Abstract
Purpose
To describe etiologies and clinical characteristics of corneal opacities leading patients to seek cosmetic treatments.
Methods
The medical records of 401 patients who presented for cosmetic improvement in corneal opacities between May 2004 and July 2007 were retrospectively reviewed. The following parameters were analyzed: age, gender, cause of corneal opacity, time course of the corneal disease, associated diseases, prior and current cosmetic treatments, visual acuity, location and depth of the corneal opacity, and the presence of either corneal neovascularization or band keratopathy. A single practitioner examined all patients.
Results
The most common causes of corneal opacity were ocular trauma (203 eyes, 50.6%), retinal disease (62 eyes, 15.5%), measles (38 eyes, 9.5%), and congenital etiologies (22 eyes, 5.5%). Prior treatments included iris colored contact lenses (125 eyes, 31.1%) and corneal tattooing (34 eyes, 8.46%). A total of 321 of 401 eyes underwent cosmetic treatment for corneal opacities. The most common treatment performed after the primary visit was corneal tattooing (261 eyes, 64.92%).
Conclusions
This is the first study to investigate the causes and clinical characteristics of patients presenting for cosmetic treatment of corneal opacities rather than for functional improvement. Various cosmetic interventions are available for patients with corneal opacities, and these should be individualized for the needs of each patient.
Diseases affecting the cornea are a major cause of blindness worldwide. These diseases can cause corneal scarring and neovascularization, which can ultimately lead to functional blindness as well as cosmetic difficulties. The treatments for corneal opacities are divided into functional and cosmetic approaches.
Functional treatments are undertaken for visual improvement and include procedures such as corneal transplantation. Due to the tremendous progress in microsurgical reconstructive procedures and immune suppressive therapies, the success rate and indications for corneal transplantation have increased. Cosmetic treatments for corneal opacities are currently used in a small and carefully selected group of patients in whom further surgical procedures will either not result in functional improvement or will not carry risks for phthisis; in these patients cosmetic treatments such as an colored iris contact lens [1,2], a scleral shell prosthesis [3], or corneal tattooing (keratopigmentation) [4,5] may be more appropriate.
A disfigured cornea can impair an individual's self-confidence and can adversely affect one's social and professional lives. Therefore, ophthalmologists might consider cosmetic repair as one of the potential treatment options for corneal opacities in carefully selected cases to improve both the patient's social relationships and personal sense of well-being. As most Asians have dark brown-colored irises, even a small corneal opacity can cause significant cosmetic problems.
As the epidemiology of cosmetic treatments for corneal opacities is not well known, we investigated the causes and clinical characteristics of patients who requested cosmetic treatment for corneal opacities.
The medical records (including anterior segment photography) of 401 patients referred to the Department of Ophthalmology, at Seoul National University Hospital for the purpose of cosmetic repair of their corneal opacities between May 2004 and July 2007 were retrospectively reviewed.
This study included only patients who requested cosmetic correction, as opposed to procedures for visual improvement, for their corneal opacities. Exclusion criteria included patients with ongoing curable ocular disease, a history of either an alteration in visual acuity or the size of the corneal opacity during the past five years, and in whom cosmetic procedures may cause additional visual loss, including children under eight years of age, in whom intervention may irreversibly affect vision development. The study was performed in accordance with the guidelines of the Declaration of Helsinki. A single practitioner (JWK) examined all patients.
The analyzed parameters included age, gender, cause of the corneal opacity, time of onset of corneal disease, associated diseases, previous treatments, visual acuity, location and depth of the corneal opacity, and the presence of either corneal neovascularization or band keratopathy. The locations of the corneal opacities were divided into two zones based on the geographic center of the cornea [6]. A central opacity was defined as being within the central half of the cornea. A peripheral opacity was defined as being located in the peripheral half of the cornea. A total opacity involved the central and more than three quadrants of the peripheral cornea (Fig. 1A). The depth of the opacity was classified as anterior stroma, middle stroma, posterior stroma, or full thickness by a careful slit-lamp examination. Prior (before the first visit) and current (after the first visit) cosmetic treatments of the corneal opacity were evaluated. Post-treatment follow up was performed at one day, one week, one month, three months, six months, and one year. Post-treatment assessment was performed subjectively by evaluating the patient's satisfaction with the cosmetic results and objectively by slit-lamp biomicroscopy.
