Abstract
Purpose
To compare clinical outcomes after deep lamellar endothelial keratoplasty (DLEK) with Descemet stripping endothelial keratoplasty (DSEK) performed as initial cases by a single surgeon.
Methods
Sixteen patients with corneal endothelial were enrolled. Eight patients (8 eyes) underwent DLEK and 8 patients (8 eyes) DSEK. We measured uncorrected visual acuity, best corrected visual acuity (BCVA), manifest refraction, corneal endothelial count, interface opacity via Schiempflug imaging, and contrast sensitivity, as well as tracked postoperative complications over the first postoperative year.
Results
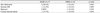
Primary graft failure occurred in two DLEK cases and one DSEK case, all of which were excluded for further analysis. The average 12-month postoperative BCVA was 20/70 in the DLEK group and 20/50 in the DSEK group, with the difference not statistically significant. No significant differences were identified between the 2 groups in terms of mean spherical equivalent and refractive astigmatism, although individuals in the DSEK group tended toward hyperopia. The average endothelial cell count at postoperative month 12 was 1849±494 in the DLEK group and 1643±417 cells/mm2 in the DSEK group, representing cell losses of 26.2% and 31.9%, respectively. No significant differences in endothelial cell count or endothelial cell loss were observed between groups. Early postoperative donor disc dislocation occurred in two eyes after DLEK and one eye after DSEK. Interface opacities and contrast sensitivities were similarly not significantly different between groups.
Lamellar keratoplasty, a surgical technique targeting only diseased corneal layers, represents a major advancement in corneal transplantation. In particular, posterior lamellar keratoplasty (PLK) is an emerging surgical alternative to full-thickness penetrating keratoplasty (PKP) in the treatment of corneal edema resulting from endothelial dysfunction. Terry and Ousley [1,2] further modified the PLK procedure, creating a technique that has come to be referred to as deep lamellar endothelial keratoplasty (DLEK). Because DLEK requires the manual lamellar dissection of the deep corneal stroma from both donor and recipient, the procedure is considered difficult and laborious by surgeons, which has consequently led to the development of Descemet stripping endothelial keratoplasty (DSEK) [3,4].
Although the current DSEK technique seems to be the most commonly performed PLK form, it is unclear whether the classical DSEK is superior to the relatively new DLEK in terms of clinical outcomes, as few reports directly compare the clinical results between techniques. Furthermore, most available case reports are from surgeons who, after fully learning DLEK, abandoned DLEK for DSEK. The learning process involved during the transition period from PKP to PLK is inevitable [5]. We conducted this prospective study to compare the clinical results of DLEK and DSEK, when all procedures were performed by a single surgeon as initial cases. In this way, we attempted to eliminate any bias from the learning process, thus providing a more objective comparison between DLEK and DSEK than other previous studies.
This prospective, comparative, nonrandomized study included a total of 16 eyes from 16 patients with corneal edema resulting either from pseudophakic bullous keratopathy or Fuchs' endothelial dystrophy. All subjects underwent either DLEK or DSEK at the Samsung Medical Center between June 2005 and September 2007. Informed consent was obtained prior to surgery in all cases. The inclusion criteria were patients with vision loss due to endothelial dysfunction. Individuals with significant ocular stromal scarring were excluded, while individuals with a history of well-controlled glaucoma, cataracts, and other comorbidities were allowed to participate. Ours was a non-randomized study, wherein DLEK cases were performed prior to DSEK, as DSEK was developed at a later timepoint. Eight subjects were enrolled in both the DLEK and DSEK groups. Three subjects were excluded from the analysis due to primary graft failure: one individual in the DLEK group and two from the DSEK group. The remaining 13 patients were followed for at least one year, and all surgeries were performed by a single surgeon.
Snellen uncorrected visual acuity (UCVA), best corrected visual acuity (BCVA), refractive astigmatism, corneal topography (Orbscan II, Bausch & Lomb, Rochester, NY, USA), ultrasonic pachymetry (Ultrapach; Eye Technology, St. Paul, MN, USA), and endothelial cell count (SP-8000; Konan Medical Inc., Nishinomiya, Japan) were performed preoperatively and at postoperative months 1, 3, 6, and 12. The rotating Scheimpflug camera (Pentacam; Oculus, Wetzlar, Germany) was used to evaluate the corneal interface opacity at postoperative month 12. Contrast sensitivity testing (MCT 6500; Vistech Consultants Inc., Dayton, OH, USA) was also performed 1 year after surgery.
