Abstract
Purpose
To evaluate the clinical characteristics and outcomes of cataract surgery in highly myopic Korean subjects.
Methods
We retrospectively reviewed the medical records of 694 eyes of 694 patients who underwent cataract surgery. The case group included 347 eyes of 347 patients whose axial lengths (AXL) were ≥26.00 mm, and the control group included 347 eyes of 347 patients with AXL between 22.00 and 25.99 mm. Cataract density was determined preoperatively using the Pentacam Scheimpflug imaging system. We compared age at operation, cataract type, coexisting disease, visual prognosis, and complications.
Results
The mean age at the time of the operation was 59.60 ± 12.28 years in the case group and 67.47 ± 11.36 years in the control group. The case group had a larger proportion of nuclear cataracts and posterior subcapsular cataracts (PSC), 40.63% and 26.22%, respectively, versus 25.07% and 11.82%, respectively, in the control group. Postoperative corrected visual acuity showed a negative correlation with AXL (R2 = 0.172), and severe funduscopic findings were related to poor visual prognosis (p = 0.05). The incidence of retinal detachment in the case group after cataract surgery was 1.72%, compared with 0.28% in the control group.
Conclusions
Highly myopic eyes tend to develop cataracts earlier than normal eyes and to have a higher prevalence of coexisting disease and complications, such as retinal detachment. Nuclear cataracts and PSC were more common in the highly myopic group. Poor visual prognosis was associated with longer axial length and retinal myopic degeneration.
The incidence of highly myopic eyes has been increasing, especially in Asian nations [1,2]. These eyes frequently have degenerative changes involving the sclera, choroid, vitreous, and retina. As a result, highly myopic eyes may more commonly have coexisting ocular conditions, such as retinal tears and lattice degeneration. And high myopia is known to be a risk factor and progression factor for primary open angle glaucoma (POAG) [3-6].
High myopia is also a risk factor for cataract formation. A relationship between myopia and cataracts has long been suggested, although some studies have found no relationship [7-9]. Recently, Praveen et al. [10] reported that high myopia was a powerful risk factor for the development of cataracts in young patients. However, to date, there have been no other reported data regarding the relationship between age, high myopia, and cataracts.
Several studies have reported that nuclear cataracts and posterior subcapsular cataracts (PSC) are more common than cortical-type cataracts in patients with high myopia. Cross-sectional data from the Blue Mountains Eye Study revealed a strong association between high myopia and nuclear cataracts and PSC [11], and the Beaver Dam Eye Study showed an association with high myopia and the incidence of cataract surgery, although they did not demonstrate a relationship between myopia and the 5 year incidence of cataracts [12]. However, these studies are population-based, cross-sectional studies, based on refractive myopia. In a study of high myopia, a definition by refractive error may be erroneous, because nucleosclerosis may result in refractive myopia. Praveen et al. [10] reported a prospective case-control study of 800 eyes in an Indian population, which showed an association between nuclear cataracts and axial high myopia. However, unlike in the findings of the Blue Mountains Eye Study, PSC was not associated with high myopia [11-15]. A limitation of these studies is the subjective classification of lens opacity. Intraobserver and interobserver repeatability could not be assessed. As a result, we determined lens density using a Pentacam Scheimpflug imaging system, for which intraobserver and interobserver repeatability have been demonstrated [16,17]. The visual prognosis varies among individuals; it depends on disease conditions, like myopic retinal degeneration, and postoperative complications, like retinal detachment. Tsai et al. reported good final visual outcome in highly myopic eyes, in cases without maculopathy or diabetes [18]. However, highly myopic eyes are frequently accompanied by maculopathy, especially as whose axial lengths (AXL) increases. This study didn't demonstrate the correlation between severity of myopia and the visual outcome. Although many authors agree that highly myopic patients have a higher risk of retinal detachment (RD) than normal AXL patients, there is still controversy about the real risk of RD in highly myopic eyes [19-27]. Our purpose in the present study was to assess the characteristics and visual outcomes of cataract surgery in highly myopic eyes.