For keratopigmentation, a sterilized tissue-marking dye (Davidson Marking System®; Bradley Products, Inc., Bloomington, MN, USA) and a 1 mL syringe with a 30-gauge needle, bevel up, were used. After removing the conjunctivalized corneal opacities and calcified plaques with a 69 Beaver blade or by EDTA chelation immediately before tattooing, the dye was injected repeatedly into the corneal stroma until the treated area became a dense black color. Then, after irrigating vigorously with a balanced saline solution, a therapeutic contact lens was placed on the eye and left in place until the cornea had re-epithelized.
In eyes that had a significant limbal deficiency or a severe calcium band, amniotic membrane transplantation was performed with a cryopreserved amniotic membrane in an overlay fashion to promote the recovery of the corneal epithelial defect.
When a sclera shell was employed, a custom-made, modified impression-based prosthesis was fabricated using poly methyl methacrylate by a trained ocularist.
Among the 401 eyes of the 401 patients examined, 244 (60.7%) were in men and 157 (39.3%) were in women. The proportions of right (n=204, 50.9%) and left (n=197, 49.8%) affected eyes was nearly identical. All patients were brown eyed. The mean age was 41.64±15.36 years (range, 13 to 80 years), and the mean age of disease onset was 14.72±15.34 years (range, 0 to 70 years). The mean duration from onset of disease to presentation for corneal opacity treatment was 26.37±15.04 years (range, 1 to 71 years). The mean follow-up time following cosmetic treatment was 15.7±4.1 months (range, 12 to 25 months).
The most common causes of the corneal opacities were ocular trauma (203 eyes, 50.6%), retinal disease (62 eyes, 15.5%), measles (38 eyes, 9.5%), and congenital corneal opacities (22 eyes, 5.5%) (Table 1).
The opacity affected the total cornea in 161 eyes (40.2%) and involved a central location in 132 eyes (32.9%) and a peripheral location in 108 eyes (26.9%). It involved the full-thickness of the cornea in 154 eyes (41.4%), the mid-stroma in 146 eyes (36.4%), the anterior stroma in 87 eyes (21.7%), and the posterior stroma in 14 eyes (3.5%). Associated corneal findings included corneal neovascularization in 256 eyes (63.7%) and band keratopathy in 187 eyes (46.8%). The frequency of band keratopathy was the lowest in cases with congenital corneal opacities and measles-related corneal opacities. In contrast, all eyes with persistent hyperplastic primary vitreous and retinopathy of prematurity pathologies had band keratopathy.
In the 203 patients with corneal opacities due to ocular trauma, the distribution by age at trauma demonstrated that 69.5% (141 eyes) of patients were aged between 0 to 15 years, 3.4% (7 eyes) were between 0 and 2 years, 38.9% (79 eyes) were aged 3 to 6 years, 18.2% (37 eyes) were aged 7 to 10 years, 8.9% (18 eyes) were aged 11 to 15 years, and 28.6% (58 eyes) were aged 15 to 55 years.
The mean frequency of surgical interventions prior to presentation for a cosmetic intervention was 0.92±1.23 times (range, 0 to 9 times).
Despite the difficulty of intraocular examination secondary to the opacity, the most commonly identified associated diseases were strabismus (95 eyes, 23.6%), iris abnormalities (77 eyes, 19.2%), phthisis (37 eyes, 9.2%), and cataracts (32 eyes, 8.0%) (Table 2).
