed easy passage of fluid without resistance on the preoperative syringing test. These factors should be considered by surgeons planning silicone tube intubation in patients with lacrimal drainage system stenosis.
Silicone tube intubation was first introduced by Keith [1], who used the technique in patients with nasolacrimal duct obstruction as an alternative to dacryocystorhinostomy. Since then, silicone tube intubation has been used for a variety of conditions, including canalicular and nasolacrimal duct stenosis in adults, as well as congenital nasolacrimal duct obstruction [23]. The reported success rate of silicone tube intubation in patients with nasolacrimal duct stenosis ranges from 38.5% to 83% [456789101112]. The wide variation in reported success rates might be related to differences in the definition of surgical success and/or follow-up duration.
Success rates might be higher in patients with a milder degree of nasolacrimal duct stenosis [13] or in those who have not previously undergone probing [612]. The preoperative lacrimal syringing test is an effective tool for estimating the surgical success of silicone tube intubation [14]. However, other factors might also be predictive of surgical success. Knowledge of these factors would allow surgeons to better predict the patients to have successful silicone tube intubation. This would allow patients to have more clear surgical expectations and physicians to make better treatment decisions. Unfortunately, few studies have examined the prognostic factors associated with silicone tube intubation, and the studies that have been performed included fewer than 100 patients.
Herein, we examined a large group of Asian patients with lacrimal drainage system stenosis. We specifically re-examined known prognostic factors and looked for unknown factors that might affect silicone tube intubation outcome.
The institutional review board of Kim's Eye Hospital in Seoul, Korea approved this study. All study methods adhered to the tenets of the Declaration of Helsinki.
A total of 1,118 eyes of 822 patients who underwent silicone tube intubation to treat lacrimal drainage system stenosis at Kim's Eye Hospital between January 2011 and December 2012 were retrospectively examined. The diagnosis of lacrimal drainage system stenosis was based on the presence of epiphora symptoms, a high tear meniscus height (as measured by slit lamp), and lacrimal drainage system stenosis (as identified by dacryocystography). Lacrimal drainage system stenosis was diagnosed by an experienced radiologist, who compared dacryocystography images to those obtained from normal patients.
Participants were excluded from analyses for the following reasons: nasolacrimal duct stenosis secondary to trauma or the presence of a mass, complete nasolacrimal duct obstruction, eyelid malposition, previous endonasal or external dacryocystorhinostomy, early silicone tube removal because of inflammation, silicone tube prolapse that could not be repositioned, failure to attend follow-up examinations, or incomplete demographic information. Patients with a history of ipsilateral facial palsies and lid malposition (e.g., ectropion, lagophthalmos, and exposure keratopathy) were also excluded from the study.
Prior to surgery, all eyes were examined using dacryocystography, underwent the lacrimal syringing test, and had their tear meniscus height measured under a slit lamp. Lacrimal syringing test results were classified into two categories, easy passage of fluid without resistance and partial passage of fluid with regurgitation. Once the decision to have surgery was made, patients were advised to stop taking aspirin, aspirin-containing products, and anticoagulants for at least 1 week before surgery in order to minimize intraoperative bleeding. Intraoperative information was collected, including intraoperative resistance, probe or trephine use, and whether or not punctoplasty was also performed. Following surgery, patients were instructed to use 0.1% fluorometholone and 0.1% levofloxacin eye drops four times a day for 4 weeks. Postoperative follow-up examinations were scheduled 1, 5, 14 and, 26 weeks after surgery. At these visits, surgeons checked for the presence of epiphora or discharge symptoms, examined tear meniscus height under a slit lamp, and performed the lacrimal syringing test. The inserted silicone tube remained in place for at least 3 months before it was removed. After tube removal, patients returned to the clinic for a follow-up visit within 1 month.
Preoperative demographic information including patient age, sex, obstruction side, and pertinent history information such as probing, conjunctival resection, punctoplasty, silicone tube operations, ipsilateral facial palsy, chemotherapy, or canaliculitis was collected. To examine the relationship between age and successful silicone tube intubation, participants were classified into different age groups; first, they were divided into subgroups by decade of age (e.g., 20s, 30s, etc.); then, they were divided into younger and older groups.
