Abstract
Purpose
To evaluate the outcome of the part-time occlusion therapy with near activities in monocular amblyopic patients according to gender, age, severity of amblyopia, and the cause of amblyopia.
Methods
Fifty eight patients who were prescribed part-time occlusion therapy with near activity from July 1998 to October 2004, were included in this retrospective study. All patients were divided into groups by gender, age, severity of amblyopia, and the cause of amblyopia. Main outcome measures were best corrected visual acuity, line improvement, and success rate.
Results
At the end of patch therapy, visual acuity improved from baseline by an average of 3.2±2.5 lines (0.33±0.26 log MAR), and follow-up period was 19.71±14.61 months (1.62±1.20 years). At the last follow-up, visual acuity improved from baseline by an average of 3.7±2.4 lines (0.38±0.26 log MAR), and follow-up period was 37.41±25.83 months (3.08±2.12 years). The success rate was 86% (50 patients) at the end of patch therapy. In 44 patients out of 50 patients (88%), the visual acuity was maintained. While 43 patients out of 47 patients who were less than 7 years old (91%) achieved success, 7 patients out of 11 patients 7 years or older (64%) achieved success (p=0.035).
Although amblyopia is one of the most common ocular disorders in children, preferred treatment modalities and dosage vary a great deal among opthmlologists.1 Occlusion therapy and pharmacologic penalization, using atropine and other cycloplegic drops, represent two of the most common forms of treatment.1,2 Other forms of treatment, including levodopa and carbidopa combination,3 combined optical and atropine penalization,4 contact lenses, or refractive surgery,5,6 have been reported to help with treatment.
Even though occlusion therapy has been the mainstay of treatment of amblyopia, opinions vary on the number of hours of patching per day.2,7-11 Some have questioned the effectiveness of part-time occlusion therapy, but full-time occlusion therapy may have a risk of the occlusion amblyopia and poor compliance.2,12 Especially, young and older children may have poor compliance contributed to big social pressure from their friends and colleagues. Therefore, we prescribed patching only 6 hours per day and recommended combination with at least one hour of near-visual activities while patching to prevent the side effect and poor compliance of full-time patching.
The aim of this study was to evaluate the outcome of the part-time occlusion therapy with near activities in monocular amblyopic patients. We studied the success rate, maintenance rate of total patients, difference according to the gender, age, severity of amblyopia, and the cause of amblyopia, and consecutive changes of visual acuity in 12 months.
This retrospective study included 58 Korean monocular amblyopic patients with strabismic and/or anisometropic amblyopia from July 1998 to October 2004. Patients were recruited from the pediatric ophthalmologic clinic of our hospital, according to the tenets of Declaration of Helsinki. They were prescribed part-time occlusion therapy combined with near activities and showed good compliance.
Eligibility testing included visual acuity, cycloplegic refraction, manifested refraction, fundus examination, and ocular motility test. The major eligibility criteria for the trial included the age from 3 to 10 years, best-corrected visual acuity (BCVA) 20/30 or better in the sound eye, intereye visual acuity difference of 2 or more Snellen lines, the presence of or a history of an amblyogenic factor for strabismus and/or anisometropia, and the wearing of optimal spectacle correction for minimum of 4 weeks at the time of enrollment. Patients with less than 6 months of follow-up after cessation of occlusion therapy were excluded. Strabismic amblyopia was defined as amblyopia (1) in the presence of either a heterotropia at distance and/or near fixation or a history of strabismus surgery and (2) in the absence of refractive error meeting the criteria below for mixed amblyopia. Anisometropic amblyopia was defined as amblyopia in the presence of anisometropia of ≥ 2.00 of spherical or ≥ 1.50 of cylinder diopters, with no measurable heterotropia at distance or near fixation, which persisted after at least 4 weeks of spectacle correction. Mixed amblyopia was defined as amblyopia in the presence of (1) either a heterotropia at distance and/or near fixation or a history of strabismus surgery and (2) anisometropia of ≥ 2.00 of spherical or ≥ 1.50 of cylinder diopters, with no measurable heterotropia at distance or near fixation, which persisted after at least 4 weeks of spectacle correction. The exclusion criteria were following: (1) presence of an organic, ocular cause of reduced visual acuity; (2) prior intraocular surgery; (3) known skin reaction to patch or bandage adhesive; and (4) prior amblyopia treatment.