For each subject, the interface opacity was evaluated by a single examiner using the Pentacam system. This examiner extracted densitometry standard output values from the captured images in a blinded fashion. Image degrees of 45 to 225 and 135 to 315 were used for the right eye, and 225 to 45 and 315 to 135 for the left eye. On each image, measurement points were manually located by cursor at the center of the cornea, and at points 1.5 mm and 3.0 mm left and right of center. The interface opacity was measured at a total of 10 points.
All data were analyzed using SPSS ver. 11.0 (SPSS Inc., Chicago, IL, USA). The Mann-Whitney U-test was used to compare clinical outcomes between DLEK and DSEK at different postoperative time points. p-values of <0.05 were defined as statistically significant in all cases.
Following a 5.0 mm scleral incision in the recipient cornea, deep lamellar dissection was performed to approximately 80% of the corneal thickness using a dissecting spatula (DORC International, Zuidland, Netherlands). The epithelial surface was marked using with methylene blue on a 8.0 mm template, and the posterior lamellar disc was excised from the cornea with curved PLK scissors (DORC International) over 360 degrees. The donor cornea was mounted on an artificial anterior chamber (Bausch & Lomb, St. Louis, MO, USA), dissected in a similar way, and punched out with trephine so to match corneal size between recipient and donor. An 8.0 mm prepared donor posterior disc was folded endothelium to endothelium (separated by viscoelastics [Hyaluronate sodium 10 mg/1 mL; Hyal-2000, LG Life Sciences, Daejeon, Korea]), and then inserted into the anterior chamber through the scleral incision. After unfolding, the donor disc was attached to the recipient stromal bed by injecting air underneath the graft. The scleral incision was then sutured with 10-0 nylon, and the previously injected air was replaced with balanced salt solution (BSS; Alcon Laboratories, Fort Worth, TX, USA) after 15 minutes in order to promote adherence between donor and recipient stromal surfaces.
Donor discs were prepared as described above (size 8.0 mm). A 5-mm superior scleral tunnel incision was made in the recipient cornea, and the epithelial surface marked with a 8.0 mm template for Descemet membrane stripping. The Descemet membrane was scored and stripped using a reverse-Sinskey hook within the epithelial marking. The donor disc was then folded with forceps, inserted into the anterior chamber, and unfolded. Finally, an air bubble was injected to attach the donor disc to the recipient stromal bed. The scleral wound was closed with 10-0 nylon sutures, and the previously injected air was replaced with BSS after 15 minutes.
This study included a total of 16 eyes from 16 patients aged 53 to 78 years. The mean follow-up was 45.5±6.89 months (with a range of 32 to 52 months) for the DLEK group and 13.6±2.7 months (with a range of 11 to 17 months) for the DSEK group. Table 1 summarizes the patients' preoperative characteristics and operative data. Because of the significant difference in follow up period between groups, only data from the first post operative year were analyzed in regards to visual outcome, endothelial cell count, donor-recipient interface opacity, contrast sensitivity testing and complication rates.
The mean preoperative BCVA was 20/1000 (logarithm of the minimum angle of resolution [logMAR], 1.72±0.27) for the DSEK group and 20/1000 (logMAR, 1.70±0.30) for the DLEK group, with no statistically significant difference occurring (p>0.05). Although statistically insignificant, the postoperative UCVA and BCVA for individuals in the DSEK group were observed to be better during the entire follow up period (Fig. 1). At postoperative month 12, the BCVA was 20/70 (logMAR, 0.55±0.28; range, 20/500 to 20/30) for the DLEK group and 20/50 (logMAR, 0.40±0.35; range, 20/200 to 20/25) for the DSEK group, with no statistically significant difference occurring (p=0.642) (Table 2).
Table 2 shows the mean spherical equivalents and refractive astigmatisms between the two groups at postoperative month 12. The mean spherical equivalents between the 2 groups did not vary significantly (p=0.641), although the DSEK group was found to be slightly more hyperopic. Refractive astigmatisms were similarly not significantly different between groups (p=0.201).