This study was a retrospective comparative case-control study based on the review of medical records. In total, 694 eyes of 694 patients who underwent phacoemulsification and posterior chamber intraocular lens (IOL) implantation in our clinic over the last 5 years were included. If both eyes of a patient were involved, one eye was selected randomly. The case group included 347 eyes of 347 patients with AXL ≥26.00 mm, and the control group included 347 eyes of 347 patients with AXL between 22.00 and 25.99 mm. The control group size was comparable to the case group size. The definition of high myopia is not well-established. It is usually defined as eyes with an AXL >26.0 mm or as a spherical equivalent ≥6.0 diopter (D) [11,12]. Because there is no accepted definition for high myopia, we defined high myopia as being AXL ≥26.00 mm. We chose AXL as the parameter because a nuclear cataract with a normal axial length and a normal keratometric value can result in refractive myopia.
AXL values were measured with an A-scan ultrasound device 835 (Humphrey Instruments Inc., Palo Alto, CA, USA) with high frequency (10 MHz), low-energy ultrasound pulses emitted by the probe. AXL was determined until five acceptable values were generated for each eye, and the average value was determined. Patients who underwent cataract surgery for correction of refractive error without cataract were not included. We collected data from 392 highly myopic eyes and, after evaluating for coexisting disease, 45 eyes with previous ocular trauma or surgery were excluded; 22 eyes had received barrier retinal photocoagulation therapy for retinal tears and holes before cataract surgery, and eight eyes had a surgical history, due to RD. There were also 28 eyes with amblyopia, mostly anisometric amblyopia. Additionally, diabetic retinopathy was seen in 17 eyes, glaucoma in 15, and epiretinal membrane in nine.
Retrospective review of the patients' charts included: non-corrected visual acuity (NCVA) and best corrected visual acuity (BCVA), and autorefractor (KR-7100; Topcon, Tokyo, Japan), manual keratometry (Topcon DM-4; Topcon), topography (Orbscan II; Bausch & Lomb, Rochester, NY, USA), A-scan biometry (Humphrey Instruments Inc.), endothelial specular microscope (Noncon Robo-CA SP-8000; Konan Inc., Hyogo, Japan), and dilated fundus examination findings preoperatively. The cataract type was evaluated by a trained observer after pupil dilation using the Lens Opacities Classification System III and the densitometry of the Pentacam Scheimpflug imaging system [28]. The densitometry was evaluated in 82 patients; 22 eyes in the case group and 60 eyes in the control group. NCVA, BCVA, and autorefraction were checked at 1 week, and at 1, 2, and 6 months postoperatively. Data regarding surgical complications, such as posterior capsular tear, zonulysis, remnant cortex, and vitreous loss, were also gathered.
We classified the case group by funduscopic findings: group 1 for normal fundus, group 2 for tigroid appearance, group 3 for posterior staphyloma or chorioretinal atrophy at the macula, and group 4 for choroidal neovascularization diagnosed in fluorescence angiography and indocyanine green angiography. Postoperative visual acuity was compared between groups. Both the SRK 2 and SRK T formulae were used in the IOL calculation. The SRK 2 formula was appled to the control group, and the SRK T formula was applied to the case group.
This research was conducted by medically qualified personnel in accordance with the guidelines of the Catholic University of Korea, School of Medicine Institutional Review Board, and in accordance with the tenets of the Declaration of Helsinki.
The case group included 121 eyes from males and 226 eyes from females; there were no gender differences between the groups. The control group included 105 eyes from males and 242 eyes from females. The mean axial length and spherical equivalent were 28.599 ± 1.940 mm and 13.433 ± 7.182 D, respectively, in the case group, and 23.065 ± 2.172 mm and 0.371 ± 3.275 D, respectively, in the control group. There was no significant difference in preoperative BCVA between the two groups (Table 1). There were unilateral cataracts in 80 eyes (23.69%) in the control group, and in 104 eyes (30.91%) in the highly myopic eyes. Among the other eyes of unilateral highly myopic cataract patients, 36 eyes (29.97%) showed normal AXL. The mean follow-up periods were 7.27 ± 2.16 months in the highly myopic eyes and 6.15 ± 1.74 months in the control group.
