Abstract
Purpose
To determine the effects of intravitreal anti-vascular endothelial growth factor (VEGF) on thickness of the retinal nerve fiber layer (RNFL) in patients with age-related macular degeneration.
Methods
Twenty eyes of 20 patients diagnosed with age-related macular degeneration who underwent intravitreal anti-VEGF injection were studied. Postinjection RNFL thickness was measured using optical coherence tomography. Average thickness, four-quadrant RNFL thicknesses, and intraocular pressure (IOP) in affected eyes were measured before and 6 and 12 months after anti-VEGF injection for comparison. RNFL thickness and IOP in affected and normal fellow eyes were also compared. Given that macular lesions can affect RNFL thickness, the changes in thickness were evaluated by dividing the 12 clock-hour RNFL into the pathologic areas adjacent to the lesion and the non-pathologic area.
Results
The mean clock-hour segment in the pathologic area was 4.8 hours. A significantly thicker RNFL was exhibited in temporal quadrants and pathologic areas (p = 0.043 and 0.048, respectively) in affected eyes before injection compared to the baseline RNFL thickness in normal eyes. No significant differences were found in RNFL thickness or IOP between affected and normal eyes after injection. The changes over time in the temporal and pathologic areas were statistically significant at 6 and 12 months after injection compared to baseline data (p < 0.05). No significant differences were displayed in RNFL thickness in the other three quadrants or in non-pathologic areas in either affected or normal eyes. Sequential changes in RNFL thickness in affected eyes were not significant.
Conclusions
Repeat intravitreal anti-VEGF treatment did not have a significant effect on RNFL thickness. RNFL thickness significantly decreased with time in the pathologic areas and in the temporal segment adjacent to exudative macular lesions. The reduction in RNFL thickness was most likely associated with changes in the macular lesion rather than with anti-VEGF injection.
Vascular endothelial growth factor (VEGF) is involved in angiogenesis and vascular permeability and plays a crucial role in inducing exudative age-related macular degeneration (AMD) by promoting choroidal neovascularization. Anti-VEGF therapy is widely used in various eye disorders, including AMD, because it is effective for suppressing angiogenesis and macular edema [123].
The efficacies of the anti-VEGF agents ranibizumab (Lucentis; Genentech, San Francisco, CA, USA) and bevacizumab (Avastin, Genentech) have been illustrated in many studies, although some complications have been reported [4567]. Elevated intraocular pressure is a common complication following intravitreal injection of anti-VEGF. In some studies, intraocular pressure increased steeply following injection but declined to normal levels within 10 to 30 minutes [891011]. In other studies, intraocular pressure remained elevated for some time following injection [121314]. Some studies have also suggested that blocking VEGF with antagonists leads to nerve damage, given the role of VEGF in neurophysiological processes [151617].
Because the effects of intravitreally injected VEGF medications are of limited duration, repeated injections are required for long-term VEGF-inhibiting effects. Repeat intravitreal injection might result in sustained intraocular pressure, and blocking VEGF might cause optic nerve damage. Therefore, the effects of repeat intravitreal anti-VEGF injection on the optic nerve were evaluated in patients with AMD, based on spectral domain optical coherence tomography (OCT) retinal nerve fiber layer (RNFL) thickness measurements.
This was a prospective cohort study. The protocol was approved by the institutional review board of Chungnam National University Hospital. All participants signed informed consent forms, and the study adhered to the tenets of the Declaration of Helsinki.
The study initially included 24 eyes of 24 patients who presented to the retina clinic at the hospital, were diagnosed with unilateral exudative AMD, and underwent anti-VEGF treatment with intravitreal ranibizumab. Normal fellow eyes served as the control group. All subjects received three intravitreal injections of ranibizumab at monthly intervals from the diagnosis date. Additional injections were administered if necessary, depending on the presence of macular edema or hemorrhage.
Subjects were excluded if they had an eye disorder that could affect RNFL thickness, such as glaucoma or retinal vessel obstruction, a history of photodynamic treatment for macular degeneration, bilateral exudative AMD, or a history of intraocular surgery such as vitrectomy. In addition, four of the initial patients were excluded because of poor data quality, resulting in a total of 20 eyes of 20 patients included for final analysis.
