Abstract
Objective
With the increased use of interspinous spacers in the treatment of lumbar stenosis, knowledge of the geometry of the interspinous space is important. To prevent dislodgment of an interspinous spacer, the accurate depth and width of the interspinous space needs to be established to facilitate the best intraoperative selection of correct spacer size.
Methods
To determine the depth and width of the interspinous space, two methods are available which utilize plain film and magnetic resonance imaging (MRI). Data analysis of the interspinous depth and width was undertaken in 100 patients.
Results
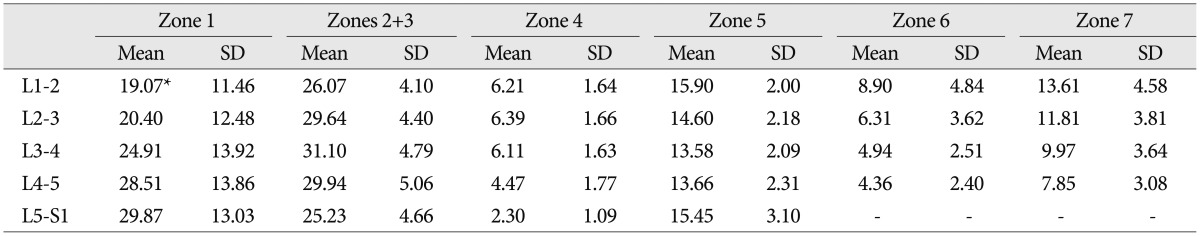
The standard deviations were variable, since skin thickness (zone 1) was altered by sex and age. The difference in the zone 1 distance between adjacent interspinous processes varied according to gender (p<0.05), but was not influenced by age [p=0.32 by analysis of variance between groups (ANOVA)]. Zone 2, the supraspinous, and zone 3, the interspinous ligament depths, comprise the operative working area during insertion of an interspinous spacer. There were no differences with regard to gender or age (p>0.05). For zones 6 and 7, the interspinous distances at the narrowest and widest points, respectively, were found to decrease with the aging process, but the decrease was not statistically significant. There were no differences with regard to gender (p>0.05).
The cause of sagittal plane spinal instability in the lumbar spine is related to degeneration of the intervertebral disc, with its disruption of fibrous structure of the annulus fibrosis3), reduction in disc height, and consequent laxity of the intervertebral ligaments.
A useful alternative would be stabilization of the painful lumbar segment in the sagittal plane with the allowance of some spinal mobility.
A number of clinical trials utilizing posterior dynamic stabilization devices for lumbar spinal disease have been carried out, many with differing biomechanical principles as their bases. Lumbar interspinous distraction implants used for dynamic stabilization.
There has been an increased interest in the use of an interspinous spacer to treat lumbar stenosis : the design and insertion of which requires the spatial characteristics of the interspinous space. Anatomists, spinal surgeons and biomechanical engineers therefore require comprehensive and representative data concerning the geometry of the interspinous space.
The need for quantitative data regarding the function of the vertebral column has been expressed in numerous studies6,14). Simulation models have been used in many mathematical and biomechanical studies to predict the mechanical responses of the vertebral body/disc segment and the vertebral column as a whole, under various dynamic conditions10). The anthropometric dimensions of the vertebral and intervertebral disc parameters have been presented and thoroughly discussed by Nissan and Gilad6,7). However, no data are available on the dimensions of the interspinous space. The design and insertion of an interspinous spacer requires an accurate understanding of the depth and width of the interspinous space, so as to prevent a change in lordosis and dislodgment of this spacer. These measurements need to be established.
A total of 100 Stanford University Medical Center (SUMC) subjects between the ages of 19 to 84 years of age were evaluated. The subjects' medical files were reviewed and to be included in this study, the patients must have been without indications of known spinal disease or congenital spinal deformation. All plain films were taken using the same X-ray machine (Phillips-Medic DLX, Amsterdam, The Netherlands) and the same type of film plates were utilized (Agfa-Gevaret CURIX RPI, Nordrhein-Westfalen, Leverkusen, Germany). Frames of 14×14 cm were used for the lumbar spine X-ray. For lateral lumbar spine radiography, the subject was placed on his or her side with knees positioned in slight flexion, and the upper extremities placed outside of the photographed area. The distance between the X-ray tube and the film plate was 100 cm. The machine was calibrated at 89-95 kV, and the tube was focused on the center of the L3 vertebral body.
