Abstract
A 70-year-old man with a long history of diabetes mellitus presented to our hospital (Department of Ophthalmology, Sahm Yook Medical Center, Seoul, Korea) complaining of severe ocular pain and visual disturbance in his left eye that had started three days prior to admission. A round 3.7 × 5.0 mm dense central stromal infiltrate with an overlying epithelial defect was noted on slit-lamp examination. Following corneal scrapings and culture, topical 0.5% moxifloxacin and 0.5% tobramycin were administered hourly. A few days later, Stenotrophomonas maltophilia was isolated in a bacterial culture from a corneal specimen. According to the results of susceptibility tests, topical 0.5% moxifloxacin was given every hour and 0.5% tobramycin was stopped. The patient's clinical features improved steadily with treatment. The corneal epithelium healed rapidly, and the infiltrate resolved within four weeks of the initiation of treatment. The patient's best corrected visual acuity improved from hand motion to 20 / 25.
Stenotrophomonas maltophilia (S. maltophilia) is a non-fermentative, gram-negative bacillus that has assumed an increasingly important role as a nosocomial pathogen in immune compromised patients [1]. Treatment of S. maltophilia infections is also complicated by the fact that isolates are resistant to many broad-spectrum agents [2]. Ophthalmologic syndromes, including conjunctivitis, keratitis, dacrocystitis and pre-septal cellulitis, may be caused by S. maltophilia [3]. S. maltophilia keratitis is associated with very poor prognoses because of its resistance to many broad-spectrum antibiotics [4]. We describe a case of S. maltophilia keratitis that was effectively treated with topical moxifloxacin (fourth-generation fluoroquinolone) monotherapy.
A 70-year-old male presented to our hospital (Department of Ophthalmology, Sahm Yook Medical Center, Seoul, Korea) with a three-day history of left eye pain and decreased vision. He had a long history of diabetes mellitus that was controlled with oral anti-hyperglycemic agents. The patient suffered from bilateral proliferative diabetic retinopathy and had undergone pan retinal photocoagulation several times since March 1995. At age 60 he had undergone phacoemulsifications with intraocular lens implantation for the treatment of senile cataracts in both eyes.
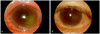
On presentation, the patient's visual acuity was hand motion in the left eye. Slit lamp examination revealed a heavily edematous cornea and a round 3.7 × 5.0 mm dense central stromal infiltrate with an overlying epithelial defect (Fig. 1). Anterior chamber cells 3+ and ciliary injection were also observed.
After scrapings were collected from the lesion for smears and cultures, the patient was treated hourly with 0.5% moxifloxacin and 0.5% tobramycin. Four days after the initiation of treatment, heavy growth of S. maltophilia was observed in culture. The isolated bacteria were sensitive to ciprofloxacin, sulfamethoxazole-trimethoprim, levofloxacin, and moxifloxacin, but were resistant to all aminoglycosides and B-lactams (Table 1). According to the results of susceptibility tests, topical 0.5% moxifloxacin was given every hour and 0.5% tobramycin was stopped.
The patient's corneal epithelium healed in two weeks after the initiation of treatment. After the epithelium had healed, moxifloxacin was administered four times per day. The corneal infiltrate resolved within four weeks. However, mild opacity remained in the posterior stroma (Fig. 1). The patient's best corrected visual acuity improved from hand motion to 20 / 25. His infectious keratitis was controlled and had not recurred at the one-year follow-up examination.
S. maltophilia is a motile, non-fermentative, oxidase-negative, aerobic, Gram-negative bacillus that is widespread in the environment [5]. It is an opportunistic pathogen believed to have limited pathogenicity unless it is associated with nosocomial infections of immune compromised patients [6]. S. maltophilia is a seldom-reported pathogen in lens care systems or ocular infections [7]. However, reports of postoperative and post-traumatic S. maltophilia ocular infections are increasing [8]. The reasons underlying this emergence are complex, but may be related to the improved laboratory isolation techniques and enhanced reporting. Treatment of S. maltophilia infections is complicated by the fact that isolates are often resistant to many broad-spectrum antibiotic agents [2].