Corneal endothelial cell counts were evaluated at postoperative month 12: the donor endothelial cell count was 2507±416 cells/mm2 for the DLEK group and 2415±275 cells/mm2 for the DSEK groups, with no statistically significant difference between groups. At postoperative month 12, the corresponding endothelial densities were 1849±494 and 1643±417 cells/mm2, representing cell losses of 26.2% and 31.9% for the DLEK and DSEK groups, respectively. No significant differences in endothelial cell counts or endothelial cell losses were identified between groups 12 months after surgery (p=0.620, p=0.470) (Table 2; Fig. 2).
Preoperative corneal thickness also did not significantly differ between groups (p=0.590), with thicknesses assessed at 707±169 for the DLEK group and 774±130 µm for the DSEK group. However, a statistically significant difference in mean corneal thickness was observed at postoperative month 12. At this time, the mean corneal thickness was 553±139 µm among individuals in the DLEK group and 677±69 µm among individuals in the DSEK groups (p=0.042) (Table 2).
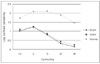
The donor-recipient interface opacity was assessed by averaging data from 10 different Pentacam-measured points. At postoperative month 12, the DSEK group exhibited slightly less interface opacity than the DLEK group, although these results were not significant (p=0.576) (Table 2) and may have occurred from stripping technique performed in the DSEK group. At all spatial frequencies, no significant differences in postoperative contrast sensitivity testing were identified (p>0.05), with Fig. 3 summarizing the mean values at all frequencies.
Table 3 summarizes the data regarding incidence of intra- and postoperative complications occurring after DLEK and DSEK surgeries. The difference in complication rates was not statistically different between the two groups. Disc dislocation occurred in two individuals (28.5%) who underwent DLEK and one individual who underwent DSEK, all of which were rescued with air injection. Due to primary donor failure, one subject (12.5%) in the DLEK group and two subjects (25.0%) in the DSEK group required secondary penetrating keratoplasty due to primary donor failure.
Recently, a number of comparative studies have compared DLEK and DSEK [6-8]. A lamellar corneal transplantation that specifically replaces the diseased endothelium may be performed using either method. Interestingly, the cause of endothelial dysfunction appears to differ between Asians and Caucasians, with pseudophakic bullous keratopathy occurring more commonly in Asians and Fuchs' endothelial dystrophy in Caucasians. As most previously published studies have primarily only enrolled Caucasian subjects, the present study is especially significant, as it was performed in ethnic Koreans and is, to the best of our knowledge, the first comparative study of DLEK and DSEK in Asians.
In this cohort, the average BCVA value at postoperative month 12 was 20/70 for DLEK and 20/50 for DSEK, which are not as good as previously reported values [2,9-13]. However, given the relatively high prevalence of vision-limiting diseases in the enrolled subjects (such as glaucoma) and the relatively low preoperative potential acuity meter values (20/60), we contend that the visual outcomes achieved here were more than satisfactory. Moreover, when we compared the visual outcomes between groups, no significant differences in BCVA were identified at postoperative months 3, 6, or 12, with these results mirroring those of previously published reports. Furthermore, the visual outcomes achieved here were better than those previously reported for PKP [14,15], suggesting that PLK may be a better treatment option for patients with endothelial dysfunction.
In terms of refraction, the DSEK group showed a tendency toward hyperopia (p=0.641). It was recently reported that thickness changes in donor grafts might induce a hyperopic shift, and that this hyperopia decreases with changes in posterior corneal curvature [16]. Data from another study also indicate that donor lenticules with thicker peripheries and thinner centers may act as minus lenses, thus producing a hyperopic shift [17]. Such an effect may have been minimized in the DLEK group in our study, as the donor lenticules were similar in shape to the recipient stromal beds, thereby reducing differences in the thickness between the central and peripheral cornea and ultimately ensuring a good fit. Moreover, the mean refractive astigmatism did not significantly differ between groups, which is consistent with previous reports [2,4,9].
The differences in endothelial cell loss between the DLEK and DSEK groups were not observed to be statistically significant. At 12 months after surgery, the average percentage of endothelium loss was 26.2% in the DLEK group and 31.9% in the DSEK groups. Terry and Ousley [18,19] reported an average cell loss of 29% at 12 months after small-incision surgery and 28% after large-incision DLEK surgery. Similarly, Van Dooren et al. [20] reported a losses of 26% after large-incision posterior lamellar keratoplasty, while data from Gorovoy [13] showed losses of 40% after small-incision DSEK surgery. Overall, our findings concur with these results, although the subjects in our study experienced minimal progressive cell losses between postoperative months 6 and 12, which is different from previous reports. Terry et al. [21] demonstrated that endothelial cell loss after PLK may occur as late as one to two years postoperatively, with donor cell loss substantially accelerating with time. Consequently, long-term data is needed to adequately categorize postoperative cell loss rates.