Eyes were divided into two groups according to surgical success criteria. Success criteria were defined to meet all of the following: resolution of epiphora symptoms, normalization of tear meniscus height, and easy passage of fluid without resistance on the lacrimal syringing test at the final follow-up examination. For subgroup analyses, eyes were also divided into two groups based on dacryocystography findings, as noted by a radiologist. One subgroup had only nasolacrimal duct stenosis, while the other subgroup had both nasolacrimal duct and canalicular stenosis.
Results are presented as mean ± standard deviation for continuous variables and as percentage for categorical variables. Differences in continuous variables were tested for statistical significance using Student's t-test. Differences in categorical variables were tested for statistical significance using chi-square or Fisher's exact test. A receiver operation characteristic curve was used to determine the age cut-off for successful silicone tube intubation. Multiple logistic regression analysis was used to identify independent predictors of silicone tube intubation success. The magnitude of a factor's impact was estimated using an estimated odds ratio, which is presented with 95% confidence interval. Variables with a p-value ≤0.2 on univariate analyses, as well as a priori variables that were clinically relevant, were entered into a forward stepwise multiple logistic regression model. All tests were two-sided, and statistical significance was defined as p < 0.05. Data were analyzed using IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA).
A total of 994 eyes of 727 patients (503 women and 224 men) were included in this study. Average participant age was 59.68 ± 10.7 years (range, 21 to 87 years). The overall success rate of silicone tube intubation was 67.2% (668 of 994 eyes), and the average postoperative follow-up period was 34.11 ± 18.70 weeks. Although the study group contained more women than men, the distribution of men and women was not statistically different between the success and failure groups (p = 0.285).
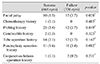
Patient demographics and relevant clinical histories are summarized in Tables 1 and 2. Statistically significant differences between the success and failure groups were found for age, preoperative syringing test results, follow-up period, and history of ipsilateral facial palsy. Patients were significantly older in the failure group (62.21 ± 10.24 years) than in the success group (58.60 ± 10.55 years, p < 0.001). The degree of passage on the preoperative syringing test was also significantly different between the two groups (p = 0.001). We found that 389 eyes (59.7%) in the success group had preoperative easy passage of fluid without resistance, while only 153 eyes (48.3%) in the failure group showed similar preoperative results. The follow-up period averaged 30.64 ± 11.66 weeks in the success group and 41.25 ± 26.72 weeks in the failure group, a difference that was highly significant (p < 0.001). A history of ipsilateral facial palsy was reported in 10 of 668 eyes (1.5%) in the success group and in 12 of 326 eyes (3.7%) in the failure group (p = 0.028). Interestingly, the cause of failure in patients with facial palsy was "anatomical problems" in seven of 12 eyes (58.3%). Anatomical problems were identified using the syringing test result at the final follow-up visit, which was noted as partial passage of fluid with regurgitation.
Participants were also sorted according to stenotic site for subgroup analysis. One group had stenosis in the nasolacrimal duct only (n = 748 eyes), while the other group had both nasolacrimal duct and canalicular stenosis (n = 246 eyes). Potential prognostic factors of silicone tube intubation success were examined separately for each group. In both groups, age (nasolacrimal duct only, p < 0.001; nasolacrimal duct and canalicular, p = 0.003) and preoperative syringing test (nasolacrimal duct only, p = 0.002; nasolacrimal duct and canalicular, p = 0.001) result were significantly different between the success and failure groups. These results are similar to those obtained with data from the whole study population.
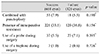
Intraoperative findings are summarized in Table 3. Briefly, the presence of resistance during the operation, the use of a probe or trephine, and combined punctoplasty and silicone tube intubation were not significantly different between the success and failure groups. Intraoperative presence of resistance was observed more often in patients with partial passage of fluid with regurgitation on the preoperative syringing test (169 of 452 eyes, 37.4%) than in those with easy passage of fluid without resistance (172 of 542 eyes, 31.7%) (p = 0.011).
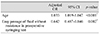
Multivariable logistic regression analysis revealed significant effects of age and preoperative degree of passage on the syringing test (Table 4).
Our study was designed to identify prognostic factors of silicone tube intubation success. In our experience, the success rate of this procedure is low in older patients with nasolacrimal duct stenosis. However, no previous reports have mentioned an effect of age on silicone tube intubation success. We hypothesized that patient age influences surgical outcome of silicone tube intubation and found that success rate was negatively correlated with patient age, but we could not find an age cut-off value.