All subjects underwent intraocular pressure measurement, slit-lamp examination, and fundus examination. The average and four-quadrant RNFL thicknesses were measured in the affected and normal counterpart eyes using a Cirrus spectral domain OCT (Carl Zeiss Meditec, Dublin, CA, USA).
RNFL thickness was measured before and 6 and 12 months after intravitreal injection with the optic disc cube mode of Cirrus spectral domain OCT. OCT was performed by an experienced examiner. Poor-quality images with a signal strength less than 5 and any scans with visible eye movements, blinking artifacts, or poor centration were excluded. Also, images with missing parts, misplacement of boundaries between retinal layers, or images showing seemingly distorted anatomy that resulted in readings of zero or otherwise abnormally low values were discarded to prevent algorithm segmentation failure. All eyes were scanned twice to evaluate reproducibility, and good reproducibility was achieved based on intraclass correlation coefficients of 0.941 to 0.989. The Optic Disc Cube 200 × 200 scanning program (Cirrus HD-OCT, Carl Zeiss Meditec) obtains 200 A-scans from 200 linear B-scans evenly distributed in a 6 mm × 6 mm area centered over the optic nerve. This scanning mode was used to measure the average and four-quadrant RNFL thicknesses.
RNFL thicknesses were measured in affected eyes before and 6 and 12 months after intravitreal injection for sequential comparison. RNFL thickness in affected and normal eyes was also compared. RNFL thickness was divided into 12 segments of 30 degrees for 12 clock-hour RNFL thickness measurements.
Under the assumption that macular lesions affect RNFL thickness, changes in average thickness were evaluated after dividing the 12 clock-hour RNFL thickness measurements into pathologic area, including the lesion, and non-pathologic area of the affected eye and the corresponding area of the normal fellow eye (Fig. 1A and 1B).
Intraocular pressure measurements were obtained using a Goldmann applanation tonometer before and 6 and 12 months after intravitreal injection for sequential comparison. Intraocular pressure in affected and normal eyes was also compared.
Statistical analysis was performed using PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA). Sequential time-related changes in RNFL thickness in affected and normal eyes were analyzed using Wilcox signed-ranks tests. The comparison of RNFL thickness between affected and normal eyes at different time points was conducted using a Mann-Whitney U-test. A p-value less than 0.05 was considered statistically significant.
Twenty eyes of 20 patients were enrolled, of whom 13 were male and seven were female with a median age of 67.1 ± 8.9 years. The average best-corrected visual acuity was 0.5 ± 0.6 (logarithm of the minimum angle of resolution), and the mean intraocular pressure was 15.3 ± 2.6 mmHg. The mean number of anti-VEGF injections was 5.0 ± 1.0, and the mean clock-hour segment in the pathologic area was 4.8 ± 0.5 in the 12 clock-hour RNFL thickness analysis (Table 1).
The overall average RNFL thickness at baseline was 98.0 ± 6.8 µm in affected eyes and 94.5 ± 7.3 µm in normal eyes (p = 0.146). Postinjection differences in RNFL thickness between the two groups were not significant at 6 or 12 months (p = 0.892 and 0.776, respectively). The average RNFL thickness in affected eyes was 96.3 ± 4.2 µm at 6 months and 95.5 ± 4.3 µm at 12 months after intravitreal injection, showing no significant difference from baseline (p = 0.153 and 0.070, respectively).
Segmental RNFL thickness in the superior, inferior, and nasal quadrants did not exhibit significant changes in the affected or normal eyes at 6 and 12 months postinjection compared to baseline RNFL thickness (p > 0.05). Postinjection changes in RNFL thickness were not significant in affected eyes over time (p > 0.05).
Temporal RNFL thickness at baseline was 84.4 ± 20.9 µm in affected eyes, which was significantly thicker than the 73.0 ± 9.7 µm observed in normal eyes (p = 0.043). However, postinjection differences in temporal RNFL thickness between the two groups were not significant at 6 or 12 months (p = 0.464 and 0.787, respectively). Time-related changes in temporal RNFL thickness were significant in affected eyes 6 and 12 months after injection compared to baseline (p = 0.012 and 0.006, respectively) (Table 2 and Fig. 2).
