Abstract
Cervical epidural steroid injection is indicated for radicular symptoms with or without axial neck pain. Complications are rare but can be serious. Here, we report the case of a 54-year-old man with cervical radicular pain who was treated with cervical epidural steroid injection. Injection was administered twice under fluoroscopic guidance with the loss-of-resistance technique using air to confirm the epidural space. After the second procedure, the patient complained of severe persistent headache and was diagnosed with pneumocephalus on brain computed tomography. The patient returned home without any neurological complication, after a few days of conservative treatment. Though, a fluoroscopic guidance cervical epidural injection is also known to diminish the risk of complications. Physicians should always keep in mind that it does not guarantee safety, particularly in the cervical region, related to its anatomical considerations.
Cervical epidural steroid injection (CESI) is frequently used in the treatment of cervical radicular pain and neck pain. Complications are rare, but significant events can occur, particularly in the cervical region. Here, to contribute to the understanding of complications, we report a case of pneumocephalus after CESI that occurred despite administering the injection under fluoroscopy guidance-considered to improve safety. Written informed consent to publish this case was obtained from the patient.
A 54-year-old man with a history of cervical radiculopathy visited our clinic. He complained of neck pain and radicular symptoms involving the left arm, which had started 20 days previously when lifting heavy luggage. History included medication for the past 10 years for gout, but he was otherwise healthy. Radiography of the cervical spine revealed narrowing of the C6-7 intervertebral space. The nonsteroidal anti-inflammatory drug medication had had no effect on his pain, so CESI was selected as treatment. The patient was placed in the prone position with arms at the side. The needle was advanced via the interlaminar approach at the level of C7-T1 after ensuring correct positioning of the needle by checking in a lateral or contralateral oblique view as a "safety view" to ensure appropriate depth. The epidural space was finally located using the loss-of-resistance (LOR) technique with 1.0 mL of air. In addition, positioning in the epidural space was reconfirmed on the AP and lateral planes on fluoroscopy after injection of 2 mL of contrast medium. A mixture composed of 10-mg dexamethasone, 2-mL mepivacaine 0.5%, and normal saline up to a total volume of 6 mL was injected through a 21-gauge Tuhoy needle. The procedure was repeated twice with a 1-week interval. The first injection was effective for relief of radicular pain, resulting in a reduction of 40% on a visual analogue scale, so the patient agreed to continue treatment. Second procedure went in a same manner with first. However, 4 h after completion of the second procedure, the patient experienced sudden onset of a severe thunderclap-like headache. The headache was aggravated by coughing or sneezing and accompanied by severe dizziness, and was not relieved by changes in position, like lying down.
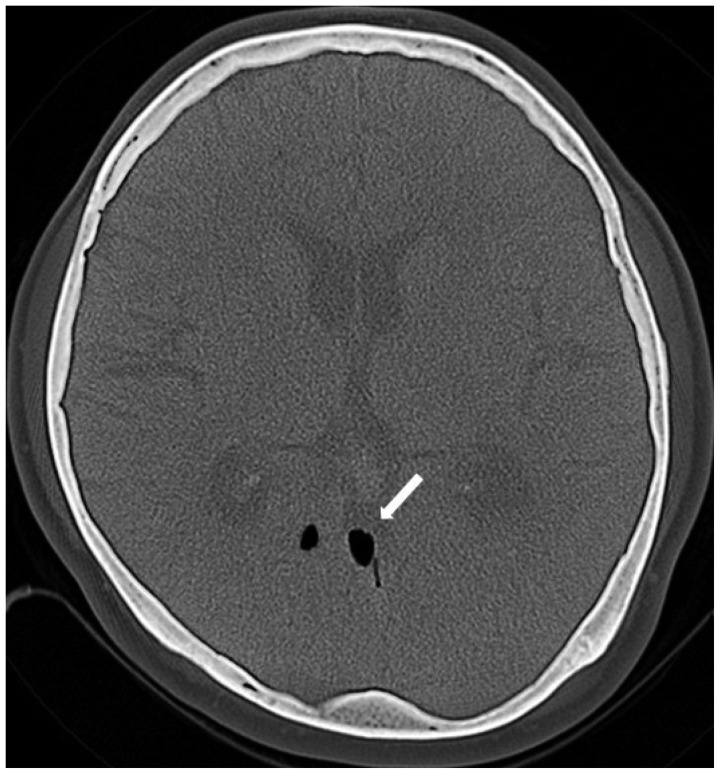
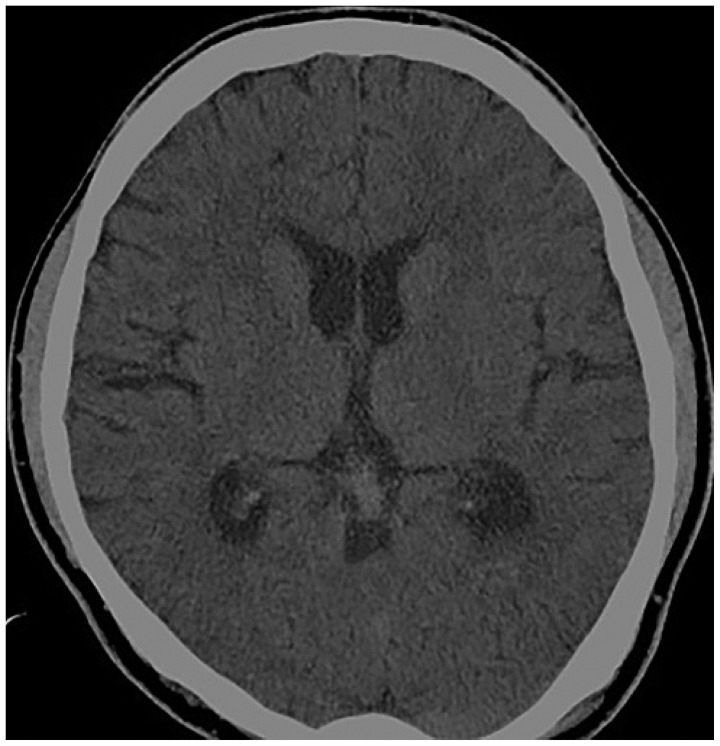
The patient demonstrated stable vital signs. Opioids were administered but failed to relieve symptoms. The headache persisted all day, and the patient was transferred to the department of neurology the next day. Findings on neurologic examination were normal but, because of the unremitting headache, brain computed tomography (CT) was performed. Brain CT revealed air in the subarachnoid space, around the basal cisterns (Fig. 1). With a suspicious diagnosis of pneumocephalus as the cause of his headache, the patient was treated with conservative management including analgesics and 100% of oxygen. Over the next 16 days, the headache and dizziness resolved completely, showing non-specific findings on follow-up brain CT (Fig. 2) and the patient was discharged. The patient experienced no neurologic sequelae from pneumocephalus, and the radicular pain resolved within the next 3 weeks.
CESI has been used in the management of chronic persistent neck pain with or without upper extremity pain11). Injections in the cervical spine are performed using either interlaminar or transforaminal approaches. Complications reported with interlaminar CESI include dural puncture, infections, bloating, nausea and vomiting, vasovagal reaction, facial flushing, fever, nerve root injury, spinal cord injury, pneumocephalus, epidural hematoma, subarachnoid hemorrhage (SAH), and stiff neck2). Complications with this procedure are relatively rare, with an overall rate of 0.25-0.5%12). Headache occurring after the procedure may indicate postdural puncture headache (PDPH), SAH, migraine, or pneumocephalus. Careful history taking and review of the technique can help differentiate the cause of the symptoms. A migraine is often recurrent and similar to other headaches. SAH is extremely rare with high mortality. PDPH usually presents as a headache that is position related, and can be relieved by lying down, with a relatively long onset time of 24-48 h after the procedure. Detection of cerebrospinal fluid following inadvertent dura puncture also supports a diagnosis of PDPH. Pneumocephalus can be caused by air entering the meninges during the process of finding the epidural space. Therefore, pneumocephalus should be considered when an LOR technique with air is used. In contrast to PDPH, onset time of the headache is generally immediate and the symptoms do not improve with positional change. However, as it was in our case, pneumocephalus-related headache can occur up to 4 h after CESI-a somewhat delayed onset time. Although the clinical results are usually fair7) with conservative treatment including 100% oxygen, adequate monitoring is essential to detect secondary complications, such as unconsciousness, apnea, and hypotension,4) which may lead to fatal consequences such as hypoxic damage or death if not treated promptly. A brain CT scan is a useful diagnostic tool to confirm the condition.
