Abstract
Purpose
To describe surgical outcomes for transconjunctival anterior orbitotomy for intraconal cavernous hemangiomas.
Methods
The medical records of 9 consecutive patients with intraconal cavernous hemangiomas who underwent surgical removal by transconjunctival anterior orbitotomy were retrospectively reviewed. The conjunctiva was incised and retracted with a traction suture. For large tumors, a rectus muscle was temporarily disinserted. Tenon's capsule was separated and the tumor was removed with a cryoprobe or clamp. Surgical outcomes, positions of the tumors, methods of approach, and intra- and post-operative complications were evaluated.
Results
The mean follow-up period was 33 ± 6.8 months. No bony orbitotomy was used in this technique and the cosmetic results were very satisfactory. All tumors were removed intact. In 4 patients, tumors were extirpated with the aid of a cryoprobe. No patients had residual proptosis or limitation of ocular movement. No signs of recurrence were noted in any cases at 33 months follow-up. No serious or permanent complications were observed during or after the operation.
Cavernous hemangiomas are relatively common benign tumors of the orbit, and the second most frequent cause of unilateral proptosis after thyroid-related orbitopathy [1-3]. Although benign histopathologically, a cavernous hemangioma may often cause proptosis and interfere with optic nerve function, necessitating surgical intervention. Most of these tumors are located within the intraconal space, so lateral orbitotomy [4] or anterior orbitotomy [5,6] are the preferred methods of surgical removal. Lateral orbitotomy offers a wide surgical field; however, it requires a skin incision, removal of bone tissue, and anatomical reconstruction. Additionally, if the mass is on the medial aspect of the optic nerve the approach must pass by the optic nerve, increasing the risk of optic nerve damage. Transconjunctival anterior orbitotomy (TCAO) is better from a cosmetic perspective and saves time compared to a lateral orbitotomy with bony orbitotomy. TCAO also has a low risk of optic nerve damage because the conjunctival incision can be made according to the location of the mass. In general, the transconjunctival approach to the orbit has been under-utilized because of concern regarding inadequate exposure and postoperative complications, especially when the posterior border of the mass abuts the orbital apex. However, if the characteristics of a cavernous hemangioma are considered, such as encapsulation by a fibrous capsule, TCAO can be utilized in many more cases. The purpose of this study is to describe our surgical outcomes and discuss the advantages and disadvantages of TCAO for intraconal cavernous hemangiomas (ICCHs).
We reviewed the medical records of all patients who underwent TCAO for ICCH at Seoul St. Mary's Hospital between June 1998 and May 2006 by a single surgeon. Indications for the surgery included compression of the optic nerve, proptosis, or limited ocular movements with preoperative diplopia. All identified cases were histologically diagnosed as cavernous hemangiomas. A detailed ocular history and ophthalmological examination were performed. The patients underwent both B-scan ultrasonography and computed tomography (or magnetic resonance imaging) before surgery. The mean follow-up period was 33 ± 6.8 months.
All 9 patients underwent TCAO to remove an ICCH. After spreading the eyelids apart, the conjunctiva was incised at the location of the mass. The resulting flap was opened in a caudal direction. The conjunctiva was then retracted and traction sutures were placed under at least 2 rectus muscles to guide the globe in the desired direction to reach the retrobulbar space. For large tumors, it was often necessary to temporarily disinsert a rectus muscle, depending on the location of the tumor (Table 1). Next, Tenon's capsule was separated from the sclera with cotton-tip applicators and the anterior tip of the tumor was exposed (Fig. 1A). If the tumor was relatively mobile, the anterior portion was frozen with a standard retinal cryoprobe and pulled out gently (4 cases, Fig. 1B). In other instances, the tumor was removed by grasping the tip with a clamp, separating the mass from the sclera with cotton-tip applicators, and slowly pulling out with rotating movements (5 cases). After complete removal, the rectus muscle was reinserted and the conjunctiva was sutured into its original position. Two patients underwent a transconjunctival incision combined with a lateral canthotomy to gain access to cavernous hemangiomas that were deeper and closer to the inferior orbital wall. The position and size of the masses and the methods of surgical approach are shown in Table 1. In 2 patients, the posterior border of the tumor abutted the orbital apex (Fig. 2D).
Clinical ophthalmological evaluation included assessment of visual acuity, exophthalmos (Hertel exophthalmometer), ocular motility, color perception test (Ishihara color plates), biomicroscopy of the anterior segment, kinetic perimetry (Humphrey), and measurements of intraocular pressure using Goldman's tonometer, followed by dilated examination of the fundus. This protocol was performed before the operation, at 1 and 2 weeks after the operation, and then at 3 months intervals.