The mean age was 59.60 ± 12.28 years in the case group and 67.47 ± 11.36 in the control group (p = 0.001) (Fig. 1). Fig. 1 shows the younger distribution in the highly myopic eyes, versus in the control group, including four subjects underwent cataract surgery in their twenties. These patients did not have any other disease other than high myopia. There was no correlation between AXL and age on surgery in the regression analysis (R2 = 0.2; p = 0.67).
The highly myopic group had a larger proportion of nuclear cataracts and PSC than the control (40.63% and 26.22% vs. 25.07% and 11.82%, respectively) (Table 1). The mean AXLs of each cataract type were 28.27 ± 1.78, 29.10 ± 2.04, and 28.64 ± 2.29 for cortical, nuclear, and PSC, respectively (p = 0.134 by one-way ANOVA test). Eyes with nuclear cataracts had the longest AXL, but the difference was not statistically significantly. Cataract density measured by a Pentacam densitometry was 11.601 ± 4.451 in the normal AXL group (n = 60), and 12.300 ± 3.751 in highly myopic eyes (n = 22) (p = 0.086). AXL and the density showed a positive relationship, but it was not statistically significant (R2 = 4%; p = 0.084) (Fig. 2).
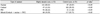
Severe funduscopic findings were related to poor visual prognosis (Pearson chi-squared test; p = 0.048) (Table 2). Eyes with mild retinal changes showed no difference in postoperative visual acuity compared to the control group. However, eyes with posterior staphyloma, chorioretinal atrophy at the macula area, and choroidal neovascularization showed poor visual prognoses. Corrected visual acuity at postoperative 2 months and AXL showed a negative correlation (R2 = 19.8%; p < 0.005) (Fig. 3).
The incidences of RD and posterior capsular opacity were higher in highly myopic eyes (p < 0.001, 0.042). The incidence of RD in highly myopic eyes after cataract surgery was 1.72%, compared with 0.28% in the control group. Postoperative myopic shifts were detected in 17 eyes (4.89%) that were all highly myopic (Table 3).
Our study summarizes the clinical characteristics and postoperative prognosis of cataract surgery in highly myopic eyes, as compared with a normal AXL group. The mean age of the case group was much younger than that of the control group, which is consistent with the study of Praveen et al. [10], which identified high myopia as a risk factor for cataract development. A laboratory-based study identified a relationship between lipid peroxidation and myopic cataracts [29]. An animal study has also shown a correlation between the degree of retinal lipid peroxidation and lens opacity in rodents [30]. These studies provide a possible explanation for the association between high myopia and cataracts; damage to rod outer segments in high myopia results in products that induce cataracts.
We tried to demonstrate the relationship between AXL and cataract density using Pentacam densitometry, of which intraobserver and interobserver repeatability has been demonstrated. It has been shown that there is a relationship between nucleoscelrosis and cortical opacity [16,17]. The highly myopic eyes tend to have a high density of cataracts, but the association is not statistically significant. Further study is needed with a larger number of patients.
Highly myopic cataract patients should undergo careful dilated fundus examinations for retinal tears and glaucoma, which frequently accompany high myopia. We had 22 / 392 (5.6%) patients who needed barrier retinal photocoagulation therapy for retinal tears. Of them, 21 had no complication, like RD, but one patient developed RD after simple phacoemulsification with posterior chamber IOL implantation. The causative tear was not detected preoperatively.
Although there is controversy about PSC development in highly myopic patients, we identified an association between PSC and high myopia. We suggest that different cataract classifications and different observers could be reasons for the controversy. The Emery & Little classification was used by Praveen et al. [10], while the Wisconsin Cataract grading system was used in the Blue Mountains Eye Study and the Beaver Dam study [11,31].