Although pneumocephalus is a possible complication with epidural steroid injection, most of the cases that have been reported to date were procedures involving the lumbar region. We could find only two reports in the literature on pneumocephalus after epidural injection in the cervical region89). A safe volume of air with the LOR technique has not been established. The volume of air used in the lumbar region ranged from 2 to 20 mL in previous reports57). However, less than 2 mL of subarachnoid air in the lumbar region has been associated with headache6). These previous reports only considered the lumbar region. It is reasonable to hypothesize that the risk of pneumocephalus is higher in the cervical than lumbar region, even with a smaller volume of air, because of the proximity to the brain. Compared with the previous report on pneumocephalus after CESI with 2 mL of air8), it appears that a volume of air as small as 1.0 mL (used in our case) can cause pneumocephalus after epidural injection in the cervical region.
Various reports have considered anatomical and methodological factors affecting safe implementation of epidural injection. The potential for pneumocephalus is said to be reduced by using normal saline with the LOR technique3). However, this method is controversial for identification of the epidural space. Placement of the needle into epidural blood vessels or interspinous ligament can give rise to false-positive results, particularly with the blind technique used in a previous report7). Various anatomical characteristics of the cervical region need to be considered during epidural injection. 1) The ligamentum flavum at the cervical level is thin, making loss of resistance subtle. 2) The possibility of a false loss of resistance between the interspinous ligament and ligamentum flavum is increased in the cervical region. 3) Compared with the lumbar region, the distance between the ligamentum flavum and dura is small, and a smaller epidural space results in closer proximity of the spinal cord; thus, although complications are rare, they may be serious, even by a small margin of error. In our case, we assume that small air used in the loss-of-resistance technique for confirming epidural space was the cause of the pneumocephalus related to anatomical features in cervical region described above.
In consideration of these factors, it is recommended to use fluoroscopy rather than the blind technique to reduce the risk of complications10). Epidurography, involving the use of contrast medium with fluoroscopic guidance helps differentiate between the epidural and subdural spaces and to confirm that the needle has not entered an epidural vessel. However, operators must be mindful that fluoroscopy does not always guarantee the patient's safety, even when performed by expert physicians. A noteworthy anatomical investigation of the cervical epidural space in cadavers highlights the frequency of mid-line gaps in the ligamentum flavum at the cervical and upper-thoracic levels5). In this study, the frequency of mid-line gaps was 64% at C6-7 and 51% at C7-T1. Thus, mid-line gaps are relatively common in the cervical region, and, from a clinical perspective, physicians cannot depend on the ligamentum flavum as a perceptible safety barrier for epidural needle placement at these levels; this is of particular importance because C6-7 is one of the most common level where CESI is performed . On the other hand, the LOR technique can give rise to false-positive results, particularly with the fluoroscopy-guided interlaminar approach, which emphasizes an exact midline approach12). Taken together, these factors indicate that safety may be improved by inserting the epidural needle slightly to the lateral side while observing the lateral facet line on an anteroposterior fluoroscopy view.
In conclusion, pneumocephalus is a rare complication with CESI, but has a significant risk of headache and neurologic complications even with a small amount of air. To reduce the risk, the patient must remain immobile, the needle must be stabilized, and care should be taken during the attachment of extension tubing after aspiration to ensure that the air has been aspirated into the barrel of the syringe. Fluoroscopic guidance with AP and lateral view during the procedure is also known to diminish the risk, but physicians should always keep in mind that it does not guarantee safety, particularly in the cervical region.
References
1. Derby R, Lee SH, Kim BJ, Chen Y, Seo KS. Complications following cervical epidural steroid injections by expert interventionalists in 2003. Pain Physician. 2004; 7:445–449. PMID: 16858486.
2. Huston CW. Cervical epidural steroid injections in the management of cervical radiculitis : interlaminar versus transforaminal. A review. Curr Rev Musculoskelet Med. 2009; 2:30–42. PMID: 19468916.

