Abstract
Postdural punctural headache (PDPH) following spinal anesthesia is due to intracranial hypotension caused by cerebrospinal fluid (CSF) leakage, and it is occasionally accompanied by an intracranial hematoma. To the best of our knowledge, an intracranial chronic subdural hematoma (CSDH) presenting with an intractable headache after a cervical epidural steroid injection (ESI) has not been reported. A 39-year-old woman without any history of trauma underwent a cervical ESI for a herniated nucleus pulposus at the C5-6 level. One month later, she presented with a severe headache that was not relieved by analgesic medication, which changed in character from being positional to non-positional during the preceding month. Brain magnetic resonance imaging revealed a CSDH along the left convexity. Emergency burr-hole drainage was performed and the headache abated. This report indicates that an intracranial CSDH should be considered a possible complication after ESI. In addition, the event of an intractable and changing PDPH after ESI suggests further evaluation for diagnosis of an intracranial hematoma.
Epidural steroid injections (ESIs) are commonly used in the treatment of radicular pain. ESIs are generally considered safe, but accidental dural punctures have been reported on rare occasions1). In turn, dural punctures occasionally have been reported to cause postdural puncture headaches (PDPHs), owing to leakage of cerebrospinal fluid (CSF)3). Although one case of a scanty intracranial acute subdural hematoma after lumbar ESI has been reported previously9), an intracranial chronic subdural hematoma (CSDH) following ESI has never been reported in the literature. To the best of our knowledge, we here report the first case of an intracranial CSDH following cervical ESI, and discuss the clinical importance of a persistent headache after ESI.
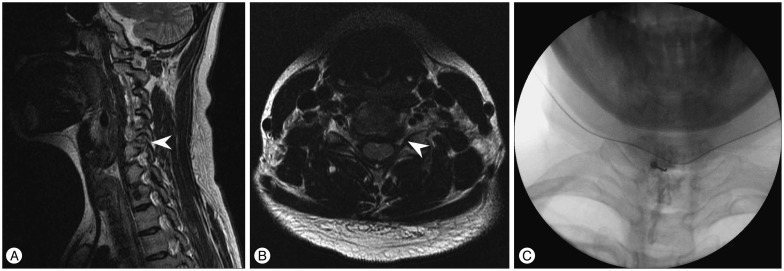
On 27th January 2014, a healthy 39-year-old woman presented to our pain clinic with chronic left arm pain. She had no history of trauma, and neurological examinations revealed pain without motor weakness along the C6 sensory dermatome of the left arm. Cervical magnetic resonance imaging (MRI) demonstrated a left C5-6 herniated nucleus pulposus (Fig. 1A, B). She subsequently underwent a fluoroscopically-guided C6 epidural steroid injection (Fig. 1C). Since then the symptom improved.
Following the procedure, she gradually developed a mild headache that was aggravated while in the upright position. Five days after ESI, she revisited the pain clinic, and a brain computed tomography (CT) scan showed unremarkable findings. However, her headache worsened within 10 minutes after sitting, and was accompanied by nausea, vomiting and neck stiffness. In addition, her headache was extremely aggravated during a Valsava maneuver. PDPH was suspected, and she underwent conservative treatment with bed rest and analgesics. During hospitalization, her headache was successfully relieved, and she was discharged.
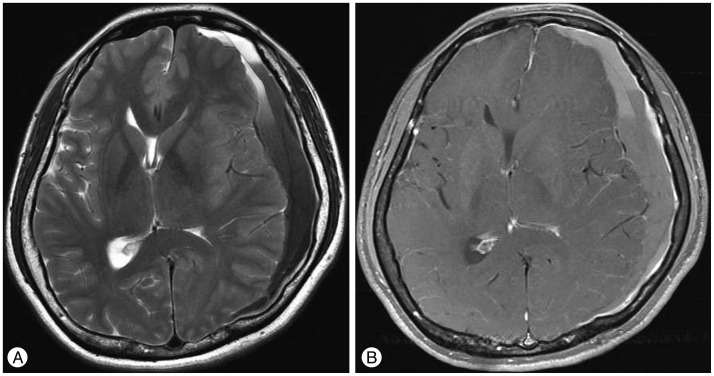
A month later, she visited the emergency department and presented with a persistent and severe headache. The headache did not improve with analgesics, and it had changed in character from being positional to non-positional. Her neurological examinations were normal. Brain MRI revealed a massive chronic subdural hematoma along the left convexity with mixed signals on T1- and T2-weighted images (Fig. 2). There were no vascular abnormalities or enhancing lesions.
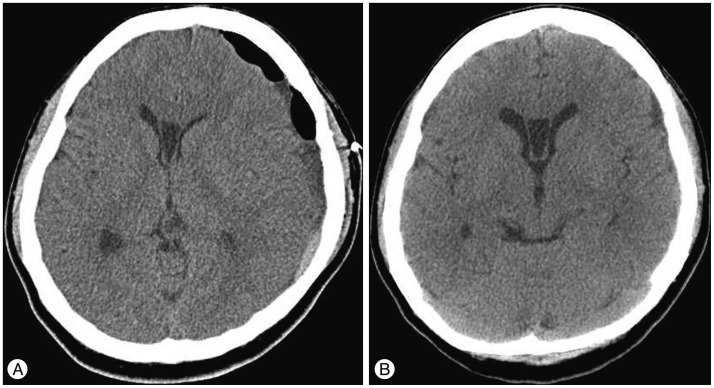
Emergency burr-hole drainage was performed, and her headache improved immediately after the surgery. She has not complained of headaches since, and was discharged 5 days after surgery. At the latest follow-up, brain CT revealed unremarkable findings (Fig. 3).
Epidural steroid injections are frequently used to treat spinal radiculopathy resulting from herniated nucleus pulposus and spinal stenosis1). Major complications of ESI include intracranial subdural air, spinal subdural hematoma, and cauda equina syndrome16810); however, post-ESI complications are relatively rare, occuring at a rate of approximately 9.6%, as reported by Botwin et al.2). PDPH is a well-known complication of ESI, with a reported incidence of 1.4-6%. Although the pathophysiological mechanisms underlying PDPH are currently unclear, a possible role for CSF leakage has been suggested, with Gass et al.4) reporting that CSF leakage results in a downward displacement of intracranial structures, which causes cerebral hypotension and stretches intracranial pain-sensitive structures.
The characteristics of PDPH change according to position, with the pain worsening when the patient is in the upright position, while improving when recumbent. However, Nolte et al.8) reported that the changing nature of a headache (including non-positional headaches) and unresponsiveness to conventional therapy are warning signs that necessitate a search for cerebral lesions by brain CT or MRI. In the case presented herein, the patient's headache was initially positional, but changed in character and became unresponsive to analgesic medication over time.
Chronic subdural hematomas after puncture of the spinal dura have been previously reported following spinal anesthesia. Moradi et al.7) reported that intracranial hypotension from CSF leakage after dural puncture can lead to a caudal shift of the brain, with subsequent traction on the arachnoid membrane and dural veins. This damages the blood vessels, which could result in blood leakage and the formation of a subdural hematoma. However, with ESI, one such case has been reported previously, which involved a scanty intracranial acute subdural hematoma after lumbar ESI. The reason for this involves the difference between spinal anesthesia and ESI. Spinal anesthesia is a form of regional anesthesia involving injection of a local anesthetic into the subarachnoid space, whereas ESI is a steroid injection into the spinal epidural space. Therefore, CSF leakage and PDPH after spinal anesthesia are more frequent than after ESI. To our knowledge, the present case is the first report of an intracranial CSDH, which is a potentially fatal complication, following cervical ESI.
Treatment for PDPH consists of bed rest, hydration, and analgesics. If a severe headache persists, an epidural blood patch may be indicated to prevent further CSF leakage5). However, an intractable headache changing in character from positional to non-positional requires immediate consultation with a neurosurgeon, and the patient should be monitored for evidence of progressive neurological deficits. Upon diagnosis of subdural hematoma by cranial imaging, the most appropriate conservative or surgical treatment must be considered.
Acknowledgements
We thank Wade Martin of Medical Research International for his critical review of this manuscript.
References
1. Bilir A, Gulec S. Cauda equina syndrome after epidural steroid injection : a case report. J Manipulative Physiol Ther. 2006; 29:492.e1–492.e3. PMID: 16904497.
2. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Freeman TL, Slaten WK. Complications of fluoroscopically guided transforaminal lumbar epidural injections. Arch Phys Med Rehabil. 2000; 81:1045–1050. PMID: 10943753.

3. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Hanna A, Rittenberg J, et al. Complications of fluoroscopically guided caudal epidural injections. Am J Phys Med Rehabil. 2001; 80:416–424. PMID: 11399002.

4. Gass H, Goldstein AS, Ruskin R, Leopold NA. Chronic postmyelogram headache. Isotopic demonstration of dural leak and surgical cure. Arch Neurol. 1971; 25:168–170. PMID: 5109715.
5. Huston CW. Cervical epidural steroid injections in the management of cervical radiculitis : interlaminar versus transforaminal. A review. Curr Rev Musculoskelet Med. 2009; 2:30–42.

6. Katz JA, Lukin R, Bridenbaugh PO, Gunzenhauser L. Subdural intracranial air : an unusual cause of headache after epidural steroid injection. Anesthesiology. 1991; 74:615–618. PMID: 1825771.
7. Moradi M, Shami S, Farhadifar F, Nesseri K. Cerebral subdural hematoma following spinal anesthesia : report of two cases. Case Rep Med. 2012; 2012:352028. PMID: 22536262.
8. Nolte CH, Lehmann TN. Postpartum headache resulting from bilateral chronic subdural hematoma after dural puncture. Am J Emerg Med. 2004; 22:241–242. PMID: 15138975.

9. Ozdemir O, Calisaneller T, Yildirim E, Altinors N. Acute intracranial subdural hematoma after epidural steroid injection : a case report. J Manipulative Physiol Ther. 2007; 30:536–538. PMID: 17870423.

10. Reitman CA, Watters W 3rd. Subdural hematoma after cervical epidural steroid injection. Spine (Phila Pa 1976). 2002; 27:E174–E176. PMID: 11884923.

Fig. 1
Cervical MRI, fluoroscpic imaging and brain CT findings (performed in the pain clinic). A : Sagittal T2-weighted MRI of the cervical spine showed left foraminal space narrowing of C5-6 (arrowhead). B : Axial T2-weighted MRI of the cervical spine revealed C5-6 disc herniation with exiting C6 nerve root compression (arrowhead). C : C6 epidural steroid injection using fluoroscope was performed.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download