As expected, a more severe the retinal state results in a worse visual outcome. In eyes with mild myopic changes, for example, a tigroid appearance, the visual prognosis is not different from that of the control group. Axial length and visual outcome showed a negative correlation.
RD developed in six eyes (1.72%). Because the mean follow-up was only 7.27 ± 2.16 months, more cases of RD may develop eventually. In the study of Alio et al. [27], the risk of RD increased over time for 5 years.
Our study summarizes the characteristics and visual prognosis of cataract surgery in highly myopic eyes based on the largest study group to date. Further study is needed to examine the pathophysiologic mechanism(s) of cataract formation in highly myopic eyes.
Figures and Tables
Fig. 1
Age distribution in highly myopic eyes and control eyes: mean age was 59.60 ± 12.28 in highly myopic group, 67.47 ± 11.36 in control eyes (p = 0.001). The figure shows younger distribution in highly myopic eyes.

Fig. 2
Pentacam densitometry and whose axial lengths showed positive correlation, was not statistically significant (R2 = 4%, p = 0.084, Pearson's correlation) (n = 82). Averagic densitometric value was 11.601 ± 4.451 in control group (n=60), and 12.300 ± 3.751 in highly myopic eyes (n=22).
Fig. 3
Corrected visual acuity (logarithm of the minimum angle of resolution) at postoperative 2 months and whose axial lengths showed negative correlation (R2 = 19.8%, p < 0.005, Pearson's correlation). BCVA = best corrective visual acuity.
Table 2
Visual prognosis of control and highly myopic eyes, graded by funduscopic findings

Visual acuity was analyzed in logarithm of the minimum angle of resolution value.
Each p-value was compared with control value using paired t-test.
POD = post operative day.
*Controled; †Highly myopic eyes. Group 2, normal fundus; group 3, tigroid appearance; group 4, posterior staphyloma c chorioretinal atrophy at macula; group 5, choroidal neovascularization.
References
1. Wang TJ, Chiang TH, Wang TH, et al. Changes of the ocular refraction among freshmen in National Taiwan University between 1988 and 2005. Eye (Lond). 2009. 23:1168–1169.
2. Lee SJ, Kim JM, Yu BC, et al. Prevalence of myopia in 19-year-old men in gyeongsangnam-do, Ulsan and Busan in 2002. J Korean Ophthalmol Soc. 2009. 50:1392–1403.
3. Hyung SM, Kim DM, Hong C, Youn DH. Optic disc of the myopic eye: relationship between refractive errors and morphometric characteristics. Korean J Ophthalmol. 1992. 6:32–35.
4. Suzuki Y, Iwase A, Araie M, et al. Risk factors for open-angle glaucoma in a Japanese population: the Tajimi Study. Ophthalmology. 2006. 113:1613–1617.
5. Mayama C, Suzuki Y, Araie M, et al. Myopia and advanced-stage open-angle glaucoma. Ophthalmology. 2002. 109:2072–2077.
6. Lee YA, Shih YF, Lin LL, et al. Association between high myopia and progression of visual field loss in primary open-angle glaucoma. J Formos Med Assoc. 2008. 107:952–957.
7. Perkins ES. Cataract: refractive error, diabetes, and morphology. Br J Ophthalmol. 1984. 68:293–297.
8. Weale R. A note on a possible relation between refraction and a disposition for senile nuclear cataract. Br J Ophthalmol. 1980. 64:311–314.
9. Brown NA, Hill AR. Cataract: the relation between myopia and cataract morphology. Br J Ophthalmol. 1987. 71:405–414.
10. Praveen MR, Shah GD, Vasavada AR, et al. A study to explore the risk factors for the early onset of cataract in India. Eye (Lond). 2010. 24:686–694.
11. Lim R, Mitchell P, Cumming RG. Refractive associations with cataract: the Blue Mountains Eye Study. Invest Ophthalmol Vis Sci. 1999. 40:3021–3026.
