Abstract
Objective
Methods
Results
Conclusion
References
Fig. 1
ICA Case 3. A 54-year-old woman, Hunt and Hess grade 3, presented with Fisher grade 4 SAH. A : Femoral angiogram demonstrates suspicious outpouching on the right supraclinoid carotid artery. B : Angiogram after 7 days revealed saccular outgrowth indicating dissecting aneurysm (white arrow). C : Stent-assisted coiling was performed (Enterprise 4.5/28 mm) with resultant near complete occlusion without contrast leakage (white arrow). D : Follow-up angiography after 2 weeks revealed regrowth of aneurysmal sac. Additional stent-assisted coiling (Enterprise 4.5/28) was performed (white arrow). E : Final angiogram showed near complete occlusion of the aneurysm (white arrow). F : After 6 months, follow-up angiogram showed no evidence of aneurysmal regrowth (white arrow). ICA : internal carotid artery, SAH : subarachnoid hemorrhage.
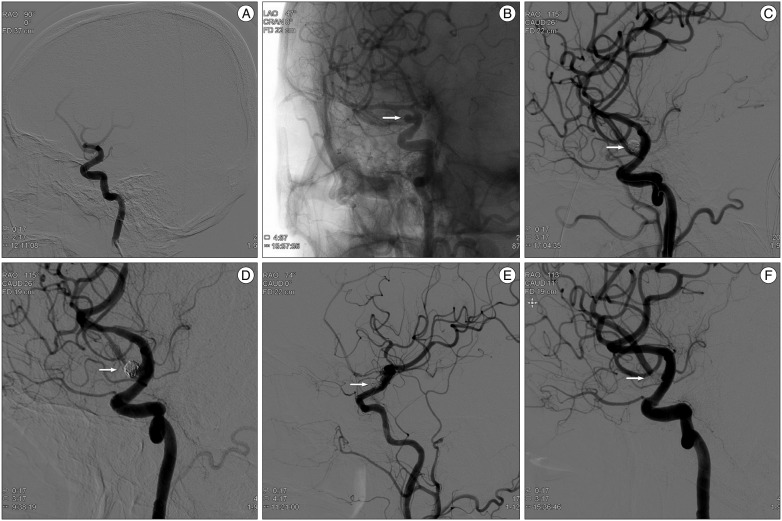
Fig. 2
ICA Case 5. A 39-year-old man, Hunt and Hess grade 2, was presented with Fisher grade 2 SAH. A : Angiogram revealed unremarkable results similar to CT angiogram. He was admitted to the intensive care unit for close observation. B : On the 5th hospital day, angiogram revealed a bleb-like dissecting aneurysm (white arrow) on the right distal carotid artery. C : Double stent-assisted coiling was performed (Enterprise 4.5/22, 4.5/28 mm), and control angiogram showed incomplete occlusion of the dissecting aneurysm (white arrow). D : Follow-up angiogram after 2 weeks failed to show any change in the lesion (white arrow). E : Follow-up angiogram after 6 months revealed further thrombosis within the aneurysm (white arrow). ICA : internal carotid artery, SAH : subarachnoid hemorrhage.
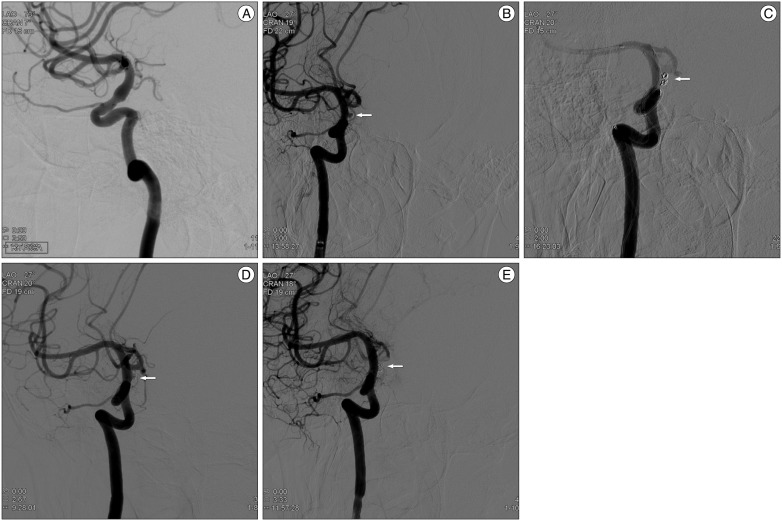
Fig. 3
VA Case 7. A 52-year-old man, Hunt and Hess grade 1, was presented with Fisher grade 4 SAH. A and B : Angiogram demonstrated a definite dissecting aneurysm (white arrow) on the right VA traversing the right posterior inferior cerebellar artery (PICA). Right VA was the dominant vessel, and the dissecting aneurysm incorporated the origin of the right PICA. C : Double stent insertion was performed (Enterprise, 4.5/28, 4.5/37 mm), and then, 14 coils were then placed in the aneurysmal sac with jailing technique (white arrow). D : Final angiogram showed partial occlusion of the aneurysm, but without any contrast leakage. He improved gradually until the 14th hospital day (white arrow). E : Brain CT showed dense infratentorial SAH and intraventricular hemorrhage in the 4th ventricle. He remained unconsciousless for a few days until demise. VA : vertebral artery, SAH : subarachnoid hemorrhage.
