Abstract
Cervical epidural steroid injection is frequently used in the conservative management of neck pain and cervical radiculopathy. Epidural cervical transforaminal injections are usually well-tolerated with mild side effects such as transient decreased sensory and motor function, or headache due to dural puncture. Although there are a few case reports about adverse effects of cervical epidural injection in the literature, it can cause severe complications such as large hematoma, infarction by spinal vascular injury. Subdural hematoma has been occurred much less common rather than epidural hematoma in the spinal cord. We report a rare catastrophic case of cervical spinal subdural hematoma with quadriparesis after cervical transforaminal epidural block.
Cervical epidural steroid injections are frequently used in the conservative management of neck pain, cervical radiculitis, and cervical radiculopathy51023). Success rate of subjective pain improvement was reported as 64-76%2326). However, although these injections are usually well tolerated, a variety of side effects have been reported. The incidence rate of complication has been reported to low and it mainly occurred in the cause of traumatic injury of the spinal nerve, dural puncture and infections19). Mild common side effects are facial flushing and generalized erythema, dyspnea, nausea, vomiting, dizziness, hypotension, and transient neck stiffness5691020). However, Transforaminal cervical epidural steroid injection have a potential hazard of fatal vascular injury because of the presence of a vessel that communicates with the anterior spinal artery in the posterior aspect of the foramen.
Many recent studies reported the devastated severe complication of spinal cord vascular injury, which can result in infarction, anterior spinal artery syndrome and even death24). Spinal subdural hematoma following cervical epidural steroid injection is a rare spinal vascular injury causing compression of the spinal cord. We report a rare catastrophic case of quadriparetic sequela after cervical epidural block.
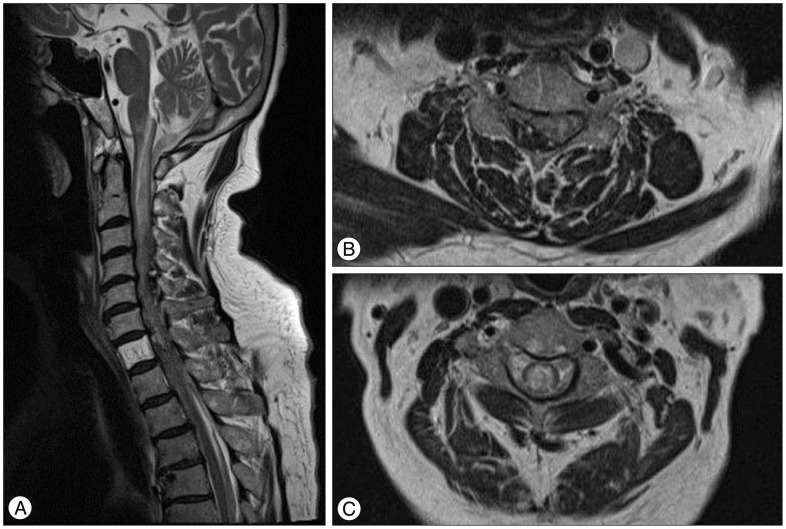
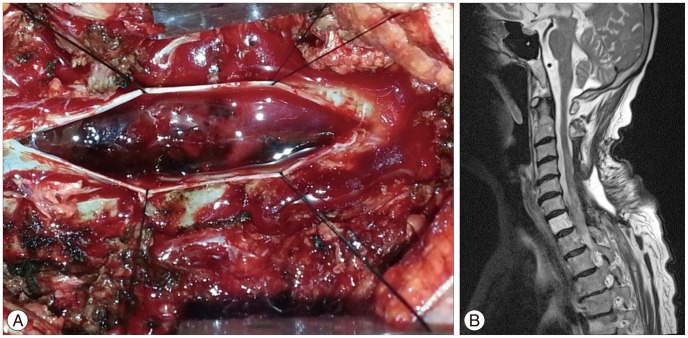
A 70-year-old female patient was transferred to our institute emergency room for acute progressive quadriparesis. The past initial cervical magnetic resonance imagings (MRI) which were checked 2 months ago showed just multiple degenerative changes without any compressive spinal cord lesion. She has been treated with cervical epidural steroid injection for neck pain in local clinic about 5 hours before hospital arrival. After cervical injection, suddenly neurological symptoms occurred and became worse progressively. At the initial neurological examination in our hospital, her mentation was awake and alert. Her pupils were both 2 mm sized and normally reacted to the brightness of light. However, she was unable to move bilateral lower extremities voluntarily at all in response to painful stimuli. Motor grade of upper extremities were 2/5 on right side and 3/5 on left side. Her all senses (pain, temperature, light touch, vibration) was decreased beneath C4-5 level. Cervical MR images showed a mottled mixed signal intensity of nodular lesions in right side of intradural and extramedullary space at level from C3 to C7 and a high intensity of spinal cord with bulging contour of spinal cord that means a spinal cord injury (Fig. 1). We planned to perform emergency operation for decompression and hematoma removal. We performed cervical laminectomy on C3-6 and evacuated hematoma via intradural approach (Fig. 2A). After emergent operation, she needed intensive care to cure bradycardia, hypotension and respiratory function for 3 weeks. Unfortunately she began a late course of motor recuperation. 3 months later, postoperative MR images showed all subdural hematoma was removed and spinal cord compressive lesion was not detected any more (Fig. 2B). Her neurological symptoms improved to motor grade 3 of lower extremities and ambulating with a wheeled walker. A physical examination showed motor strength in right upper extremities of 3/5 and left upper extremities of 4-5. Currently, she was transferred to the rehabilitation department.
Injection of steroids into or adjacent to the spinal canal is performed on a regular basis at the lumbar, thoracic, and cervical levels. Cervical transforaminal epidural corticosteroid injections are generally considered to be safe and commonly recommended for the cervical radiculopathic pain by physicians. On the other hand, some articles reported a very low incidence of serious complications1).