The overall average RNFL thickness at baseline was 85.8 ± 21.2 µm in the pathologic area of affected eyes, which was significantly greater than the 74.0 ± 10.0 µm measured in normal eyes (p = 0.048). However, postinjection differences in RFNL thickness were not significant between affected and normal eyes at 6 or 12 months (p = 0.607 and 0.665, respectively). Longitudinal changes in RNFL thickness in the pathologic areas were significant in affected eyes at 6 and 12 months postinjection compared to baseline (p = 0.011 and 0.005, respectively).
The average intraocular pressure at baseline was 15.3 ± 2.6 mmHg in affected eyes and 16.0 ± 2.9 mmHg in normal eyes, showing no significant difference (p = 0.473). Postinjection differences in intraocular pressure between the two groups were not significant at 6 or 12 months (p = 1.000 and 0.534, respectively) (Table 4).
Intravitreal anti-VEGF injection is commonly used in the treatment of a wide variety of retinal diseases, including exudative AMD. However, intravitreal injection can result in complications, including endophthalmitis, intraocular hemorrhage, and ocular hypertension. Several studies have addressed these complications [4567].
Temporary ocular hypertension following intravitreal anti-VEGF injection is caused by increased intraocular volume [8911]. Falkenstein et al. [9] reported that the average intraocular pressure soared to 36.3 mmHg from a baseline of 15.2 mmHg 3 minutes after intravitreal injection of 0.05 mL bevacizumab in 70 patients. However, the mean intraocular pressure decreased to 24.6 mmHg at 10 minutes, and intraocular pressure in all eyes decreased to less than 30 mmHg after 15 minutes. Sharei et al. [11] also reported that intraocular pressure increased to more than 40 mmHg immediately after intravitreal injection of 0.05 mL ranibizumab in 71.1% of 45 patients but decreased to 21 mmHg at 10 minutes.
On the other hand, some studies have observed a longer duration of ocular hypertension. Kahook et al. [12] reported six cases of chronic ocular hypertension after one-time or repeat injection of bevacizumab and cited aqueous outflow induced by an accumulated trabecular meshwork and inflammatory responses as the cause of sustained ocular hypertension [15].
In our study, intraocular pressure measurements of affected and normal eyes were obtained 6 and 12 months after intravitreal injection for comparison. The difference in mean intraocular pressure was not significantly different between the affected and normal eyes.
In addition, anti-VEGF drugs can have adverse effects on neuronal cells due to the blockage of VEGF [16171819]. Considering that VEGF is involved in the survival of neuronal cells and has neuroprotective and neurotrophic actions in addition to its angiogenesis role [1617], anti-VEGF treatment can affect the neurophysiologic role of VEGF and cause damage to optic nerves.
Because the effects of anti-VEGF agents are of limited duration, repeated intravitreal injections are required in many cases. As a result, brief ocular hypertension, increased intraocular pressure fluctuations, changes in ocular blood flow, and adverse effects on the optic nerve can ensue.
Seth et al. [20] analyzed changes in the cup-to-disc ratio in 23 eyes over 9 months following repeat intravitreal injection of pegaptanib. They observed no statistically significant changes in the ratio between treated and normal eyes. Horsley et al. [19] retrospectively assessed changes in RNFL thickness in patients with AMD following repeat intravitreal anti-VEGF injection using stratus OCT and reported no significant postinjection changes in RNFL thickness throughout the follow-up period. Another study assessed RNFL thickness in 49 eyes of 49 patients with AMD using stratus OCT for 12 months after an average of 4.8 intravitreal injections of an anti-VEGF agent [21]. They found that average RNFL was significantly thinner at 12 months compared to baseline values. They also found that RNFL thickness significantly decreased in the superior, inferior, and temporal quadrants at 12 months compared to baseline data. However, there was no significant change in nasal RNFL thickness.