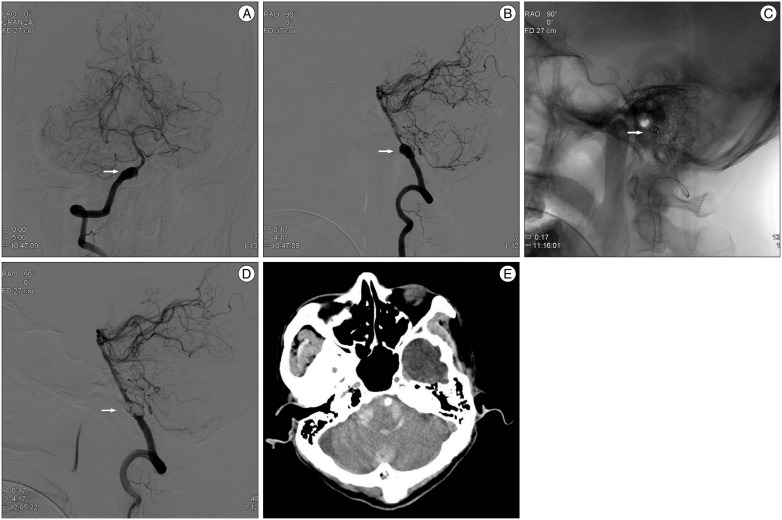
Fig. 4
VA Case 12. A 52-year-old man, Hunt and Hess grade 3, was presented with Fisher grade 4 SAH. A and B : Angiogram demonstrated a typical pearl and string dissection (white arrow) in the right VA incorporating the right PICA. C : Left VA was the dominant vessel, and the dissecting aneurysm in the right VA incorporated the origin of the right PICA. However, the inferior territory of the cerebellum was perfused by the right anterior inferior cerebellar artery and the left PICA. D : Right VA was sacrificed with trapping with coiling. E : Final angiogram showed complete occlusion of the aneurysm and inferior cerebellar perfusion was intact (white arrow). F : After 6 months, follow-up angiogram showed no evidence of recanalization or aneurysmal regrowth (white arrow). VA : vertebral artery, SAH : subarachnoid hemorrhage, PICA : posterior inferior cerebellar artery.