Eight patients were female and 1 was male. The average age was 40.9 ± 14.3 (range, 20 to 61 years). The presenting symptoms are shown in Table 1. The most common complaint was a painless, gradually progressive proptosis (6 cases) lasting for an average of 48 months (range, 1 to 120 months). The average amount of proptosis was 5.6 mm (range, 2.0 to 12.0 mm). Diplopia or limitation of ocular movement (LOM) was the second most common symptom (4 cases). Other less common symptoms included a lump of the lower lid (2 cases) and decreased visual acuity (2 cases). Clinical signs at presentation included strabismus (4 cases), a pale optic disc (1 case), papilledema with a relative afferent pupillary defect (1 case), and a protruding mass of the lower lid (2 cases).
Orbital cavernous hemangiomas usually exhibit characteristic features on B-scan ultrasonograms, computed tomography (CT)-scans, and magnetic resonance images. The B-scan ultrasonograms of all patients showed high internal reflectivity of a round orbital mass. The CT and magnetic resonance imaging (MRI) displayed well-circumscribed masses that were round or ovoid in shape and sharply delineated from the surrounding tissue (Fig. 2). The tumors were isointense with brain tissue on T1-weighted images and hyperintense on T2-weighted images. The tumors did not alter the orbital bone contours in any of the cases. Lesions immediately behind the eyeball caused flattening of the globe, leading to choroidal atrophy, a pale optic disc, or papilledema in 2 cases (Fig. 2D).
All tumors were completely removed. No patient had any residual proptosis. Two patients who had presented with decreased visual acuity showed postoperative improvements which remained stable after 29 months of follow-up. None of the patients' visual acuity worsened. Diplopia or LOM resolved spontaneously in all 4 patients in whom ocular movements were limited preoperatively. Two patients who did not have diplopia or LOM preoperatively exhibited LOM postoperatively; however, this was improved at 6 months follow-up. The cavernous hemangiomas exhibited a typical gross appearance. The tumors had a round or oval shape, were completely encapsulated, and possessed a typical dark red or purple color (Fig. 1C and 1D). The tumors were all easily dissected from the surrounding tissue and removed with little adherence to other structures.
Cavernous hemangiomas are one of the most common benign tumors of the orbit and are classified as congenital low-flow vascular malformations [1-3]. In our series, females were more likely to be affected than males (female:male = 8:1). A similar preponderance was found by Harris and Jakobiec [7] who reported that 70% of their patients were women. The mean age of our patients was 40.9 (range, 20 to 61 years), which was similar to the series of McNab and Wright [8] and Harris and Jakobiec [7] with mean ages of 42 years (range, 18 to 67) and 47.8 years (range, 19 to 72), respectively. Left eyes were affected more commonly than right eyes (left : right = 6 : 3). This result was also similar to that of McNab and Wright [8] (left : right = 51 : 34). The most common complaint was painless, gradually progressive proptosis (n = 6).
Several surgical methods have been attempted since Asregadoo [9] successfully excised a cavernous hemangioma using the Naffziger approach. Lateral orbitotomy [10] and anterior orbitotomy using a transcutaneous or transconjunctival approach [6] have been the preferred methods. Lateral orbitotomy offers a wide operative field; however, it requires a skin incision, removal of bone tissue, and anatomical reconstruction. This surgery is also time-consuming and leaves a scar.
An ICCH is typically surrounded by a fibrous capsule and composed of large, dilated vascular spaces lined by flattened endothelial cells and fibrous interstitial tissue; also, they do not have a prominent blood supply [11]. This unique structure makes ICCHs suitable for TCAO. In our series all 9 patients underwent TCAO. All tumors were completely removed and no signs of recurrence were noted during the mean follow-up period of 33 months. Both immediate and long-term morphological and aesthetic results were good in all patients. No patient exhibited any residual proptosis. LOM resolved spontaneously in all 4 patients in whom ocular movements were limited preoperatively. Two patients who did not have diplopia or LOM preoperatively exhibited LOM postoperatively; however, this had improved at 6 months follow-up. These immediate postoperative complications of diplopia or LOM may have been caused by over-retraction of thick fat tissue protruding into the operative field. No other immediate or long-term complications were encountered.
In general, the transconjunctival approach to the orbit has been under-utilized because of concern regarding inadequate exposure and postoperative complications such as lower eyelid shortening and ectropion. However, this approach offers several advantages compared to conventional methods. The transconjunctival approach provides excellent exposure of the orbit, leaves no visible scar, possesses a lower risk of the complications associated with transcutaneous techniques such as nerve or muscle damage, and allows for a shorter operation time (usually 30 to 40 minutes) compared to other techniques. Despite these advantages, this approach cannot be used in cases where the tumor margin is ill-defined, adhesions are present, or the risk of malignant changes exists. Current imaging modalities and in particular, MRI, allow for relatively high accuracy in making the diagnosis of orbital cavernous hemangioma at the preoperative stage, making precise surgical planning possible.