In the present study, RNFL thickness at baseline was significantly greater in the temporal and pathologic areas of affected eyes compared to normal eyes. However, no significant difference was displayed between the two groups after injection. RNFL thickness in the temporal and pathologic areas of affected eyes did, however, display significant changes at sequential time points after injection. Longitudinal changes in RNFL thickness were not significant in quadrants other than the temporal quadrant in non-pathologic areas of affected eyes. Therefore, the reduction in RNFL thickness in the pathologic area is more likely to be due to a change in the macular lesion rather than a result of increased pressure due to anti-VEGF administration. That is, RNFL thickness was increased at baseline due to an exudative lesion, edema, or hemorrhage in the macular area [22], and RNFL thickness was reduced 6 and 12 months after injection because the exudative lesion improved after repeat injection. This conclusion is supported by the findings of greater RNFL thickness in the temporal quadrant in affected eyes at baseline compared to that of normal eyes, without a significant difference in postinjection RNFL thickness between the two groups. The mean clock-hour RNFL segment in the pathologic area was 4.8 hours. This area overlapped that of the temporal quadrant, leading to similar changes in RNFL thickness.
Hwang et al. [22] described two reasons for increased RNFL thickness in diabetic macular edema (DME) patients. First, an increase in temporal sector RNFL thickness in patients with acutely worsening DME might be related to a change in macular tomography due to macular edema. Second, the breakdown of the inner blood retinal barrier in RNFL causes RNFL edema, which then results in increased RNFL thickness in all sectors in patients with chronic DME. The present study targeted AMD patients rather than DME patients. Thus, a similar increase in temporal sector RNFL thickness at baseline in patients with AMD might be related to changes in macular tomography due to macular edema.
This prospective study represents an improvement over previous studies. Spectral domain-OCT was used, which offers better reproducibility than time-domain OCT. Four-quadrant RNFL thickness measures were conducted in addition to an overall assessment of average RNFL thickness. Additionally, pathologic and non-pathologic areas close to and distant from the macular lesions were separately evaluated.
In conclusion, repeat intravitreal anti-VEGF treatment did not have a significant effect on overall RNFL thickness. However, RNFL thickness significantly decreased with time in the temporal and pathologic areas. It can be concluded that the reduction in RNFL thickness was more associated with changes in the macular lesion rather than with anti-VEGF injection. Long-term prospective studies with more subjects are needed to investigate the long-term effects of anti-VEGF treatment in various disease states.
Figures and Tables
Fig. 1
Fundus photograph and retinal nerve fiber layer thickness analysis of (A) the right affected eye and (B) the left normal fellow eye of a patient with age-related macular degeneration. The red and black arrows represent the pathologic and non-pathologic areas in the affected eye, respectively. The green and blue arrows represent the same area in the unaffected eye, respectively.

Fig. 2
Longitudinal changes in average and quadrant retinal nerve fiber layer (RNFL) thickness in affected eyes. The differences between baseline and postinjection at 6 months (p = 0.012) and 12 months (p = 0.006) were statistically significant in the temporal areas. *p < 0.05, Wilcoxon signed-rank test.

Fig. 3
Longitudinal changes in average retinal nerve fiber layer (RNFL) thickness in the pathologic and non-pathologic areas of affected eyes. The differences between baseline and post-injection at 6 months (p = 0.011) and 12 months (p = 0.005) were statistically significant in the pathologic areas. *p < 0.05, Wilcoxon signed-rank test.

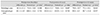
Table 2
Changes in average and quadrant retinal nerve fiber layer thickness in affected and normal counterpart eyes

References
1. Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006; 355:1419–1431.
2. Gunther JB, Altaweel MM. Bevacizumab (Avastin) for the treatment of ocular disease. Surv Ophthalmol. 2009; 54:372–400.
3. el Matri L, Chebil A, Kort F, et al. Intravitreal injection of triamcinolone combined with bevacizumab for choroidal neovascularization associated with large retinal pigment epithelial detachment in age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2010; 248:779–784.