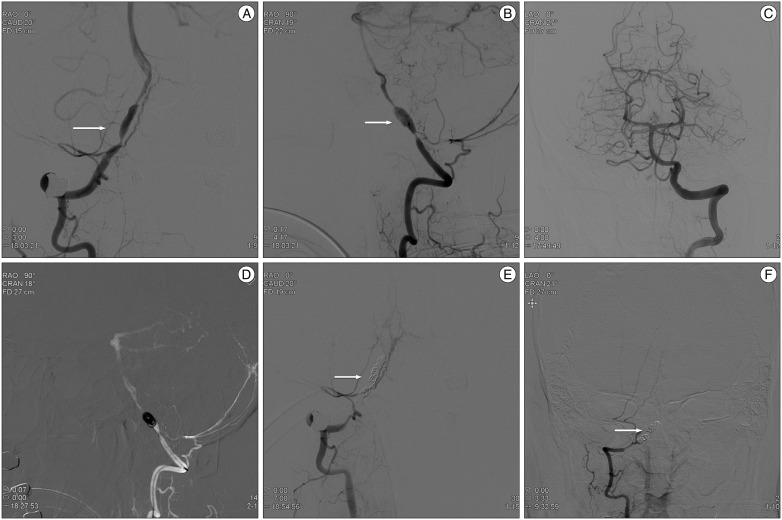
Table 1
Summary of clinical presentations and treatment outcomes in 6 patients with subarachnoid hemorrhage caused by the intracranial internal carotid artery dissections
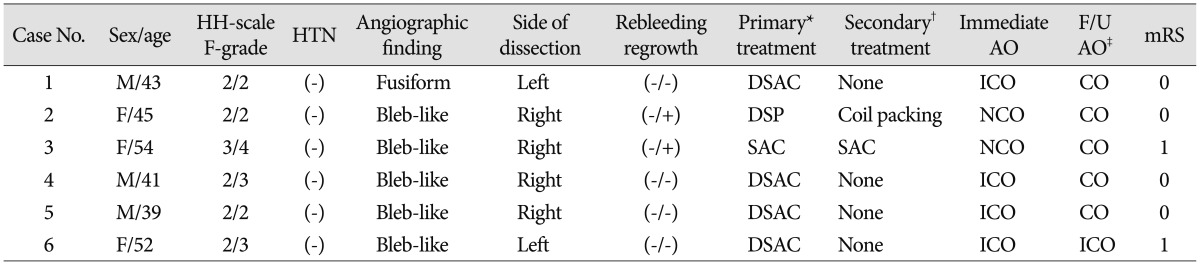
*Primary treatment was performed immediately as soon as the aneurysm was detected, †Secondary treatment was performed when an aneurysms were recurred on follow-up angiography at 2 weeks, ‡Follow-up angiography was performed at 6 months after discharge. AO : angiographic outcome, CO : complete occlusion, DSAC : double stent-assisted coiling, DSP : double stent placement, F-grade : Fisher-grade, HH-scale : Hunt and Hess grade, HTN : hypertension, ICO : incomplete occlusion, mRS : modified Rankin Scale, NCO : near complete occlusion, SAC : single stent-assisted coiling