It is not exactly known that the prevalence of these serious complications and the mechanisms8). Inadvertent intra-arterial injection is the most often-hypothesized mechanism and the injected particulate corticosteroids might cause embolus and infarction711). Rozin et al.24) reported the case of death after transforaminal epidural steroid injection and he confirmed the cause of death was the vertebral artery dissection. Scanlon et al.25) insisted that direct arterial damage leads to dissection or thrombosis, or that vessel puncture and needle-induced vasospasms create a downstream infarction. Hodges et al.13) reported two cases having permanent neurologic sequela after cervical dural puncture. Reitman and Watters22) reported one case of a subdural hematoma following a cervical epidural steroid injection. Acute quadriplegia occurred and progressively has been recovered partially after surgical decompression, but the patient was died by meningitis. However, these report did not specify the mechanism of hematoma development. Bose3) report one case with quadriparesis following cervical epidural steroid injection. He hypothesized the patients may have suffered a vascular event from a cervical epidural injection.
Huntoon1516) reported anterior spinal artery syndrome as a complication of transforaminal epidural steroid injections. He reported anatomy of the cervical intervertebral foramina that ascending cervical and deep cervical arteries anastomosing with the vertebral artery posterior to the spinal nerves. Vascular injury may be occurred by epidural injection cervical transforaminal due to the needle cannulating a segmental artery contributed by the ascending cervical artery.
In our case of quadriparesis, acute large amount of subdural hematoma occurred after cervical epidural transforaminal steroid injection. There is high probabilty of direct arterial damage by vessel puncture because branches of radicular artery can communicate with the anterior spinal artery in the posterior aspect of the foramen.
Generally, the radicular artery arise from the vertebral artery and the ascending cervical artery and accompany the spinal nerve and its roots to the spinal cord29). This radicular artery tended to enter the foramina just inferior to the exiting spinal nerve and follow a tortuous course along the inferior and anterior aspect of the spinal nerve until it penetrated the dura to join the anterior or posterior spinal artery14). During transforaminal injection, the vertebral artery injury can be avoided by keeping the needle over the posterior aspect of the foramen. However, these radicular arterial branches may arise variably from the vertebral and especially the posterior branch can lie anterior to the course of the needle insertion16). Usual maneuver that handle the needle tip to touch the superior articular process and then redirected to enter the dorsal midpoint of the foramen can cause the injury of posterior branch of radicular artery.
To avoid unintended intravascular injection, several methods such as aspiration for blood with a syringe, radio-opaque contrast injection have been introduced. However, these techniques were shown to miss more than 50% of vascular injections, because the vascular contrast patterns have a fleeting appearance and more often spread to epidural space simultaneously27). Careful observation of the dynamic flow of contrast under live fluoroscopic view is necessary and important. Live observation using digital subtraction angiography helps us to identify more exact vascular anatomical structures and improve detection of inadvertent vascular injections24). Anesthetic test doses before corticosteroid injection are used to identify vascular entry of medications undetected by other methods but can produce adverse outcomes including transient paresis or seizure172728). In addition, intravascular anesthetics can result in cardiovascular toxicity or even death1221).
We are suggesting the strategies of preventative vascular injury in the following manner : 1) the use of high-quality imaging guidance with contrast injection and possibly digital subtraction fluoroscopy, 2) the use of blunt/pencil point needles with side port to avoid sharp needle penetration and damage to critical vessels, 3) the use of local anesthetic test dosing before injection of particulate steroid, 4) the use of steroid spreading by diffusion into the foramen with keeping needle distance from foramen.
We report a rare case of a patient who experienced serious quadriparetic complication due subdural hematoma after cervical epidural injection. The cervical transforaminal epidural injection is effective to treat cervical radiculopathy. However, the radicular artery is vulnerable and it may cause severe complications such as embolous, infarction, dissection and even catastrophic hematoma.
References
1. Abram SE, O'Connor TC. Complications associated with epidural steroid injections. Reg Anesth. 1996; 21:149–162. PMID: 8829408.
2. Baker R, Dreyfuss P, Mercer S, Bogduk N. Cervical transforaminal injection of corticosteroids into a radicular artery : a possible mechanism for spinal cord injury. Pain. 2003; 103:211–215. PMID: 12749976.