All patients followed 6 hours daily occlusion therapy (part-time occlusion) with 3 M opticlude, and were followed up every 1-4 months. We recommended at least one hour of near visual activities such as reading a book, dictation, computer or video game, and television watching while patching. At the first visit, measurement of visual acuity, cycloplegic refraction, ocular motility examination, and slit lamp examination were performed. After one week, manifested refraction was performed. At every visit, measurement of visual acuity, manifested refraction, and ocular motility examination were performed. Occlusion therapy was continued until the vision of the amblyopic eye had no further improvement in spite of good compliance after at least 6 months of constant patching. Treatment success was defined as visual acuity more than 20/30, three lines of improvement from baseline, or both.
The patients were divided by gender, age (less than 7 years, 7 years or older), severity of amblyopia; severe (20/400-20/100); moderate (20/80-20/40); mild (20/32-), and the causes of amblyopia (anisometropia, strabismus, mixed type). We evaluated the success rate and the line improvement in the amblyopic eye after the occlusion therapy.
We studied consecutive changes of visual acuity in 36 patients. They were followed up for 12 consecutive months and had available data for analysis. They were divided 3 groups by the cause of amblyopia.
The data were analyzed using SPSS, version 12.0 (SPSS Inc, Chicago, IL, USA). Nominal variables, including gender, age, the cause of amblyopia, severity of amblyopia, and success were analyzed using the Chi square test and Fisher's exact test. Other statistical comparisons among groups used t-test and ANOVA. The null hypothesis was rejected at the 0.05 level of significance.
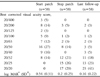
Total 80 amblyopic patients were enrolled this study and 58 patients met the study criteria. They included 28 male (48%), and 30 female (52%). The identified amblyogenic factor was anisometropia in 33 (57%), strabismus in 14 (24%), and mixed type in 11 (19%). The mean age was 4.86±1.62 years. The mean refractive error in the amblyopic eye at enrollment was spherical equivalent of 3.42±2.40 D. The mean best corrected Snellen visual acuity was 0.36±0.20 in the amblyopic eye, 0.80±0.19 in sound eye. The interocular visual acuity difference was 0.44±0.20 (Table 1).
Among the 33 anisometropic amblyopic patients, 14 had hypermetropia (mean spherical equivalent 4.38±2.05 D, 6 had myopia (mean spherical equivalent 5.94±1.24 D), and 13 had astigmatism (mean spherical equivalent 1.39±1.62 D). Among the 14 strabismic amblyopic patients, 3 had refractive accommodative esotropia (mean 13.33±5.80 prism deviation), 4 had partially accommodative esotropia (mean 48.75±8.50 prism deviation), 2 had nonrefractive accommodative esotropia (mean 32.50±3.50 prism deviation), 3 had intermittent exotropia, basic pattern (mean 25.00±5.00 prism deviation), 1 had comitant left hypertropia (30 prism deviation) and 1 right dissociated vertical deviation (10 prism deviation). Among the 11 mixed type amblyopic patients, 3 had refractive accommodative esotropia (mean 23.33±2.89 prism deviation), 3 had nonrefractive accommodative esotropia (mean 35.00±5.00 prism deviation), and 5 had intermittent exotropia, basic pattern (mean 29.00±12.45 prism deviation).
Substantial improvement in visual acuity was achieved (Table 2). At the end of patch therapy, visual acuity improved from baseline by an average of 3.2±2.5 lines (0.33±0.26 log MAR), and follow-up period was 19.71±14.61 months (1.62±1.20 years). At the last follow-up, visual acuity improved from baseline by an average of 3.7±2.4 lines (0.38±0.26 log MAR) and follow-up period was 37.41±25.83 months (3.08±2.12 years).
Fifty patients showed successful results at the end of patch therapy (data now shown). In 44 patients out of 50 patients, the visual acuity was maintained until the last follow-up (Table 3). In 47 patients less than 7 years, 43 (91%) achieved successful results. In 11 patients 7 years or over, 7 (64%) achieved successful results. In terms of age, there was a statistically significant difference of success rate between the two groups, (p=0.035) but not in terms of gender, severity of amblyopia, cause of amblyopia (Table 4).
At the end of patch therapy, visual acuity improved by 5.22±3.24 lines in 18 patients with severe amblyopia (20/400-20/100), by 2.59±1.46 lines in 32 moderate amblyopia (20/80-20/40), and by 1.38±0.74 lines in 8 mild amblyopia (20/32-). In terms of severity of amblyopia, there was significant difference of visual acuity improvement among the three groups (p<0.001) (Table 5).
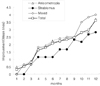
Consecutive changes of visual acuity were evaluated in 36 patients who could be followed up for 12 months (Fig. 1). Gradual linear improvement of visual acuity was noted. There were two steep slopes in the curve, at 3-4 months and at 11-12 months.