In the present study, we assessed donor-recipient interface opacity and contrast sensitivity, neither of which has been well characterized to date. Interface opacity may induce higher-order aberrations, contrast sensitivity losses, and visual impairment. Accordingly, we measured interface opacity (using Pentacam) and contrast sensitivity, and analyzed the resulting data for any differences between groups. Although the DLEK group exhibited slightly more interface opacity, the difference between the two groups was not statistically significant. In terms of contrast sensitivity, no significant difference was identified between groups. Interestingly, these results were somewhat unexpected. Since DLEK requires additional recipient stromal dissection, we expected that the DSEK group would experience less interface opacity and have better contrast sensitivity. In a previous study, the mean contrast sensitivity was found to be similar between candidates undergoing penetrating keratoplasty and deep anterior lamellar keratoplasty [22]. Due to the dearth of other studies directly comparing the postoperative interface opacity and contrast sensitivity after DLEK and DSEK, further studies are required if definitive conclusions are to be reached.
Donor disc dislocation occurred in one subject (16.6%) in the DSEK group and in two subjects (28.5%) in the DLEK group. In all cases, donor-lenticule separation was treated by graft repositioning via air or gas bubble tamponade. The donor dislocation rate that occurred here is greater than in the study from Terry and Ousley (who reported a donor dislocation rate of 4% after DLEK) [23], suggesting that the difference may result from surgeon experience. Nevertheless, the rate observed in the present study is consistent with the reported dislocation incidences in other studies (range, 14% to 25%) [5]. Moreover, the dislocation rates observed here were not significantly different between the DLEK and DSEK groups, which supports the findings of Bahar et al. [24]. However, other studies have concluded that the incidence of dislocation is greater in DSEK than DLEK, as DSEK has only one manually dissected surface and consequently a smoother donor-recipient interface [7].
In summary, our study directly compares the clinical outcomes of DLEK and DSEK, when performed as initial cases by a single surgeon. Despite the small case number, we believe that our results reflect an accurate comparison, as we attempted to eliminate the bias resulting from sufficient learning experience of DLEK. Our data indicate that both DLEK and DSEK produce favorable clinical outcomes at 12 months postoperatively, and that the two techniques did not significantly differ in subject visual acuity, refraction, endothelial cell loss, and complication rates. Interestingly, no significant differences were identified in interface opacity and contrast sensitivity between the two techniques. Further studies with larger study populations and longer follow-up periods are required to verify our findings.
Figures and Tables
Fig. 1
The best corrected visual acuities (logarithm of the minimum angle of resolution [logMAR] units) in the deep lamellar endothelial keratoplasty (DLEK) and Descemet stripping endothelial keratoplasty (DSEK) groups versus postoperative time. No significant differences were identified between the 2 groups (p>0.05).
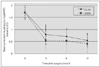
Fig. 2
Longitudinal endothelial cell counts observed over the first postoperative year after deep lamellar endothelial keratoplasty (DLEK) or Descemet stripping endothelial keratoplasty (DSEK). No significant differences were observed between groups at any time point (p>0.05).
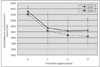
Fig. 3
Longitudinal changes in mean group contrast sensitivity function values. No significant differences were observed between groups (p>0.05). Patients in both groups had notably lower contrast sensitivity function values when compared with normal healthy controls. DLEK=deep lamellar endothelial keratoplasty; DSEK=Descemet stripping endothelial keratoplasty.
Acknowledgements
This study was supported by the Samsung Medical Center Clinical Research Development Program grant (CRS106-20-1).
References
1. Terry MA, Ousley PJ. Replacing the endothelium without corneal surface incisions or sutures: the first United States clinical series using the deep lamellar endothelial keratoplasty procedure. Ophthalmology. 2003. 110:755–764.
2. Terry MA, Ousley PJ. Deep lamellar endothelial keratoplasty visual acuity, astigmatism, and endothelial survival in a large prospective series. Ophthalmology. 2005. 112:1541–1548.
