Abstract
Objective
A cost comparison of the surgical clipping and endovascular coiling of unruptured intracranial aneurysms (UIAs), and the identification of the principal cost determinants of these treatments.
Methods
This study conducted a retrospective review of data from a series of patients who underwent surgical clipping or endovascular coiling of UIAs between January 2011 and May 2014. The medical records, radiological data, and hospital cost data were all examined.
Results
When comparing the total hospital costs for surgical clipping of a single UIA (n=188) and endovascular coiling of a single UIA (n=188), surgical treatment [mean±standard deviation (SD) : ₩8,280,000±1,490,000] resulted in significantly lower total hospital costs than endovascular treatment (mean±SD : ₩11,700,000±3,050,000, p<0.001). In a multi regression analysis, the factors significantly associated with the total hospital costs for endovascular treatment were the aneurysm diameter (p<0.001) and patient age (p=0.014). For the endovascular group, a Pearson correlation analysis revealed a strong positive correlation (r=0.77) between the aneurysm diameter and the total hospital costs, while a simple linear regression provided the equation, y (₩)=6,658,630+855,250x (mm), where y represents the total hospital costs and x is the aneurysm diameter.
Conclusion
In South Korea, the total hospital costs for the surgical clipping of UIAs were found to be lower than those for endovascular coiling when the surgical results were favorable without significant complications. Plus, a strong positive correlation was noted between an increase in the aneurysm diameter and a dramatic increase in the costs of endovascular coiling.
With the improvement of diagnostic imaging, the incidence of UIA diagnosis is increasing, along with the national cost containment pressures associated with treatment and management. Economic considerations are important in the cost-benefit evaluation of treatments, and influence healthcare coverage, reimbursement, and policy.
While many studies have already compared the treatment modalities for intracranial aneurysms, surgical clipping and endovascular coiling, in terms of the procedural invasiveness, clinical and functional outcomes, and durability, few studies have investigated the economic costs for such treatments23713). Plus, treatment costs show distinct disparities between countries313).During the process of informed consent for clipping or coiling, UIA patients are also concerned about the cost implications. Therefore, the authors performed a cost comparison, and investigated the principal cost determinants of UIA treatment in South Korea.
This study conducted a retrospective review of data from a series of consecutive patients who underwent surgical clipping or endovascular coiling of a UIA at the authors' institution between January 2011 and May 2014. The exclusion criteria included a recent (<1 month) subarachnoid hemorrhage caused by a concomitant aneurysm, giant aneurysm with a diameter >2.5 cm, poor preoperative neurological state affecting postoperative management, and another disease or medical condition significantly increasing the hospital costs.