12. Wong TY, Klein BE, Klein R, et al. Refractive errors and incident cataracts: the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 2001. 42:1449–1454.
13. Tosi GM, Casprini F, Malandrini A, et al. Phacoemulsification without intraocular lens implantation in patients with high myopia: long-term results. J Cataract Refract Surg. 2003. 29:1127–1131.
14. Mehdizadeh M, Ashraf H. Prevalence of cataract type in relation to axial length in subjects with high myopia and emmetropia in an Indian population. Am J Ophthalmol. 2008. 146:329–330.
15. Chen SN, Lin KK, Chao AN, et al. Nuclear sclerotic cataract in young patients in Taiwan. J Cataract Refract Surg. 2003. 29:983–988.
16. Kirkwood BJ, Hendicott PL, Read SA, Pesudovs K. Repeatability and validity of lens densitometry measured with Scheimpflug imaging. J Cataract Refract Surg. 2009. 35:1210–1215.
17. Kim JS, Chung SH, Joo CK. Clinical application of a Scheimpflug system for lens density measurements in phacoemulsification. J Cataract Refract Surg. 2009. 35:1204–1209.
18. Tsai CY, Chang TJ, Kuo LL, et al. Visual outcomes and associated risk factors of cataract surgeries in highly myopic Taiwanese. Ophthalmologica. 2008. 222:130–135.
19. Fernandez-Vega L, Alfonso JF, Villacampa T. Clear lens extraction for the correction of high myopia. Ophthalmology. 2003. 110:2349–2354.
20. Kubaloglu A, Yazicioglu T, Tacer S. Small incision clear lens extraction for correction of high myopia. Eur J Ophthalmol. 2004. 14:1–6.
21. Pucci V, Morselli S, Romanelli F, et al. Clear lens phacoemulsification for correction of high myopia. J Cataract Refract Surg. 2001. 27:896–900.
22. Lee KH, Lee JH. Long-term results of clear lens extraction for severe myopia. J Cataract Refract Surg. 1996. 22:1411–1415.
23. Ripandelli G, Scassa C, Parisi V, et al. Cataract surgery as a risk factor for retinal detachment in very highly myopic eyes. Ophthalmology. 2003. 110:2355–2361.
24. Ravalico G, Michieli C, Vattovani O, Tognetto D. Retinal detachment after cataract extraction and refractive lens exchange in highly myopic patients. J Cataract Refract Surg. 2003. 29:39–44.
25. Jacobi FK, Hessemer V. Pseudophakic retinal detachment in high axial myopia. J Cataract Refract Surg. 1997. 23:1095–1102.
26. Colin J, Robinet A, Cochener B. Retinal detachment after clear lens extraction for high myopia: seven-year follow-up. Ophthalmology. 1999. 106:2281–2284.
27. Alio JL, Ruiz-Moreno JM, Shabayek MH, et al. The risk of retinal detachment in high myopia after small incision coaxial phacoemulsification. Am J Ophthalmol. 2007. 144:93–98.
28. Chylack LT Jr, Wolfe JK, Singer DM, et al. The Longitudinal Study of Cataract Study Group. The Lens Opacities Classification System III. Arch Ophthalmol. 1993. 111:831–836.
29. Micelli-Ferrari T, Vendemiale G, Grattagliano I, et al. Role of lipid peroxidation in the pathogenesis of myopic and senile cataract. Br J Ophthalmol. 1996. 80:840–843.
30. Zigler JS Jr, Bodaness RS, Gery I, Kinoshita JH. Effects of lipid peroxidation products on the rat lens in organ culture: a possible mechanism of cataract initiation in retinal degenerative disease. Arch Biochem Biophys. 1983. 225:149–156.
31. Klein BE, Klein R, Linton KL, et al. Assessment of cataracts from photographs in the Beaver Dam Eye Study. Ophthalmology. 1990. 97:1428–1433.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download