3. Melles GR, Wijdh RH, Nieuwendaal CP. A technique to excise the descemet membrane from a recipient cornea (descemetorhexis). Cornea. 2004. 23:286–288.
4. Price FW Jr, Price MO. Descemet's stripping with endothelial keratoplasty in 50 eyes: a refractive neutral corneal transplant. J Refract Surg. 2005. 21:339–345.
5. Price FW Jr, Price MO. Descemet's stripping with endothelial keratoplasty in 200 eyes: early challenges and techniques to enhance donor adherence. J Cataract Refract Surg. 2006. 32:411–418.
6. Melles GR. Posterior lamellar keratoplasty: DLEK to DSEK to DMEK. Cornea. 2006. 25:879–881.
7. Terry MA, Hoar KL, Wall J, Ousley P. Histology of dislocations in endothelial keratoplasty (DSEK and DLEK): a laboratory-based, surgical solution to dislocation in 100 consecutive DSEK cases. Cornea. 2006. 25:926–932.
8. Allan BD, Terry MA, Price FW Jr, et al. Corneal transplant rejection rate and severity after endothelial keratoplasty. Cornea. 2007. 26:1039–1042.
9. Fogla R, Padmanabhan P. Initial results of small incision deep lamellar endothelial keratoplasty (DLEK). Am J Ophthalmol. 2006. 141:346–351.
10. Terry MA, Ousley PJ. Rapid visual rehabilitation after endothelial transplants with deep lamellar endothelial keratoplasty (DLEK). Cornea. 2004. 23:143–153.
11. Koenig SB, Covert DJ. Early results of small-incision Descemet's stripping and automated endothelial keratoplasty. Ophthalmology. 2007. 114:221–226.
12. Koenig SB, Covert DJ, Dupps WJ Jr, Meisler DM. Visual acuity, refractive error, and endothelial cell density six months after Descemet stripping and automated endothelial keratoplasty (DSAEK). Cornea. 2007. 26:670–674.
13. Gorovoy MS. Descemet-stripping automated endothelial keratoplasty. Cornea. 2006. 25:886–889.
14. Jager MJ, Hermans LJ, Kok JH. Visual results after corneal transplantation. Doc Ophthalmol. 1989. 72:265–271.
15. Schraepen P, Koppen C, Tassignon MJ. Visual acuity after penetrating keratoplasty for pseudophakic and aphakic bullous keratopathy. J Cataract Refract Surg. 2003. 29:482–486.
16. Holz HA, Meyer JJ, Espandar L, et al. Corneal profile analysis after Descemet stripping endothelial keratoplasty and its relationship to postoperative hyperopic shift. J Cataract Refract Surg. 2008. 34:211–214.
17. Yoo SH, Kymionis GD, Deobhakta AA, et al. One-year results and anterior segment optical coherence tomography findings of descemet stripping automated endothelial keratoplasty combined with phacoemulsification. Arch Ophthalmol. 2008. 126:1052–1055.
18. Terry MA. Endothelial keratoplasty: clinical outcomes in the two years following deep lamellar endothelial keratoplasty (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2007. 105:530–563.
19. Ousley PJ, Terry MA. Stability of vision, topography, and endothelial cell density from 1 year to 2 years after deep lamellar endothelial keratoplasty surgery. Ophthalmology. 2005. 112:50–57.
20. Van Dooren B, Mulder PG, Nieuwendaal CP, et al. Endothelial cell density after posterior lamellar keratoplasty (Melles techniques): 3 years follow-up. Am J Ophthalmol. 2004. 138:211–217.
21. Terry MA, Chen ES, Shamie N, et al. Endothelial cell loss after Descemet's stripping endothelial keratoplasty in a large prospective series. Ophthalmology. 2008. 115:488–496. e3.
22. Silva CA, Oliveira ES, Sena Junior MP, Souza LB. Contrast sensitivity in deep anterior lamellar keratoplasty versus penetrating keratoplasty. Arq Bras Oftalmol. 2008. 71:71–74.
23. Terry MA, Ousley PJ. Deep lamellar endothelial keratoplasty: early complications and their management. Cornea. 2006. 25:37–43.
24. Bahar I, Kaiserman I, McAllum P, et al. Comparison of posterior lamellar keratoplasty techniques to penetrating keratoplasty. Ophthalmology. 2008. 115:1525–1533.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download