Table 2
Summary of clinical presentations and treatment outcomes in 9 patients with subarachnoid hemorrhage caused by the intracranial vertebral artery dissections
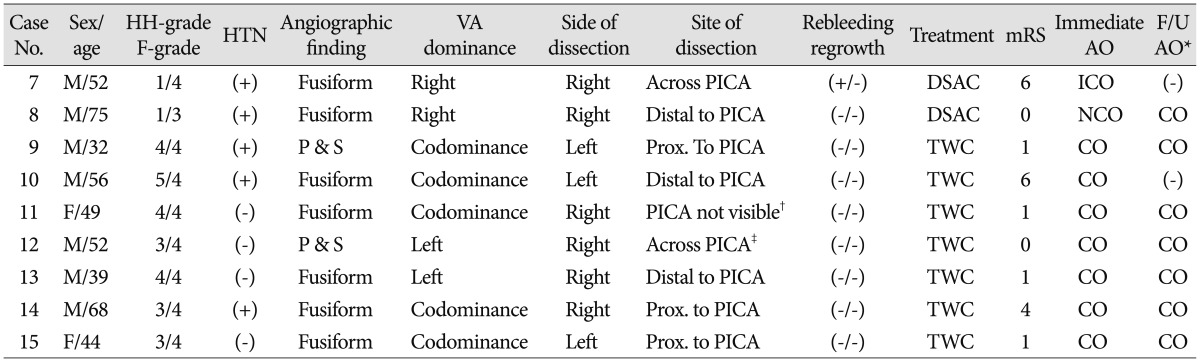
*Follow-up angiography was performed at 6 months after discharge, †Right PICA was not visible, but right AICA perfused right Inferior cerebellar territory, ‡Right AICA, left PICA perfused right inferior cerebellar territory. AICA : anterior inferior cerebellar artery, AO : angiographic outcome, CO : complete occlusion, DSAC : double stent-assisted coiling, F-grade : Fisher-grade, F/U : follow-up, HH-scale : Hunt and Hess grade, ICO : incomplete occlusion, mRS : modified Rankin Scale, NCO : near complete occlusion, P & S : pearl & string, PICA : posterior inferior cerebellar artery, Prox. : proximal, TWC : trapping with coiling, VA : vertebral artery