4. Jager RD, Aiello LP, Patel SC, Cunningham ET Jr. Risks of intravitreous injection: a comprehensive review. Retina. 2004; 24:676–698.
5. Angulo Bocco MC, Glacet-Bernard A, Zourdani A, et al. Intravitreous injection: retrospective study on 2028 injections and their side effects. J Fr Ophtalmol. 2008; 31:693–698.
6. Sampat KM, Garg SJ. Complications of intravitreal injections. Curr Opin Ophthalmol. 2010; 21:178–183.
7. Day S, Acquah K, Mruthyunjaya P, et al. Ocular complications after anti-vascular endothelial growth factor therapy in Medicare patients with age-related macular degeneration. Am J Ophthalmol. 2011; 152:266–272.
8. Hollands H, Wong J, Bruen R, et al. Short-term intraocular pressure changes after intravitreal injection of bevacizumab. Can J Ophthalmol. 2007; 42:807–811.
9. Falkenstein IA, Cheng L, Freeman WR. Changes of intraocular pressure after intravitreal injection of bevacizumab (Avastin). Retina. 2007; 27:1044–1047.
10. Kim JE, Mantravadi AV, Hur EY, Covert DJ. Short-term intraocular pressure changes immediately after intravitreal injections of anti-vascular endothelial growth factor agents. Am J Ophthalmol. 2008; 146:930–934.e1.
11. Sharei V, Hohn F, Kohler T, et al. Course of intraocular pressure after intravitreal injection of 0.05 mL ranibizumab (Lucentis). Eur J Ophthalmol. 2010; 20:174–179.
12. Kahook MY, Kimura AE, Wong LJ, at al. Sustained elevation in intraocular pressure associated with intravitreal bevacizumab injections. Ophthalmic Surg Lasers Imaging. 2009; 40:293–295.
13. Bakri SJ, McCannel CA, Edwards AO, Moshfeghi DM. Persisent ocular hypertension following intravitreal ranibizumab. Graefes Arch Clin Exp Ophthalmol. 2008; 246:955–958.
14. Adelman RA, Zheng Q, Mayer HR. Persistent ocular hypertension following intravitreal bevacizumab and ranibizumab injections. J Ocul Pharmacol Ther. 2010; 26:105–110.
15. Jalil A, Fenerty C, Charles S. Intravitreal bevacizumab (Avastin) causing acute glaucoma: an unreported complication. Eye (Lond). 2007; 21:1541.
16. Sondell M, Lundborg G, Kanje M. Vascular endothelial growth factor has neurotrophic activity and stimulates axonal outgrowth, enhancing cell survival and Schwann cell proliferation in the peripheral nervous system. J Neurosci. 1999; 19:5731–5740.
17. Zachary I. Neuroprotective role of vascular endothelial growth factor: signalling mechanisms, biological function, and therapeutic potential. Neurosignals. 2005; 14:207–221.
18. Nishijima K, Ng YS, Zhong L, et al. Vascular endothelial growth factor-A is a survival factor for retinal neurons and a critical neuroprotectant during the adaptive response to ischemic injury. Am J Pathol. 2007; 171:53–67.
19. Horsley MB, Mandava N, Maycotte MA, Kahook MY. Retinal nerve fiber layer thickness in patients receiving chronic anti-vascular endothelial growth factor therapy. Am J Ophthalmol. 2010; 150:558–561.e1.
20. Seth RK, Salim S, Shields MB, Adelman RA. Assessment of optic nerve cup-to-disk ratio changes in patients receiving multiple intravitreal injections of antivascular endothelial growth factor agents. Retina. 2009; 29:956–959.
21. Martinez-de-la-Casa JM, Ruiz-Calvo A, Saenz-Frances F, et al. Retinal nerve fiber layer thickness changes in patients with age-related macular degeneration treated with intravitreal ranibizumab. Invest Ophthalmol Vis Sci. 2012; 53:6214–6218.
22. Hwang DJ, Lee EJ, Lee SY, et al. Effect of diabetic macular edema on peripapillary retinal nerve fiber layer thickness profiles. Invest Ophthalmol Vis Sci. 2014; 55:4213–4219.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download