The medical records were reviewed to obtain relevant clinical information, and all the radiological data were obtained using an electronic picture archiving and communication system. This study was approved by the authors' Institutional Review Board.
The treatment decision, surgical coiling versus endovascular coiling, was made primarily based on the findings of the digital subtraction angiography. Surgical treatment was favored over endovascular treatment for patients with the following findings : 1) difficult navigation of the microcatheter into the aneurysm19), 2) very small (<3 mm) aneurysm149), 3) complex and wide-neck aneurysm requiring Y or X stent-assisted coiling610), 4) aneurysm with an arterial branch incorporated into the sac58), 5) fusiform or complex aneurysmal configuration, or 6) aneurysmal compression of an adjacent cranial nerve11), as long as the patients had no problems related to surgical accessibility or comorbidity.
All the patients completed an angiographic examination, chest X-ray, and laboratory tests as a preoperative evaluation before admission, and were admitted to hospital one day before the surgical or endovascular procedure.
The operative and perioperative management procedures were uniformly applied to each UIA patient. For the patients who underwent surgical clipping, a postoperative computed tomography (CT) and CT angiography were taken on day 1 following surgery. Another CT scan was performed on the day of discharge to check for the occurrence of any subdural hygromas. The perioperative medical management included an intravenous anticonvulsant and antibiotics. For most surgical patients, the length of the hospital stay was 3-6 days. In the case of elderly patients, a longer hospital stay was usually required due to fatigue and general weakness.
Meanwhile, for the patients who underwent endovascular coiling, diffusion-weighted magnetic resonance imaging was commonly performed on day 1 following the procedure to evaluate any procedure-related thromboembolic phenomena. The perioperative medical management included antiplatelet medication. The length of the hospital stay after coiling was 3-4 days for most patients, irrespective of the patient's age.
The hospital cost data were obtained from the hospital cost accounting system. The treatment costs for each patient were calculated based on the expenses incurred during the time spent as an inpatient for aneurysm treatment, including the operative and postoperative costs. The operative costs covered the neurosurgical or endovascular procedure, anesthesia, and all the materials (e.g., aneurysm clip, endovascular coil, and other surgical supplies), while the perioperative costs included the costs for the bed occupancy in the intensive care unit and regular hospital ward, radiological imaging studies, laboratory tests, and all the medications. The costs affected by patient selection (e.g., bed occupancy in the regular hospital ward) were made uniform to the basic lowest cost. All the costs are all presented in Korean won and US dollars based on an international conversion rate of ₩1100=$1.