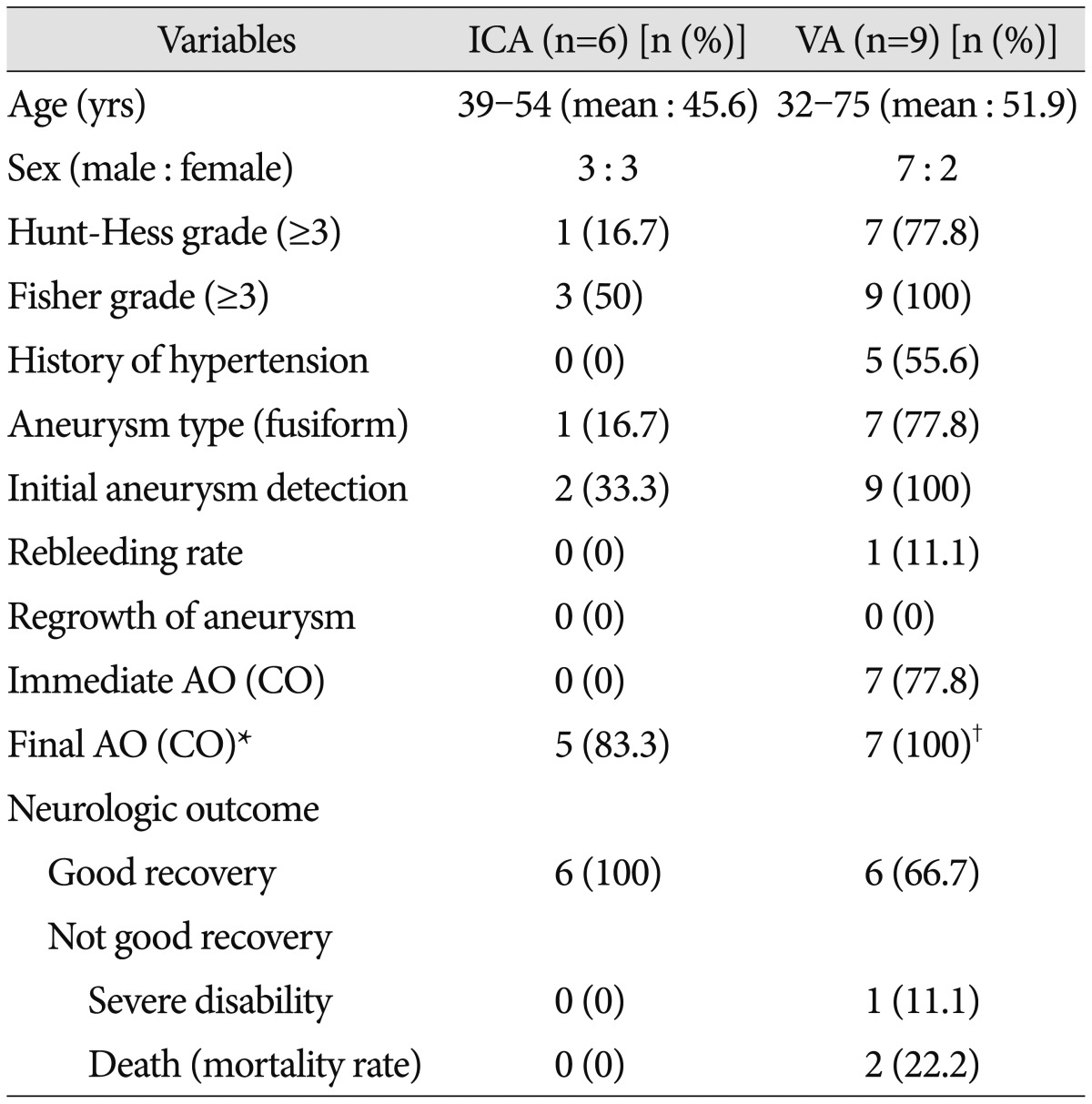
Table 4
Review of endovascular treatment of ruptured ICA and VA dissecting aneurysms
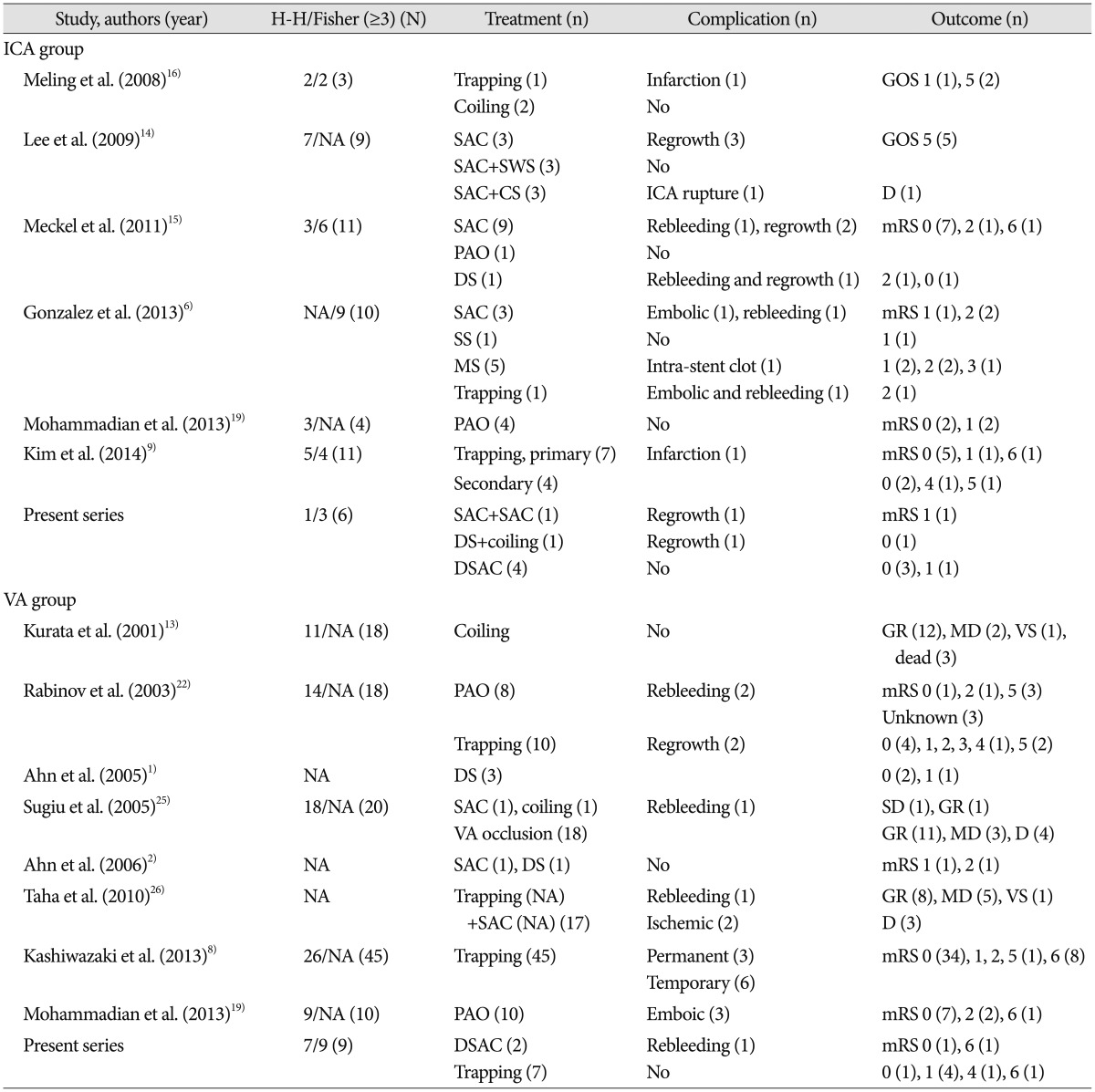
CS : covered stent, D : death, DS : double stenting, DSAC : double stent-assisted coiling, GOS : Glasgow Outcome Scale, GR : good recovery, H-H/Fisher : Hunt-Hess grade/Fisher grade, MD : moderate disability, mRS : modified Rankin Scale, MS : multiple stenting, N : total cases, n : number of cases, NA : not available; PAO : parent artery occlusion, SAC : single stent-assisted coiling, SS : single stenting, SWS : stent within a stent, VS : vegetative state




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download