There have been many arguments about the amount of occlusion treatment. Some have suggested full-time occlusion treatment and others have suggested part-time occlusion treatment, a few hours per day. In a PEDIG trial, 6 hours per day occlusion treatment produced an improvement in visual acuity that was of similar magnitude to the improvement by full-time occlusion treatment in severely amblyopic children 3 to less than 7 years of age.11 Other reports also suggests part-time occlusion treatment; one hour or more is effective in many children.10-14 In considering side effects due to long time occlusion treatment, such as social stress, irritation and allergy, part-time occlusion treatment should be preferred.
We evaluated the outcome of 6 hour of daily occlusion treatment with near visual activity in monocular amblyopia. The primary outcome was best corrected visual acuity measured each month during follow up. The distribution of visual acuity and line improvement has been shown in table 2. Study group had improved by an average of 3.2 lines at the end of patch therapy. The PEDIG study has shown the improvement of 2.4 lines in 2 hour-patching group and 6 hour-patching group.10 The study by Awan et al have shown the improvement of 2.4 lines in no patching group, 2.9 lines in 3 hour-patching group, and 3.4 lines in 6 hour-patching group.13 The result of our study is not different from other studies (Table 5).
In other reports,15-19 the percentage of treated eyes that maintained their visual acuity after termination of occlusion treatment varied widely, ranging from 40% to 79%. In our study, during the 1.45 years between cessation of treatment and the present examination, visual acuity was maintained or had improved in 88% of the treated eyes (Table 3). Although a number of parameters of our study, such as age at onset of therapy, duration of therapy, and age at final assessment, was different from previous studies, our results show a similar or higher rate of visual acuity maintenance.
In this study, the most significant factor for visual outcome was age (P=0.035) (Table 4). Previous reports showed reduced improvement in the older children and higher success rate in the younger children.11,20 Previous studies22-24 reported that amblyopia can be treated beyond 7 years of age; the success rate in children 7 years or older in this study was 64%. In a PEDIG trial24 for 7 to 17-year-olds with amblyopia ranging from 6/12 to 6/120, 53% of 7 to 12-year-old children responded, to amblyopia treatment with at least ten letters on the ETDRS chart, whereas 25% responded to optical correction alone. In 13 to 17-year-old children who had not been previously treated, 47% responded to amblyopia treatment and 20% responded to optical correction alone.
In other factors, there was no statistical significance. However, as in previous reports,20-29 our study showed that success rate in children with mild amblyopia was higher than that in other children (P=0.32) (Table 4). Although the success rate in severe amblyopia was lower than others, it was still over 50%. In terms of causes of amblyopia, success rate in children with mixed type amblyopia was lower than that in children with other causes (P=0.39) (Table 4).
In our study, severity of amblyopia was not a significant factor toward visual outcome, perhaps due to poor cooperation and selection bias. Children with severe amblyopia are detected at an earlier age than other children and the young children may not cooperate readily to tests. As they become older, they may be checked for more accurate visual acuity and thus exaggerate the good success rate of children with severe amblyopia.
In more severe amblyopia, there was more line improvement, and it was statistically significant (p<0.001) (Table 5). Therefore, we must not give up the treatment in severe amblyopia. Other factors did not show significant differences.
The 36 patients who could be followed up for 12 months showed two steep slopes in the curve, at 3-4 months and at 11-12 months (Fig. 1). It may mean that the effect of occlusion treatment is maximum during the first 3-4 months. It confirms a previous report that there is maximal influence within the first 3 months of initiation of occlusion and it may extend to 6 months.21
One factor for good outcome in our study was near activities while patching. Although many doctors recommend children to do near activities that need hand-eye coordination while patching and they believe it is successful in improving visual acuity in most children, it was unclear whether near activities enhance the effect of occlusion treatment or not. A pilot study25 by PEDIG suggested that children receiving occlusion treatment combined with near activities, actually spent more time performing those activities.
Our study has some limitations. It includes only patients who received the treatment of 6 hour part-time occlusion. We do not report a comparison group with full-time occlusion treatment because we seldom recommend full-time occlusion. Another weakness is that this is a retrospective study based on medical records. Patients in each group are few in number and there may be a selection bias. And the duration of our study is shorter than that of other studies which show the maintenance of improved vision. With longer follow-up, success maintenance may be decreased.