The statistical analyses were performed using an SPSS software package (version 18.0 for Windows; SPSS Inc., Chicago, IL, USA). Plus, Scientific Data Analysis and Graphing Software (SigmaPlot, version 10.0; Systat Software Inc., Chicago, IL, USA) was applied for the statistical linear regression analysis. An independent t-test was used for the mean comparison between the surgical and endovascular groups. The correlation between the aneurysm diameter and the total hospital costs was assessed using a Pearson correlation analysis. The results were considered significant for probability values less than 0.05.
A total of 410 patients were enrolled in this study. Surgical clipping was applied to 222 patients, where a single aneurysm was clipped in 188 patients and 2-3 multiple aneurysms were clipped in 34 patients. While most patients underwent a superciliary keyhole approach (n=180, 81.1%), the others experienced a pterional approach (n=31), interhemispheric approach (n=8), or combined pterional and interhemispheric approach (n=3). Meanwhile, endovascular coiling was applied to the remaining 188 patients with a single aneurysm.
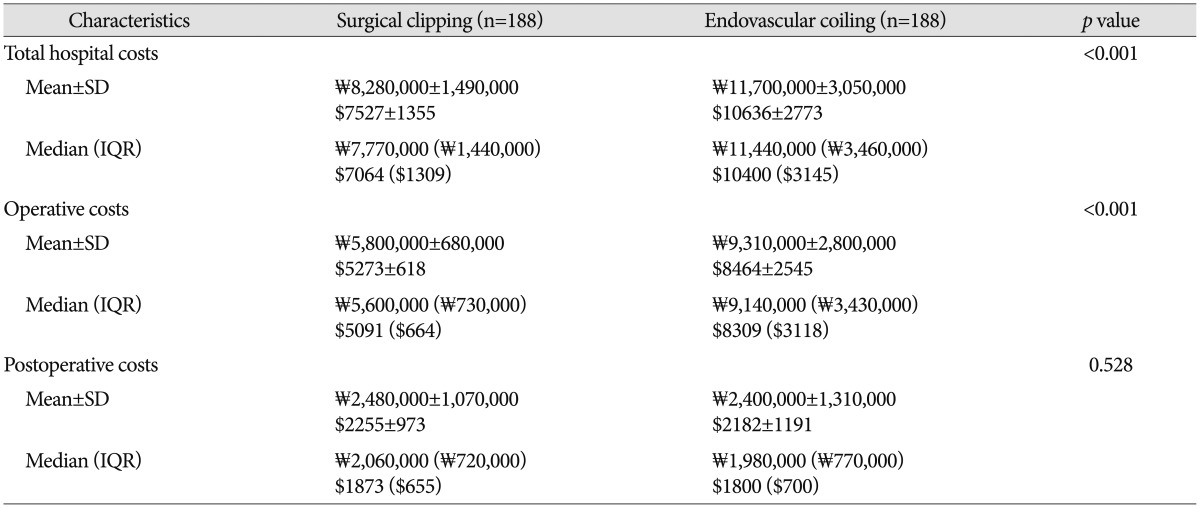
The demographic and aneurysmal characteristics of the 376 patients who underwent surgical clipping (n=188) or endovascular coiling (n=188) for a single UIA are summarized in Table 1. The ages, genders, and aneurysm locations were comparable between the surgical and endovascular groups. However, the diameters of the endovascularly-treated aneurysms were larger than those of the surgically-treated aneurysms, although the difference was small (mean±SD, range : 5.9±2.8 mm, 2.2-16.0 mm vs. 5.1±2.2 mm, 2.0-14.0 mm)
When comparing the total hospital costs for surgical clipping of a single UIA (n=188) and endovascular coiling of a single UIA (n=188), surgical treatment [mean±SD : ₩8,280,000±1,490,000 ($7527±1355)] showed significantly lower total hospital costs than endovascular treatment [mean±SD : ₩11,700,000±3,050,000 ($10636±2773), p<0.001] (Table 2). The median and interquartile range (IQR) of the total hospital costs for surgical versus endovascular treatment were ₩7,770,000 ($7064) and ₩1,440,000 ($1309) vs. 11,440,000 ($10400) and ₩3,460,000 ($3145), respectively. Thus, the median of the total hospital costs for coiling was 47% higher than that for clipping. The higher total hospital costs for endovascular treatment were due to higher operative costs, including the medical equipment and endovascular coils.
The operative costs for surgical clipping [mean±SD : ₩5,800,000±680,000 ($5273±618)] were significantly lower than the operative costs for endovascular coiling [mean±SD : ₩9,310,000±2,800,000 ($8464±2545), p<0.001]. The median and IQR of the operative costs for surgical versus endovascular treatment were ₩5,600,000 ($5091) and ₩730,000 ($664) vs. ₩9,140,000 ($8309) and ₩3,430,000 ($3118), respectively. The price of one endovascular coil was approximately ₩550,000 ($500), while the price of one surgical clip was approximately ₩140,000 ($127). In addition, endovascular treatment of a single aneurysm required a considerable increase in the number of coils according to the diameter of the aneurysm, whereas most surgical cases only required one to three aneurysm clips.
