Abstract
The authors wish to report a case of bilateral acute anterior uveitis and optic disc edema following a hemotoxic snake bite, in order to highlight the concomitant occurrence of these conditions and the potential adverse effects of anti-snake venom (ASV). A 35-year-old male was bitten by a viper at seventeen thirty hours, and was started on ASV. Two days following treatment he experienced sudden onset redness and painful diminution of vision in both eyes (OU). On examination, the patient's visual acuity (VA) in OU was 20/200. Examination revealed fresh keratic precipitates, cells, and flare in the anterior chamber (AC), posterior synechiae, sluggish and ill-sustained pupillary reaction, and hyperemic, edematous disc with blurred margins in OU. He was started on topical steroids, cycloplegics and intravenous methylprednisolone. Following treatment, the patient showed improvement and was continued on topical medications and oral prednisolone tapered over 3 weeks, after which VA OU improved, the AC showed no cells and flare and disc edema resolved. Uveitis and optic disc edema in snake bite can either be due to the direct toxic effects of the venom or the effect of ASV. Steroids have a beneficial role in the management of these symptoms.
Poisonous snakes are found throughout the world, and nearly 60,000 people are bitten by snakes every year on the Indian subcontinent, with a mortality rate of 25% [1]. However, ophthalmic complications of snake bite are rare. Acute anterior uveitis following snake bite has been reported uncommonly, and there are only a few reported cases of optic neuritis and ophthalmoplegia following a snake bite [2,3,4,5,6]. We report a case of concomitant bilateral acute anterior uveitis and optic disc edema following a hemotoxic snake bite.
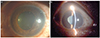
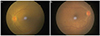
A 35-year-old male farmer was brought to the emergency department after being bitten by a viper on the dorsum of the right foot. He had received first aid following the bite in the form of local wound incision and application of tourniquet. The patient was stable and vitals were normal. There were no signs of internal or external bleeding. Examination revealed a wound on the dorsum of the right foot with cellulitis of the lower limb. The patient was started on anti-snake venom (ASV) injection 70 mL stat, followed by 30 ml every six hours for two days. On the second day the patient complained of sudden onset pain and blurring of vision in both eyes (OU) which gradually worsened over the next four days. He was referred to the eye department on sixth day following the bite. On examination, the best-corrected visual acuity (BCVA) in OU was 20/200. Extraocular movements were full and free in all directions of gaze. Anterior segment examination of OU revealed fresh keratic precipitates with grade 3 anterior chamber (AC) cells and flare with posterior synechiae (Fig. 1). Pupils showed a sluggish and ill-sustained reaction to bright light. Fundus examination through hazy media revealed disc hyperemia with blurred margins and disc edema (Fig. 2). The rest of the fundus was within normal limits. On color vision testing by pseudoisochromatic plates of Ishihara, the patient responses from the second plate to the ninth plate were incorrect, and he was not able to identify the number in tenth to thirteenth plates in OU, which indicated total red green deficiency. Visual fields could not be tested, as the patient was irritable and uncooperative. Visual evoked potential testing showed prolonged latency and decreased amplitude. Optical coherence tomography (OCT) revealed a retinal nerve fiber layer (RNFL) thickness of 247 microns in the right eye (OD) and 245 microns in the left eye (OS) superiorly, 117 microns (OD) and 113 microns (OS) nasally, 260 microns (OD) and 258 microns (OS) inferiorly, and 169 microns (OD) and 162 microns (OS) temporally, suggesting an increase in RNFL thickness. Neuroimaging of the brain was normal. Magnetic resonance imaging of the orbit showed abnormal signal intensity from the optic nerve of OU. A diagnosis of acute anterior uveitis and optic disc edema OU following snake bite was established and the patient was started on topical steroid drops six times a day and homatropine drops two times a day, and was given intravenous methylprednisolone 250 mg daily in normal saline over one hour for 3 days. On the fourth day, the visual acuity in OU improved to 20/80. Examination showed a decrease in the AC cells, flare and disc edema. OCT revealed that the disc edema had resolved. The patient was continued on topical steroids and cycloplegics, and was started on oral prednisolone in doses tapered over three weeks. At the end of three weeks, visual acuity improved to 20/30 with AC exhibiting no cells or flare, and disc edema resolved completely.
Ocular complications following snake bite are usually rare. Snake bite accounts for 4% of all ophthalmoplegias. Optic neuritis and optic atrophy following snake bite have been reported in very few cases [3,4,5,6]. Acute anterior uveitis following snake bite has been reported uncommonly and a thorough review of the English literature found no reports of acute anterior uveitis with concomitant optic disc edema following snake bite. Interestingly, in the majority of reported cases of optic neuritis following a snake bite, diminution of vision occurred on the sixth day and all of these patients received ASV.
The cause of uveitis in this patient is unclear and may have been due to the direct toxic effect of the snake venom. Various causes of optic neuritis following snake bite have been postulated, including capillary damage and extensive hemorrhage [3], allergy to ASV [4], and the direct toxic effect of snake venom [5]. There is no conclusive evidence for any of these theories, just indirect evidence.
The blurred vision that occurred in our patient on the second day can be explained by the development of acute anterior uveitis due to the toxicity of snake venom, whereas the severe diminution of vision that occurred over the next four days can be attributed to the worsening of acute anterior uveitis due to a concomitant allergy to ASV, leading to the development of optic disc edema. Pulse steroid therapy with methylprednisolone proved to be effective in our patient, as it was in a similar case reported by Menon et al. [7].
This case reports the rare concomitant occurrence of acute anterior uveitis and optic disc edema following a snake bite, and describes the role of steroids in the management of these cases. It also highlights the fact that, even though ASV remains the mainstay of treatment for snake bite, it is not free of adverse effects, and the treating physician needs to be aware of these rare complications of snake bite and ASV therapy.
Figures and Tables
References
1. Nigam P, Tandon VK, Kumar R, et al. Snake bite: a clinical study. Indian J Med Sci. 1973; 27:697–704.
2. Chopra PC. Optic neuritis after cobra bite. Indian Med Gaz. 1939; 74:420.
3. Davenport RC, Budden FH. Loss of sight following snake bite. Br J Ophthalmol. 1953; 37:119–121.
4. Mathur SP. Allergy to antivenine serum. Br J Ophthalmol. 1959; 43:50–51.
5. Rao KV. Optic neuritis and ophthalmoplegia caused by snake bite. Indian J Ophthalmol. 1981; 29:243–245.
6. Sanghavi NG, Amin SK, Naik RS. Bilateral optic neuritis following snake bite: a case report. J Assoc Physicians India. 1982; 30:117–118.
7. Menon V, Tandon R, Sharma T, Gupta A. Optic neuritis following snake bite. Indian J Ophthalmol. 1997; 45:236–237.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download