You et al. [4] reported the treatment results and prognoses of 10 cases of S. maltophilia keratitis in 2007 after one time applications of levofloxacin ophthalmic solution as a first line treatment of choice before culture results. They then added fortified tobramycin and cefazolin if corneal ulcers were large and centrally located of the cornea. Patients also underwent surgical treatment when there was no response to medication. The final visual acuity in three cases that had no co-infections was worse than hand motion.
Fourth-generation fluoroquinolones (moxifloxacin and gatifloxacin) show an enhanced spectrum of activity against Gram-positive bacteria and comparable activity to second- and third-generation fluoroquinolones (ciprofloxacin and levofloxacin) against Gram-negative bacteria [9]. New ocular antibiotic formulations with improved potency, such as moxifloxacin ophthalmic solution 0.5% (Vigamox®; Alcon Laboratories, Fort Worth, TX, USA) or gatifloxacin ophthalmic solution 0.3% (Zymar®; Allergan, Irvine, CA, USA) are currently available and have been shown to inhibit growth of organisms resistant to second- and third-generation fluoroquinolones [10]. Several in vitro susceptibility studies, demonstrate that moxifloxacin is more active than earlier generation fluoroquinolones (ciprofloxacin, ofloxacin, and levofloxacin), especially against S. maltophilia [9]. For these reasons, we chose moxifloxacin monotherapy for treatment of S. maltophilia keratitis, even though antibiotic sensitivity was equal for both levofloxacin and moxifloxacin.
In conclusion, we report the case of a patient who was diagnosed with S. maltophilia keratitis and effectively treated with moxifloxacin monotherapy. Unlike most previously-reported cases, which had poor prognoses, in our patient moxifloxacin monotherapy led to a good visual outcome.
Figures and Tables
References
1. Khardori N, Elting L, Wong E, et al. Nosocomial infections due to Xanthomonas maltophilia (Pseudomonas maltophilia) in patients with cancer. Rev Infect Dis. 1990. 12:997–1003.
2. Spencer RC. The emergence of epidemic, multiple-antibiotic-resistant Stenotrophomonas (Xanthomonas) maltophilia and Burkholderia (Pseudomonas) cepacia. J Hosp Infect. 1995. 30:Suppl. 453–464.
3. Zuravleff JJ, Yu VL. Infections caused by Pseudomonas maltophilia with emphasis on bacteremia: case reports and a review of the literature. Rev Infect Dis. 1982. 4:1236–1246.
4. You IC, Lee SH, Park YG, Yoon KC. Clinical aspect and prognosis of stenotrophomonas (Xanthomonas) maltophilia keratitis. J Korean Ophthalmol Soc. 2007. 48:889–897.
5. Palleroni NJ, Bradbury JF. Stenotrophomonas, a new bacterial genus for Xanthomonas maltophilia (Hugh 1980) Swings et al. 1983. Int J Syst Bacteriol. 1993. 43:606–609.
6. Senol E. Stenotrophomonas maltophilia: the significance and role as a nosocomial pathogen. J Hosp Infect. 2004. 57:1–7.
7. Bottone EJ, Madayag RM, Qureshi MN. Acanthamoeba keratitis: synergy between amebic and bacterial cocontaminants in contact lens care systems as a prelude to infection. J Clin Microbiol. 1992. 30:2447–2450.
8. Chen YF, Chung PC, Hsiao CH. Stenotrophomonas maltophilia keratitis and scleritis. Chang Gung Med J. 2005. 28:142–150.
9. Bauernfeind A. Comparison of the antibacterial activities of the quinolones Bay 12-8039, gatifloxacin (AM 1155), trovafloxacin, clinafloxacin, levofloxacin and ciprofloxacin. J Antimicrob Chemother. 1997. 40:639–651.
10. Mather R, Karenchak LM, Romanowski EG, Kowalski RP. Fourth generation fluoroquinolones: new weapons in the arsenal of ophthalmic antibiotics. Am J Ophthalmol. 2002. 133:463–466.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download