Notwithstanding, there was no statistical difference in the perioperative costs between the surgical and endovascular groups [mean±SD : ₩2,480,000±1,070,000 ($2255±973) vs. ₩2,400,000±1,310,000 ($2182±1191)].
In the multi regression analysis, the factors significantly associated with the total hospital costs for endovascular treatment of a single UIA were the aneurysm diameter (p<0.001) and patient age (p=0.014), while the patient gender and aneurysm location were not associated. In the case of surgical treatment, the only factor significantly associated with the total hospital costs was the aneurysm diameter (p<0.001), while the patient age, gender, and aneurysm location were not associated.
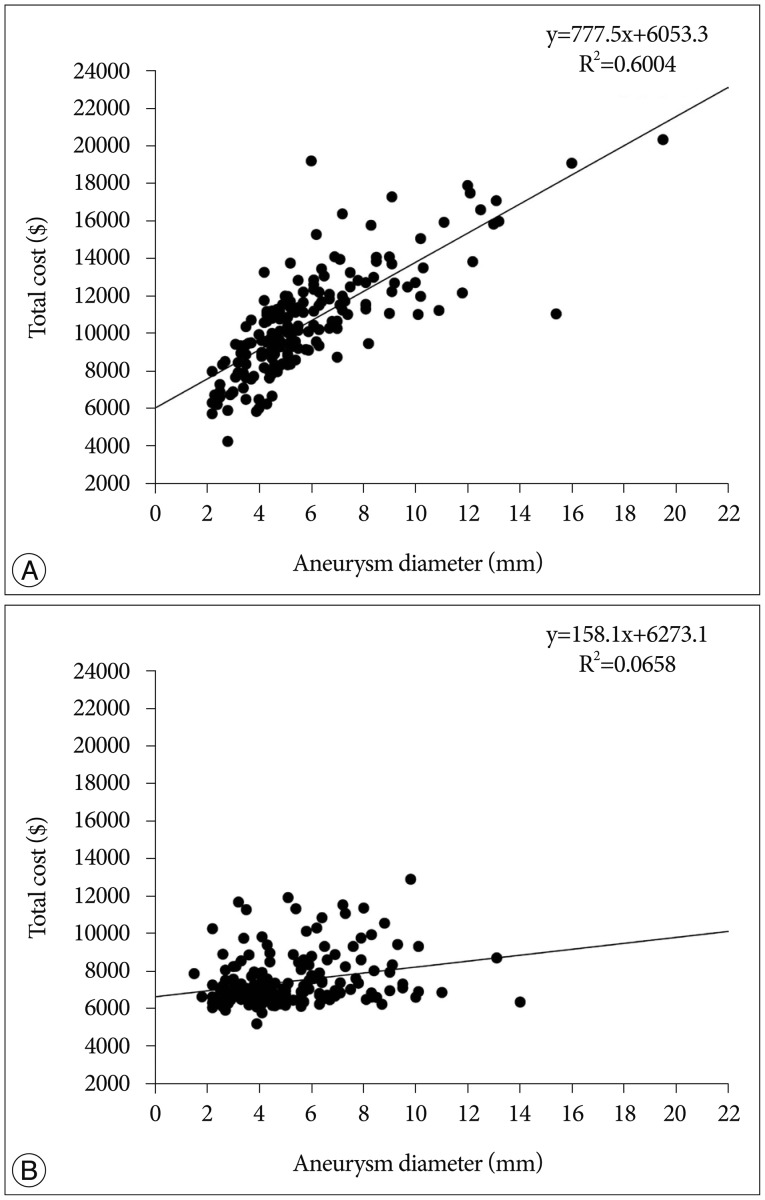
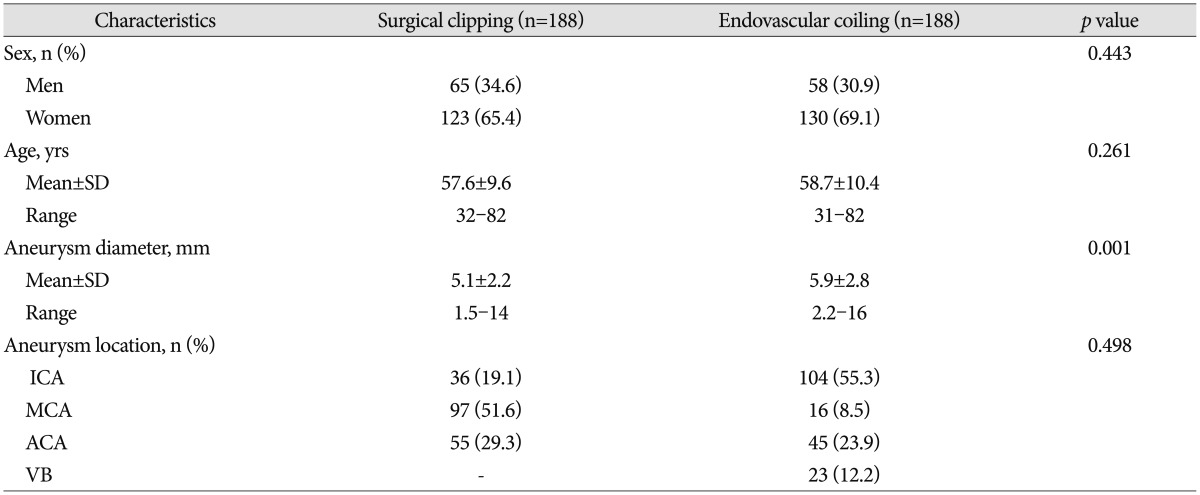
The Pearson correlation analysis of the endovascular group showed a strong positive correlation (r=0.77) between the aneurysm diameter and the total hospital costs (Fig. 1A), whereas only a weak positive correlation (r=0.16) was revealed between the patient age and the total hospital costs. Meanwhile, the Pearson correlation analysis of the surgical group showed a weak positive correlation (r=0.26) between the aneurysm diameter and the total hospital costs (Fig. 1B).
A simple linear regression analysis was used to develop an equation for predicting the dependent variable (y, total hospital costs) given a value (x, aneurysm diameter) for the independent variable. For the endovascular group, this equation was y (₩)= 6,658,630+855,250x (mm) or y ($)=6053.3+777.5x (mm). The value of R2 was 0.6004.
Thirty four patients were surgically treated for two (n=27) or three (n=7) UIAs during a single operation, however, no patient received endovascular treatment for multiple UIAs during a single session. The mean value of the total hospital costs for the surgical treatment of two UIAs was ₩10,810,000±2,960,000 ($9827±2691), while the mean value for the surgical treatment of three UIAs was ₩11,540,000±1,430,000 ($10491±1300).
For both treatment groups, no direct mortality or permanent morbidity adversely affecting the Glasgow Outcome Scale ensued from the treatments. Two patients in the surgical group developed venous infarction and transient somnolence after clipping a pericallosal artery aneurysm, yet both patients recovered without neurological deficits. Meanwhile, a patient in the endovascular group developed a thromboembolism and transient leg monoparesis after coiling an anterior communicating artery aneurysm.