An MRI was performed in all patients (1.5 T, Signa Horizon; GE Medical System, Milwaukee, WI, USA) and axial and sagittal T2-weighted images were evaluated. The T2-weighted sequence had the following characteristics : the TR/TE was 3000/114, the matrix was 256×256, the thickness of each section was four mm and the field of view was 30 cm.
The lateral lumbar plain films and midsagittal magnetic resonance imagines (MRIs) of patients were used to determine the depth and width of the interspinous space. Only films of patients without evidence of degeneration or irregularities of the intervertebral disc were used.
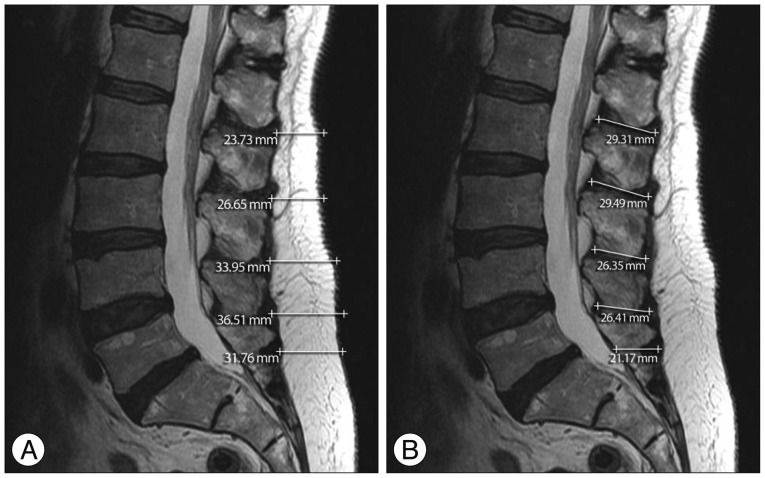
The geometric configuration of the interspinous space in the sagittal view was measured using straight lines between the skin and seven parameters, i.e., the zones 1-7 (Fig. 1). Lateral views of either MRIs or plain films were used to determine the seven parameters as follows : T2-weighted midline sagittal MRIs defined zones 1, i.e., skin thickness, 2, the supraspinous ligament depth, and 3, which was the interspinous ligament depth (Fig. 2). Axial T2-weighted MRIs were measured to determine the values for zones 4, the distance from the dural sheath to the surface of the ligamentum flavum and 5, the width of the thecal sac (Fig. 3). Plain films were used to evaluate zone 6 which represented the interspinous distance at its narrowest point and zone 7, the interspinous distance at its widest point (Fig. 4).
Five parameters were measured on the T2-weighted midsagittal MR images. Using three-fold magnification, these five parameters were calculated with a digital cursor available in the Centricity PACS Version 2.0 (GE Healthcare, Milwaukee, WI, USA). The interspinous process distances were determined at the narrowest and at the widest points between the adjacent projections of the spinous process. All measurements were repeated three times.
The intra-observer variability was avoided by measuring the above data once each week times three weeks total.
Multivariate ANOVA was used to evaluate the influence of age or gender on the recorded differences. If there was an effect, the divergent levels were identified by the univariate F-test. The deviations at these levels were verified in a one-way ANOVA with a post-hoc test (Bonferroni) to account for multiple comparisons. All calculations were done using SPSS 11.0 (SPSS Inc., Chicago, IL, USA) (p<0.05).