In conclusion, our 6 hour part-time occlusion treatment combined with near activities appears to be favorable in treating 58 children during follow-up time of mean 3.08 years. Total success rate was 86% (50 patients) and 44 (88%) of them maintained or increased their visual acuity in average 1.45 years after end of occlusion treatment. The statistically significant factor influencing success rate was the age of the subject at the start of treatment. Improvement of visual acuity was maximal within 3-4 months of occlusion treatment.
Figures and Tables
References
1. Bacal DA. Amblyopia treatment studies. Curr Opin Ophthalmol. 2004. 15:432–436.
2. von Noorden GK, Campos E. Binocular vision and ocular motility: theory and management of strabismus. 2002. 6th ed. St. Louis: Mosby;537–558.
3. Pandey PK, Chaudhuri Z, Kumar M, et al. Effect of levodopa and carbidopa in human amblyopia. J Pediatr Ophthalmol Strabismus. 2002. 39:81–89.
4. Kaye SB, Chen SI, Price G, et al. Combined optical and atropine penalization for the treatment of strabismic and anisometropic amblyopia. J AAPOS. 2002. 6:289–293.
5. Roberts CJ, Adams GGW. Contact lenses in the management of high anisometropic amblyopia. Eye. 2002. 16:577–579.
6. Autrata R, Rehurek J. Laser-assisted subepithelial keratectomy and photorefractive keratectomy versus conventional treatment of myopic anisometropic amblyopia in children. J Cataract Refract Surg. 2004. 30:74–84.
7. Hiscox F, Strong N, Thompson JR, et al. Occlusion for amblyopia: a comprehensive survey of outcome. Eye. 1992. 6:300–304.
8. Olson RJ, Scott WE. A practical approach to occlusion therapy for amblyopia. Semin Ophthalmol. 1997. 12:161–165.
9. Rutstein RP. Alternative treatment for amblyopia. Probl Optom. 1991. 3:351–354.
10. Repka MX, Beck RW, Holmes JM, et al. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003. 121:603–611.
11. Holmes JM, Kraker RT, Beck RW, et al. A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003. 110:2075–2087.
12. Scott WE, Kutschke PJ, Keech RV, et al. Amblyopia treatment outcomes. J AAPOS. 2005. 9:107–111.
13. Awan M, Proudlock FA, Gottlob I. A randomized controlled trial of unilateral strabismic and mixed amblyopia using occlusion dose monitors to record compliance. Invest Ophthalmol Vis Sci. 2005. 46:1435–1439.
14. Stewart CE, Fielder AR, Stephens DA, Moseley MJ. Treatment of unilateral amblyopia: factors influencing visual outcome. Invest Ophthalmol Vis Sci. 2005. 46:3152–3160.
15. Malik SRK, Virdi PS, Goel BK. Follow-up results of occlusion and pleoptic treatment. Acta Ophthalmol. 1975. 53:620–625.
16. Sparrow JC, Flynn JT. Amblyopia: a long-term follow-up. J Pediatr Ophthalmol. 1977. 14:333–336.
17. Bowman RJC, Williamson TH, Andrews RGL, et al. An inner city preschool visual screening programme: long term visual results. Br J Ophthalmol. 1998. 82:543–548.
18. Levartovsky S, Gottesman N, Shimshoni M, Oliver M. Factors affecting long-term results of successfully treated amblyopia: age at beginning of treatment and age at cessation of monitoring. J Pediatr Ophthalmol Strabismus. 1992. 29:219–223.
19. Leiba H, Shimshoni M, Oliver M, et al. Long-term follow-up of occlusion therapy in amblyopia. Ophthalmology. 2001. 108:1552–1555.
20. Flynn JT, Schiffman J, Feuer W, Corona A. The therapy of amblyopia: an analysis of the results of amblyopia therapy utilizing the pooled data of published studies. Trans Am Ophthalmol Soc. 1998. 96:431–450. discussion 450-3.
21. Cleary M. Efficacy of occlusion for strabismic amblyopia: can an optimal duration be identified? Br J Ophthalmol. 2000. 84:572–578.
22. Mintz Hittner HA, Fernandez KM. Successful amblyopia therapy initiated after age 7 years: compliance cures. Arch Ophthalmol. 2000. 118:1535–1541.
23. Park KH, Hwang JM, Ahn JK. Efficacy of amblyopia therapy initiated after 9 years of age. Eye. 2004. 18:571–574.
24. Scheiman MM, Hertle RW, Beck RW, et al. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005. 123:437–447.
25. Holmes JM, Edwards AR, Beck RW, et al. A randomized pilot study of near activities versus non-near activities during patching therapy for amblyopia. J AAPOS. 2005. 9:129–136.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download