Previous cost comparisons of surgical clipping and endovascular coiling of intracranial aneurysms have revealed distinct disparities between different countries. The International Subarachnoid Aneurysm Trial (ISAT), primarily conducted in Europe, showed no significant cost difference between surgical and endovascular groups at a 1-year or 2-year follow-up13). While the endovascular patients had higher costs related to the initial intervention and subsequent procedures due to recurrences, this was offset by lower costs related to the shorter hospital stay and fewer complications. However, a national analysis using a Nationwide Inpatient Sample in the United States showed significantly higher total hospital costs for surgical clipping of both ruptured and unruptured aneurysms when compared with endovascular coiling3). In contrast, the present study showed significantly lower costs for surgical clipping of UIAs, attributable to the lower device cost of clips over coils and good surgical results with minimal complications.
In the present surgical case series, the advantage of lower economic costs was also enhanced by the reduced surgical invasiveness of a keyhole approach used on 81% of the patients. Radovanovic et al.12) previously reported that minimally invasive surgery reduced hospital costs by decreasing the operative time and length of the hospital stay when compared with conventional surgery. However, in the present study, the impact of minimally invasive surgery on the treatment costs was not critical, as postoperative costs including hospital bed charges are not high in South Korea.
Since the total hospital costs associated with endovascular coiling of a UIA varied predictably as a function of the aneurysm diameter, the costs for endovascular coiling of a UIA can be estimated before the procedure using the suggested equation provided by a simple linear regression analysis, where R2 is a statistical measure of the closeness of the data to the fitted regression line. Thus, when the value of R2 is 0.6, 60% of the data is on the straight line.
The current study has several limitations. First, it is based on a retrospective review of a case series from a single institution. As the surgical techniques and results affecting treatment costs can vary significantly between medical institutions, it is difficult to make generalizations. Second, it does not include any long-term economic impact related to the surgical and endovascular treatment of UIAs. For example, the number of postoperative angiograms, outpatient services, and retreatments can be higher in the case of endovascular treatment.
In South Korea, the surgical clipping of UIAs was found to incur lower total hospital costs than endovascular coiling when the surgical results were favorable without significant complications. Plus, a strong positive correlation was noted between an increase in the aneurysm diameter and a dramatic increase in the costs of endovascular coiling.
References
1. Birknes JK, Hwang SK, Pandey AS, Cockroft K, Dyer AM, Benitez RP, et al. Feasibility and limitations of endovascular coil embolization of anterior communicating artery aneurysms : morphological considerations. Neurosurgery. 2006; 59:43–52. discussion 43-52PMID: 16823299.