One hundred fifty-nine of 401 eyes had previously undergone cosmetic treatments before the primary visit of this study. Prior cosmetic treatments included colored iris contact lenses (125 eyes, 31.2%) and corneal tattooing (34 eyes, 8.48%). Ninety-four (76%) patients who had previously used colored iris contact lenses were unsatisfied with the results, and all of the patients (a total of 34 eyes) who had undergone prior corneal tattooing complained of fading and hypopigmentation.
Table 3 lists the current cosmetic treatment for corneal opacities following the first visit. Three hundred twenty-one of 401 eyes underwent further cosmetic treatment after the first visit, with the most common treatment being corneal tattooing (261 eyes, 65.1%). Patients who experienced difficulty wearing a colored iris contact lens or scleral shell or who were reluctant to have repeated surgery, underwent corneal tattooing as an alternative. Twenty-nine prior users who experienced no difficulty wearing colored iris contact lenses were asked to continue with this intervention. In four patients who were reluctant to have evisceration or enucleation despite significant phthisis, a scleral shell was applied. Eighty of 401 eyes underwent no cosmetic treatment although an individualized cosmetic treatment was recommended.
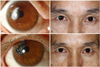
All eyes that underwent cosmetic treatment achieved the desired cosmetic result during a follow-up period of at least one year. In particular, no eye that underwent corneal tattooing demonstrated hypopigmentation, fading, or anterior segment inflammation (Fig. 1B,C).
The visual acuities of the affected eyes and contra-lateral eyes are given in Table 4. Even though the visual acuity of the affected eye was greater than 20/400, 24 patients requested a cosmetic intervention. These patients had a pupil-sparing corneal opacity caused by an open globe injury (8 eyes), measles (5 eyes), or a congenital corneal opacity, such as a limbal dermoid (4 eyes), herpetic keratitis (3 eyes), surgical scar (1 eye), interface opacity of penetrating keratoplasty (PKP) (1 eye), or an unknown cause(s) (2 eyes). All of these opacities were corrected by corneal tattooing, and there were no associated visual losses following the procedures (Fig. 2).
Fourteen patients with a history of a previous PKP requested cosmetic treatment. None requested additional PKP after graft failure due to an irreversible visual loss (due to combined glaucoma in seven eyes, post-PKP trauma in one eye, and reluctance for repeated surgery in six eyes).
Interestingly, in eight patients, a white pupil secondary to a mature cataract caused a more significant cosmetic concern than did their corneal opacity.
Corneal opacities can cause both severe visual loss as well as cosmetic difficulties. The aim of the present study was to evaluate the causes and clinical characteristics of patients presenting for cosmetic repair of corneal opacities. Here, we did not focus on either functional improvement or the efficacy of the individual cosmetic treatment.
Ocular trauma was the most common cause of a disfigured cornea. The preschool age group (3 to 6 years old) appeared to be more susceptible to this type of injury than were the other age groups. Children in this age group tend to be very active and have limited judgment with regard to the potential for injury of their activities [7-11]. Pediatric ocular trauma can cause not only severe corneal opacities but also can limit the opportunities for further treatments, such as PKP, due to deprivation of visual development. Many studies have demonstrated that males tend to be injured more frequently than females, with the male-to-female ratio varying from 2:1 to 4:1 [7-11]. In the current study, we found that 69.5% (141 eyes) of patients in the traumatic group were between 0 to 15 years old (of them, 38.9% [79 eyes] were 3 to 6 years old), and there was a male-to-female ratio of 2.03:1 (male 136, female 67).
Retinal detachment was the second most common cause of corneal opacities. These abnormalities may result from corneal decompensation from repeated intraocular surgery (mean, 1.95 injuries; range, 0 to 5 injuries), extended contact of silicone oil with the cornea (19 eyes, 52.8%), or phthisis (especially in five eyes without surgical intervention despite retinal detachment).