3. Bose B. Quadriparesis following cervical epidural steroid injections : case report and review of the literature. Spine J. 2005; 5:558–563. PMID: 16153586.

4. Brouwers PJ, Kottink EJ, Simon MA, Prevo RL. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. Pain. 2001; 91:397–399. PMID: 11275398.

5. Cicala RS, Thoni K, Angel JJ. Long-term results of cervical epidural steroid injections. Clin J Pain. 1989; 5:143–145. PMID: 2520395.

6. Cicala RS, Westbrook L, Angel JJ. Side effects and complications of cervical epidural steroid injections. J Pain Symptom Manage. 1989; 4:64–66. PMID: 2732522.

7. Derby R, Lee SH, Date ES, Lee JH, Lee CH. Size and aggregation of corticosteroids used for epidural injections. Pain Med. 2008; 9:227–234. PMID: 18298706.

8. Derby R, Lee SH, Kim BJ, Chen Y, Seo KS. Complications following cervical epidural steroid injections by expert interventionalists in 2003. Pain Physician. 2004; 7:445–449. PMID: 16858486.
9. DeSio JM, Kahn CH, Warfield CA. Facial flushing and/or generalized erythema after epidural steroid injection. Anesth Analg. 1995; 80:617–619. PMID: 7864437.

10. Ferrante FM, Wilson SP, Iacobo C, Orav EJ, Rocco AG, Lipson S. Clinical classification as a predictor of therapeutic outcome after cervical epidural steroid injection. Spine (Phila Pa 1976). 1993; 18:730–736. PMID: 8516703.

11. Furman MB, Giovanniello MT, O'Brien EM. Incidence of intravascular penetration in transforaminal cervical epidural steroid injections. Spine (Phila Pa 1976). 2003; 28:21–25. PMID: 12544950.