3. Kawamata T, Omote K, Matsumoto M, Toriyabe M, Ito T, Namiki A. Pneumocephalus following an epidural blood patch. Acta Anaesthesiol Scand. 2003; 47:907–909. PMID: 12859316.

4. Kim YD, Lee JH, Cheong YK. Pneumocephalus in a patient with no cerebrospinal fluid leakage after lumbar epidural block -a case report-. Korean J Pain. 2012; 25:262–266. PMID: 23091688.

5. Lirk P, Kolbitsch C, Putz G, Colvin J, Colvin HP, Lorenz I, et al. Cervical and high thoracic ligamentum flavum frequently fails to fuse in the midline. Anesthesiology. 2003; 99:1387–1390. PMID: 14639154.

6. Roderick L, Moore DC, Artru AA. Pneumocephalus with headache during spinal anesthesia. Anesthesiology. 1985; 62:690–692. PMID: 3994045.

7. Saberski LR, Kondamuri S, Osinubi OY. Identification of the epidural space : is loss of resistance to air a safe technique? A review of the complications related to the use of air. Reg Anesth. 1997; 22:3–15. PMID: 9010941.

8. Simopoulos T, Peeters-Asdourian C. Pneumocephalus after cervical epidural steroid injection. Anesth Analg. 2001; 92:1576–1577. PMID: 11375849.

9. Stauber B, Ma L, Nazari R. Cardiopulmonary arrest following cervical epidural injection. Pain Physician. 2012; 15:147–152. PMID: 22430652.
10. Stojanovic MP, Vu TN, Caneris O, Slezak J, Cohen SP, Sang CN. The role of fluoroscopy in cervical epidural steroid injections : an analysis of contrast
dispersal patterns. Spine (Phila Pa 1976). 2002; 27:509–514. PMID: 11880836.
11. Van Zundert J, Harney D, Joosten EA, Durieux ME, Patijn J, Prins MH, et al. The role of the dorsal root ganglion in cervical radicular pain : diagnosis, pathophysiology, and rationale for treatment. Reg Anesth Pain Med. 2006; 31:152–167. PMID: 16543102.
12. Waldman SD. Atlas of Interventional Pain Management, ed 3. Philadelphia: Saunders/Elsevier;2009. p. 170.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download