As people get older, the risk of lacrimal drainage system stenosis increases, as does the possibility of longer-standing disease. Additionally, older patients are more likely to have other problems that affect the lacrimal drainage system (e.g., reduced blinking [151617], increased lid laxity [18], and conjunctivochalasis [1920]). These problems might be easier to observe in older patients, and, unfortunately, their symptoms might not be completely relieved even after correction of nasolacrimal and/or canalicular stenosis. Furthermore, symptom relief might be especially difficult in patients with prolonged, severe stenosis following silicone tube intubation. These points all support our finding that age is negatively correlated with silicone tube intubation success in patients with lacrimal drainage system stenosis.
The success group had a higher proportion of patients with a preoperative syringing test result of easy passage of fluid without resistance than those in the failure group. The syringing test is a basic examination of epiphora symptoms and can be used to diagnose anatomical obstructions of the lacrimal drainage system. Park et al. [14] reported that the syringing test provides the most useful information for estimating the degree of lacrimal drainage system stenosis. Therefore, the preoperative syringing test is a simple and effective tool for predicting silicone tube intubation outcome. In our study subjects, if we considered only the degree of passage observed in the preoperative syringing test (without dacryocystography), 542 of 994 eyes (54.5%) would have been diagnosed with functional obstruction of the lacrimal drainage system. In reality, 172 of the 542 eyes (31.7%) with functional lacrimal drainage system obstructions demonstrated intraoperative resistance. This result is consistent with those obtained by Jeong et al. [21], who reported that 95.3% of patients diagnosed with functional lacrimal drainage system obstruction demonstrated resistance during silicone tube intubation, even if dacryocystography findings were normal. Therefore, if patients demonstrate easy passage of fluid without resistance on the preoperative syringing test and epiphora symptoms, silicone tube intubation should be considered as an effective method to resolve symptoms.
The follow-up period was significantly longer in the failure group than in the success group. This difference can be explained by an increase in hospital visits for patients who continue to exhibit epiphora symptoms after extubation.
The effect of facial palsy on surgical success was significant in univariate analyses but not in multivariate analysis. Because facial palsies tend to occur more frequently in older patients, patient age and facial palsy might not be independent of each other. However, among the 12 eyes of participants with facial palsies examined here, seven (58.3%) failed because of an anatomical rather than a functional problem. This suggests that silicone tube intubation is beneficial for patients with obvious lacrimal drainage system stenosis, even in the presence of facial palsy.
Interestingly, probing history was not significantly correlated with silicone tube intubation success. Lee et al. [6] and Kim and Jeong [12] reported a lower success rate in patients who had undergone previous probing. Unsuccessful repeat probing was performed during their study periods in the 1990s. In more recent years, ophthalmologists have become more hesitant to attempt probing because of the possible impact on future surgeries. This trend was recently revealed by Jeong et al. [21], who reported that probing history did not affect the success rate of silicone tube intubation. Our study result also showed this trend.
We found that the lacrimal drainage system stenosis location did not affect surgical outcome. Park et al. [14] also found that obstruction location did not affect silicone tube intubation outcome. However, Park et al. [14] and Jin et al. [22] reported that the degree of obstruction can affect surgical success. We considered only the location and not the degree of the stenosis. Further studies examining the relationship between degree and location of stenosis as related to surgical success would be useful.
The main limitations of our study were its retrospective design and the failure to consider other factors k nown to decrease lacrimal flow (e.g., conjunctivochalasis, lagophthalmos, lid laxity, and blinking abnormalities). Further studies are needed to evaluate factors associated with lacrimal flow and their relationships with patient age and other prognostic factors.
In conclusion, silicone tube intubation should be considered for relief of epiphora symptoms in patients with nasolacrimal duct stenosis. Silicone tube intubation follows the normal anatomical pathway, rather than creating an artificial route with bypass of the nasolacrimal duct. This allows for a shorter and less invasive surgery. We found that increasing age predicted lower surgical success when silicone tube intubation was performed for nasolacrimal duct stenosis. Easy passage of fluid without resistance during the lacrimal syringing test at the initial examination was a positive predictor of success in patients with lacrimal drainage system stenosis. When surgeons plan to perform silicone tube intubation, these factors should be considered.