Reviewing the literature, we found that many surgeons use the extensive surgical procedure of transcranial superior orbitotomy, especially when the posterior border of the mass abuts the orbital apex. TCAO could be used in these cases if the anterior part of the tumor is found immediately behind the globe. In fact, in 2 of our patients the posterior border of the tumor abutted the orbital apex. Additionally, the transconjunctival approach can be combined with lateral canthotomy to increase exposure. McCord and Moses [12] obtained good results in the repair of orbital floor fractures by using the transconjunctival approach combined with lateral canthotomy to increase exposure. We used a transconjunctival approach combined with lateral canthotomy to extract 2 masses that were either large (3.5 cm diameter) or near the orbital rim.
Surgeons are primarily concerned with two points when planning to remove a mass from the orbital cavity. The first is total removal of the tumor and the second is achieving the best possible cosmetic result. Given the development of minimally invasive surgery and better microsurgical techniques, cosmetic results have become more important to both patients and surgeons. Any injury affecting the bony structures of the orbit may cause serious and unexpected cosmetic results. TCAO is not suitable for the removal of ICCHs in which the margins are ill-defined, adhesions are present, or the risk of malignant changes exist [13-15]. However, in other cases we believe TCAO should be considered the treatment of choice for removal of ICCHs.
Figures and Tables
Fig. 1
Preoperative computed tomography (CT) and magnetic resonance imaging (MRI). (A) Axial CT (mass is ovoid in shape and sharply delineated). (B) Coronal T2-weighted MRI (intraconal mass at the medial portion of the left orbit). (C) Axial T2-weighted MRI (intraconal mass at the inferolateral portion of the left orbit). (D) Axial T2-weighted MRI (lesion immediately behind the eyeball causing flattening of the globe).

Fig. 2
Surgical procedures. (A) Anterior orbitotomy (transconjunctival incision). (B) Extraction of the mass with a cryoprobe. (C,D) Tumor mass (completely encapsulated, dark red or purple in color).
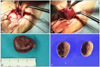
Table 1
Patient data, primary findings, surgical procedures, and outcomes

LOM=limitation of ocular movement; Preop=preoperative; Postop=postoperative; Mo. =months later; TCAO=transconjunctival anterior orbitotomy; SRM=superior rectus muscle; MRM=medial rectus muscle; IRM=inferior rectus muscle; Cryoprobe=extraction with cryoprobe; Hemostat =extraction with hemostat.
*No patients exhibited proptosis postoperatively.
References
1. Casper DS, Chi TL, Trokel SL. Orbital disease: imaging and analysis. 1993. New York: Thieme Medical Publisher;81–97.
2. Scheuerle AF, Steiner HH, Kolling G, et al. Treatment and long-term outcome of patients with orbital cavernomas. Am J Ophthalmol. 2004. 138:237–244.
3. Rootman J. Diseases of the orbit: a multidisciplinary approach. 2003. 2nd ed. Philadelphia: Lippincott Williams & Wilkins;420–460.
4. Forrest AW. Intraorbital tumors. Arch Ophthal. 1949. 41:198–232.
5. Knapp H. A case of carcinoma of the outer sheath of the optic nerve, removed with preservation of the eyeball. Arch Ophthalmol Otol. 1874. 4:323–354.
6. Yan J, Wu Z. Cavernous hemangioma of the orbit: analysis of 214 cases. Orbit. 2004. 23:33–40.
7. Harris GJ, Jakobiec FA. Cavernous hemangioma of the orbit. J Neurosurg. 1979. 51:219–228.
8. McNab AA, Wright JE. Cavernous haemangioma of the orbit. Aust N Z J Ophthalmol. 1989. 17:337–345.
9. Asregadoo ER. Retrobulbar cavernous hemangioma with slowly progressive proptosis. Ann Ophthalmol. 1979. 11:375–378.
10. Shields JA, Shields CL, Eagle RC. Cavernous hemangioma of the orbit. Arch Ophthalmol. 1987. 105:853.
11. Hood CI. Cavernous hemangioma of the orbit. A consideration of pathogenesis with an illustrative case. Arch Ophthalmol. 1970. 83:49–53.
12. McCord CD Jr, Moses JL. Exposure of the inferior orbit with fornix incision and lateral canthotomy. Ophthalmic Surg. 1979. 10:53–63.
13. Geyer O, Godel V, Lazar M. Transconjunctival approach for intraorbital tumors. Arch Ophthalmol. 1988. 106:14–15.
14. Silkiss RZ, Carroll RP. Transconjunctival surgery. Ophthalmic Surg. 1992. 23:288–291.
15. Mullins JB, Holds JB, Branham GH, Thomas JR. Complications of the transconjunctival approach: a review of 400 cases. Arch Otolaryngol Head Neck Surg. 1997. 123:385–388.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download