Measles was the third most common cause of corneal opacity in the current study and is the single leading cause of blindness among children in third world countries [12,13]. According to World Health Organization estimates, 30 million children develop measles every year [12]. Approximately 10 to 20% of children with measles require hospitalization for related complications, and about 1% of hospitalized children subsequently lose their vision [13]. In the current study, the mean age at presentation for corneal opacities due to measles was 51 years of age, illustrating that the rate of measles-related visual impairment in Korea has decreased. In fact, there have been few reports of keratopathy caused by measles in Korea in recent years. This is likely due to the low incidence of active measles strains as a result of widespread childhood immunization, improvements in vitamin A-related nutrition [14], and improving socioeconomic conditions. The major complications of measles-related visual impairment are corneal scarring, irido-corneal adhesions, and phthisis bulbi [13]. The current study demonstrated irido-corneal adhesions in ten eyes and phthisis bulbi in one eye.
Among keratitis-related corneal opacities, the most common clinical cause was herpetic keratitis, especially in those with a history of uveitis, early onset, or chronic disease recurrence.
The most common associated disease was sensory strabismus, itself a significant cosmetic problem; 30 patients had undergone prior strabismus surgery.
If fitted and handled properly, colored iris contact lenses can be a useful device for treating disfigured eyes [1,2]. Improved contact lens technology has diminished the use of corneal tattooing. Cosmetic correction with contact lenses is reversible and may be more appropriate for patients reluctant to have repeated surgeries, including tattooing, and who may have a thin cornea (a risk for perforation) or a severe conjuntivalized cornea (a risk for a poor tattooing result). Therefore, we generally recommend colored iris contact lenses as the primary therapy for patients having no previous problems related to contact lenses.
While the most common prior cosmetic treatment was the use of colored iris contact lenses, the most common treatment in the current study was corneal tattooing. This may be due to the fact that many patients enrolled in this study had already experienced difficulty wearing contact lenses previously prescribed at other clinics and did not want to continue with this treatment modality.
Corneal tattooing has several advantages over colored contact lenses [4,5]. The risk of tattoo-associated corneal infection is limited to the postoperative period, and the cost to the patient is only for the initial procedure. Patients also do not have to be concerned about contact lens maintenance. For patients with peripheral corneal opacities and useful vision, corneal tattooing may correct the cosmetic complaint without additional loss of vision, which can be caused by the use of colored contact lenses. Therefore, corneal tattooing may provide a reasonable cosmetic alternative, especially in patients who have difficulties wearing colored contact lenses or in those with a peripheral corneal opacity and useful vision.
Of several potential complications of keratopigmentation, the discoloration of the impregnated pigment is an uncommon but disconcerting side effect [4,5]. In the current study, 34 patients who had previous corneal tattooing at other clinics presented for additional cosmetic intervention due to discoloration of the pigment. Fortunately, all eyes undergoing corneal tattooing at our clinic had cosmetic staining that covered the full opacity area without significant fading or hypopigmentation during a follow-up period of at least one year. Only two patients had a residual corneal opacity following tattooing; this was due to severe calcium plaques in the deep stroma. For these cases, a colored iris contact lens was prescribed. Corneal tattooing combined with amniotic membrane transplantation can be considered for promoting recovery of the corneal epithelial defect and for reducing post-operative discomfort, especially in eyes with a significant limbal deficiency or a severe calcium band.
For the disfigured cornea combined with painless phthisis, the fitting of a prosthesis, such as a scleral shell, over the eye can be a useful intervention. This can maintain the integrity of the orbital anatomy, including fornix volume, enhance appearance, and accelerate the rehabilitation of patients with a disfigured blind eye, with the intent of avoiding evisceration or enucleation [3]. A scleral shell prosthesis is a thin, hard, acrylic shell-like artificial eye designed to be worn over a disfigured eye like a contact lens. Compared to an artificial eye in anophthalmos, the sclera shell prosthesis has several potential advantages [15-17]. It can move in conjunction with eyeball movement, without pegging, and demonstrates a superior cosmetic effect. It also has no orbital implant.related complications such as exposure, infection, or protrusion. Moreover, both evisceration and enucleation can change the orbital anatomy, including fornix volume and size of the palpebral fissure. In the current study, all four patients who had phthisis and who were reluctant to undergo evisceration or enucleation achieved the desired cosmetic result with a scleral shell.