Figures and Tables
References
1. Keith CG. Intubation of the lacrimal passages. Am J Ophthalmol. 1968; 65:70–74.
2. Beigi B, O'Keefe M. Results of Crawford tube intubation in children. Acta Ophthalmol (Copenh). 1993; 71:405–407.
3. Fulcher T, O'Connor M, Moriarty P. Nasolacrimal intubation in adults. Br J Ophthalmol. 1998; 82:1039–1041.
4. Connell PP, Fulcher TP, Chacko E, et al. Long term follow up of nasolacrimal intubation in adults. Br J Ophthalmol. 2006; 90:435–436.
5. Shah A, Tekriwal AK, Drummond PM, Woodruff G. Long-term results of closed nasolacrimal intubation in adults. Eur J Ophthalmol. 2007; 17:490–493.
6. Lee SH, Kim SD, Kim JD. Silicone intubation for nasolacrimal duct obstruction in adult. J Korean Ophthalmol Soc. 1997; 38:185–189.
7. Lee HS, Hwang WS, Byun YJ. Clinical results of silicone intubation for nasolacrimal duct obstruction in adult. J Korean Ophthalmol Soc. 1997; 38:1926–1930.
8. Kwon YH, Lee YJ. Long-term results of silicone tube intubation in incomplete nasolacrimal duct obstruction (NLDO). J Korean Ophthalmol Soc. 2008; 49:190–194.
9. Angrist RC, Dortzbach RK. Silicone intubation for partial and total nasolacrimal duct obstruction in adults. Ophthal Plast Reconstr Surg. 1985; 1:51–54.
10. Conway ST. Evaluation and management of "functional" nasolacrimal blockage: results of a survey of the American Society of Ophthalmic Plastic and Reconstructive surgery. Ophthal Plast Reconstr Surg. 1994; 10:185–187.
11. Sohn HY, Hur J, Chung EH, Won IG. Clinical observation on silicone intubation in obstruction of lacrimal drainage system. J Korean Ophthalmol Soc. 1990; 31:135–140.
12. Kim HD, Jeong SK. Silicone tube intubation in acquired nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2000; 41:327–331.
13. Oum JS, Park JW, Choi YK, et al. Result of partial nasolacrimal duct obstruction after silicone tube intubation. J Korean Ophthalmol Soc. 2004; 45:1777–1782.
14. Park JS, Ha SW, Lew HL. Factors affecting the long-term outcome of silicone tube intubation in patients with nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2011; 52:129–135.
15. Sun WS, Baker RS, Chuke JC, et al. Age-related changes in human blinks: passive and active changes in eyelid kinematics. Invest Ophthalmol Vis Sci. 1997; 38:92–99.
16. Pottier F, El-Shazly NZ, El-Shazly AE. Aging of orbicularis oculi: anatomophysiologic consideration in upper blepharoplasty. Arch Facial Plast Surg. 2008; 10:346–349.
17. Lee H, Park M, Lee J, et al. Histopathologic findings of the orbicularis oculi in upper eyelid aging: total or minimal excision of orbicularis oculi in upper blepharoplasty. Arch Facial Plast Surg. 2012; 14:253–257.
18. Detorakis ET, Zissimopoulos A, Katernellis G, et al. Lower eyelid laxity in functional acquired epiphora: evaluation with quantitative scintigraphy. Ophthal Plast Reconstr Surg. 2006; 22:25–29.
19. Gumus K, Crockett CH, Pflugfelder SC. Anterior segment optical coherence tomography: a diagnostic instrument for conjunctivochalasis. Am J Ophthalmol. 2010; 150:798–806.
20. Huang Y, Sheha H, Tseng SC. Conjunctivochalasis interferes with tear flow from fornix to tear meniscus. Ophthalmology. 2013; 120:1681–1687.
21. Jeong HW, Cho NC, Ahn M. Result of silicone tube intubation in patients with epiphora who showing normal finding in dacryocystography. J Korean Ophthalmol Soc. 2008; 49:706–712.
22. Jin SW, Ahn HB, Kim MH. Long-term results of silicone tube intubation in patients with common canalicular stenosis. J Korean Ophthalmol Soc. 2012; 53:1373–1377.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download