12. Heath ML. Deaths after intravenous regional anaesthesia. Br Med J (Clin Res Ed). 1982; 285:913–914.

13. Hodges SD, Castleberg RL, Miller T, Ward R, Thornburg C. Cervical epidural steroid injection with intrinsic spinal cord damage. Two case reports. Spine (Phila Pa 1976). 1998; 23:2137–2142. discussion 2141-2142PMID: 9794061.
14. Hoeft MA, Rathmell JP, Monsey RD, Fonda BJ. Cervical transforaminal injection and the radicular artery : variation in anatomical location within the cervical intervertebral foramina. Reg Anesth Pain Med. 2006; 31:270–274. PMID: 16701194.

15. Huntoon MA. Anatomy of the cervical intervertebral foramina : vulnerable arteries and ischemic neurologic injuries after transforaminal epidural injections. Pain. 2005; 117:104–111. PMID: 16055268.

16. Huntoon MA. Anterior spinal artery syndrome as a complication of transforaminal epidural steroid injections. Semin Pain Med. 2004; 2:204–207.

17. Karasek M, Bogduk N. Temporary neurologic deficit after cervical transforaminal injection of local anesthetic. Pain Med. 2004; 5:202–205. PMID: 15209975.

18. Kim SB, Kim MK, Kim KD, Lim YJ. Unintended complication of intracranial subdural hematoma after percutaneous epidural neuroplasty. J Korean Neurosurg Soc. 2014; 55:170–172. PMID: 24851156.

19. Muro K, O'Shaughnessy B, Ganju A. Infarction of the cervical spinal cord following multilevel transforaminal epidural steroid injection : case report and review of the literature. J Spinal Cord Med. 2007; 30:385–388. PMID: 17853663.

20. Nelson DA. Dangers from methylprednisolone acetate therapy by intraspinal injection. Arch Neurol. 1988; 45:804–806. PMID: 3291836.

21. Petitjeans F, Mion G, Puidupin M, Tourtier JP, Hutson C, Saissy JM. Tachycardia and convulsions induced by accidental intravascular ropivacaine injection during sciatic block. Acta Anaesthesiol Scand. 2002; 46:616–617. PMID: 12027861.

22. Reitman CA, Watters W 3rd. Subdural hematoma after cervical epidural steroid injection. Spine (Phila Pa 1976). 2002; 27:E174–E176. PMID: 11884923.

23. Rowlingson JC, Kirschenbaum LP. Epidural analgesic techniques in the management of cervical pain. Anesth Analg. 1986; 65:938–942. PMID: 3017152.

24. Rozin L, Rozin R, Koehler SA, Shakir A, Ladham S, Barmada M, et al. Death during transforaminal epidural steroid nerve root block (C7) due to perforation of the left vertebral artery. Am J Forensic Med Pathol. 2003; 24:351–355. PMID: 14634474.

25. Scanlon GC, Moeller-Bertram T, Romanowsky SM, Wallace MS. Cervical transforaminal epidural steroid injections : more dangerous than we think? Spine (Phila Pa 1976). 2007; 32:1249–1256. PMID: 17495784.
26. Shulman M. Treatment of neck pain with cervical epidural steroid injection. Reg Anesth Pain Med. 1986; 11:92–94.
27. Smuck M, Fuller BJ, Chiodo A, Benny B, Singaracharlu B, Tong H, et al. Accuracy of intermittent fluoroscopy to detect intravascular injection during transforaminal epidural injections. Spine (Phila Pa 1976). 2008; 33:E205–E210. PMID: 18379390.

28. Smuck M, Maxwell MD, Kennedy D, Rittenberg JD, Lansberg MG, Plastaras CT. Utility of the anesthetic test dose to avoid catastrophic injury during cervical transforaminal epidural injections. Spine J. 2010; 10:857–864. PMID: 20692210.

Fig. 1
A : Preoperative sagittal T2 weighted MR image shows the mottled mixed signal intensity nodular lesions in right side of intradural and extramedullary space at the level from medulla and cerebellum to C7 level. B and C : Axial T2 weighted MR images show high signal intensity of spinal cord with bulging contour that means spinal cord injury.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download