2. Hoh BL, Chi YY, Dermott MA, Lipori PJ, Lewis SB. The effect of coiling versus clipping of ruptured and unruptured cerebral aneurysms on length of stay, hospital cost, hospital reimbursement, and surgeon reimbursement at the university of Florida. Neurosurgery. 2009; 64:614–619. discussion 619-621PMID: 19197221.

3. Hoh BL, Chi YY, Lawson MF, Mocco J, Barker FG 2nd. Length of stay and total hospital charges of clipping versus coiling for ruptured and unruptured adult cerebral aneurysms in the Nationwide Inpatient Sample database 2002 to 2006. Stroke. 2010; 41:337–342. PMID: 20044522.

4. Ioannidis I, Lalloo S, Corkill R, Kuker W, Byrne JV. Endovascular treatment of very small intracranial aneurysms. J Neurosurg. 2010; 112:551–556. PMID: 19715422.

5. Kim BM, Park SI, Kim DJ, Kim DI, Suh SH, Kwon TH, et al. Endovascular coil embolization of aneurysms with a branch incorporated into the sac. AJNR Am J Neuroradiol. 2010; 31:145–151. PMID: 19749218.

6. Koebbe CJ, Veznedaroglu E, Jabbour P, Rosenwasser RH. Endovascular management of intracranial aneurysms : current experience and future advances. Neurosurgery. 2006; 59(5 Suppl 3):S93–S102. discussion S3-S13PMID: 17053622.
7. Lad SP, Babu R, Rhee MS, Franklin RL, Ugiliweneza B, Hodes J, et al. Long-term economic impact of coiling vs clipping for unruptured intracranial aneurysms. Neurosurgery. 2013; 72:1000–1011. discussion 1011-1013PMID: 23612602.

8. Lubicz B, Lefranc F, Levivier M, Dewitte O, Pirotte B, Brotchi J, et al. Endovascular treatment of intracranial aneurysms with a branch arising from the sac. AJNR Am J Neuroradiol. 2006; 27:142–147. PMID: 16418374.
9. Moret J, Pierot L, Boulin A, Castaings L, Rey A. Endovascular treatment of anterior communicating artery aneurysms using Guglielmi detachable coils. Neuroradiology. 1996; 38:800–805. PMID: 8957810.

10. Murayama Y, Nien YL, Duckwiler G, Gobin YP, Jahan R, Frazee J, et al. Guglielmi detachable coil embolization of cerebral aneurysms : 11 years' experience. J Neurosurg. 2003; 98:959–966. PMID: 12744354.

11. Park J, Kang DH, Chun BY. Superciliary keyhole surgery for unruptured posterior communicating artery aneurysms with oculomotor nerve palsy : maximizing symptomatic resolution and minimizing surgical invasiveness. J Neurosurg. 2011; 115:700–706. PMID: 21699478.

12. Radovanovic I, Abou-Hamden A, Bacigaluppi S, Tymianski M. A safety, length of stay, and cost analysis of minimally invasive microsurgery for anterior circulation aneurysms. Acta Neurochir (Wien). 2014; 156:493–503. PMID: 24395051.

13. Wolstenholme J, Rivero-Arias O, Gray A, Molyneux AJ, Kerr RS, Yarnold JA, et al. Treatment pathways, resource use, and costs of endovascular coiling versus surgical clipping after aSAH. Stroke. 2008; 39:111–119. PMID: 18048858.

Fig. 1
Graph showing Pearson correlation analysis results between aneurysm diameter and total hospital costs. A : Endovascular group showing strong positive correlation (r=0.77). B : Surgical group showing weak positive correlation (r=0.26).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download