Our study has several limitations. The reported results are probably not applicable to a general ophthalmology practice, as cosmetic treatment of corneal opacities is currently applied to a small and carefully selected group of patients. Additionally, these results may not be able to be generalized to populations with iris colors that are much more difficult to cosmetically match with tattoo dye; all of the patients in the current study had brown-colored irises. Also, since this study focused on the epidemiology of corneal opacities presenting for cosmetic repair and not the efficacy of the cosmetic treatments themselves, choosing the best cosmetic option for the various causes and clinical presentations will require further studies with larger populations, more outcome data, and longer follow-up periods.
To our knowledge, this is the first study to investigate the causes of injury and clinical characteristics of patients presenting for cosmetic treatment of corneal opacities. We have discussed all available cosmetic treatments for corneal opacities and speculated on which treatment would be most appropriate for each patient group through review of previous literature and based on our own experience. The results of this study demonstrate that various cosmetic interventions are available for patients with corneal opacities, and that these should be individualized to each patient.
Figures and Tables
Fig. 1
A 38-year-old male patient with total corneal opacity and band keratopathy of the left eye (A,B). Prior to cosmetic treatment (C). One year post corneal tattooing (keratopigmentation).

References
1. Yildirim N, Basmak H, Sahin A. Prosthetic contact lenses: adventure or miracle. Eye Contact Lens. 2006. 32:102–103.
2. Cole CJ, Vogt U. Medical uses of cosmetic colored contact lenses. Eye Contact Lens. 2006. 32:203–206.
3. Raizada K, Rani D. Ocular prosthesis. Cont Lens Anterior Eye. 2007. 30:152–162.
4. Mannis MJ, Eghbali K, Schwab IR. Keratopigmentation: a review of corneal tattooing. Cornea. 1999. 18:633–637.
5. Pitz S, Jahn R, Frisch L, et al. Corneal tattooing: an alternative treatment for disfiguring corneal scars. Br J Ophthalmol. 2002. 86:397–399.
6. Rezende RA, Uchoa UB, Uchoa R, et al. Congenital corneal opacities in a corneal referral practice. Cornea. 2004. 23:565–570.
7. LaRoche GR, McIntyre L, Schertzer RM. Epidemiology of severe eye injuries in childhood. Ophthalmology. 1988. 95:1603–1607.
8. MacEwen CJ, Baines PS, Desai P. Eye injuries in children: the current picture. Br J Ophthalmol. 1999. 83:933–936.
9. Jandeck C, Kellner U, Bornfeld N, Foerster MH. Open globe injuries in children. Graefes Arch Clin Exp Ophthalmol. 2000. 238:420–426.
10. Strahlman E, Elman M, Daub E, Baker S. Causes of pediatric eye injuries. A population-based study. Arch Ophthalmol. 1990. 108:603–606.
11. Cascairo MA, Mazow ML, Prager TC. Pediatric ocular trauma: a retrospective survey. J Pediatr Ophthalmol Strabismus. 1994. 31:312–317.
12. WHO-UNICEF joint statement on strategies to reduce measles mortality worldwide. Wkly Epidemiol Rec. 2002. 77:224–228.
13. Semba RD, Bloem MW. Measles blindness. Surv Ophthalmol. 2004. 49:243–255.
14. Sommer A. Xerophthalmia and vitamin A status. Prog Retin Eye Res. 1998. 17:9–31.
15. Bailey CS, Buckley RJ. Ocular prostheses and contact lenses. I-Cosmetic devices. BMJ. 1991. 302:1010–1012.
16. Cote RE, Haddad SE. Fitting a prosthesis over phthisis bulbi or discolored blind eyes. Adv Ophthalmic Plast Reconstr Surg. 1990. 8:136–145.
17. Lee HY, Yang JW. Clinical analysis of fitting a sclera shell over phthisis bulbi or discolored blind eyes. J Korean Ophthalmol Soc. 2008. 49:1041–1045.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download