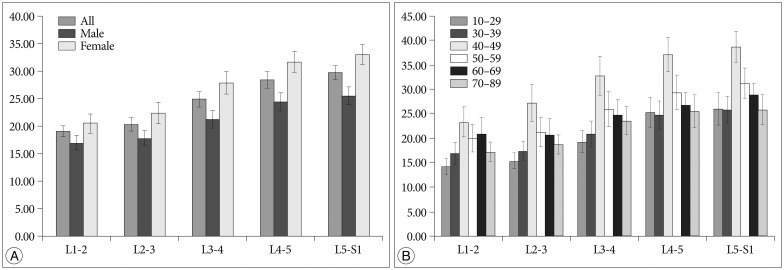
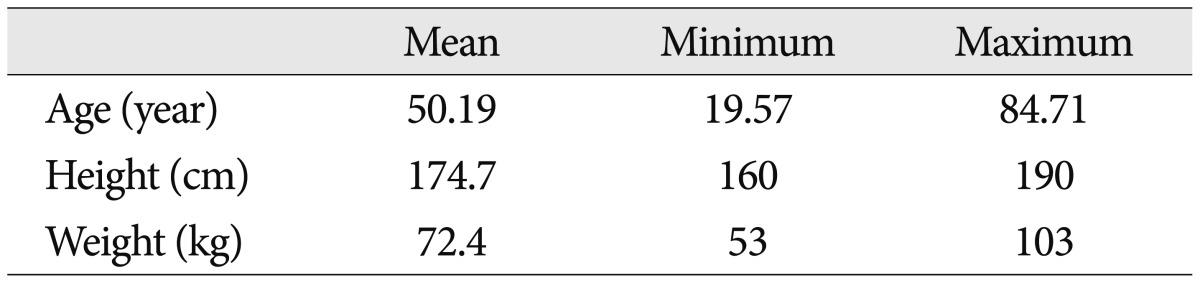
Table 1 presents the physical characteristics of all patients. The sex ratio was 1:1.22 (male:female). Table 2 shows the overall results of the morphometric evaluation of the lumbar interspinous spaces. It was shown in this study that the mean value of the skin depth was 19.06 mm at L1-2, 20.40 mm at L2-3, 24.91 mm at L3-4, 28.51 mm at L4-5 and 29.87 mm at L5-S1. Zone 1, the skin thickness, depended on gender (p<0.05) and was influenced by age, but the latter values were not statistically significant (p=0.32; multivariate ANOVA) (Fig. 5). The skin thickness, or zone 1, tended to be greatest between 40 and 49 years of age (Fig. 5).
Zones 2 and 3 represented the main operative working space used during insertion of an interspinous spacer. Differentiation between zone 2 and zone 3 was difficult, however, therefore, zones 2 and 3 were combined into one measurement (zone 2+zone 3). Zone 2+zone 3 was 26.07 mm at L1-2, 29.64 mm at L2-3, 31.10 mm at L3-4, 29.94 mm at L4-5, and 25.23 mm at L5-S1.
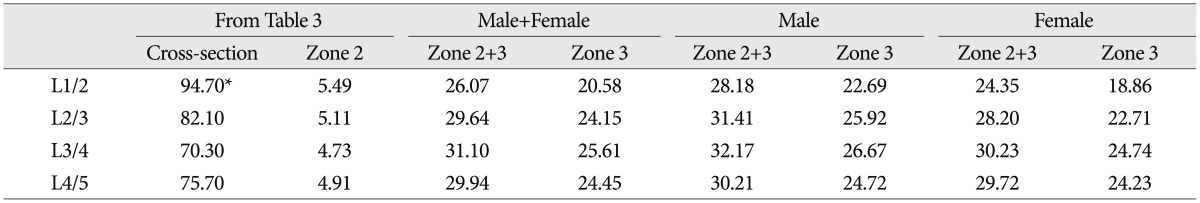
The working area for use of surgical instruments during interspinous spacer insertion was represented by zone 3. In this study, the separation between zone 2 and zone 3 was not well-delineated on sagittal MRI and thus differentiation between these two zones was difficult to evaluate using this modality. Zones 2 and 3 were merged into one value for this reason. The midline attachments of the posterior layer of the thoracolumbar fascia and the longissimus thoracis and multifidus muscles form the principal connective tissue component of both the supraspinous and interspinous ligaments in the lumbar spine9). Any attempt to separate these two ligaments, since they both originate from the same connective tissues, is thus purely arbitrary. There are a few papers regarding the measurement of the lumbar spinal ligaments. Table 3 shows the lengths and cross-sectional areas of the supraspinous and interspinous ligaments from another author's study8).
Thus, the mean value of zones 2+3 were 26.07 mm at L1-2, 29.64 mm at L2-3, 31.10 mm at L3-4, 29.94 mm at L4-5, and 25.23 mm at L5-S1 in our study. Zone 3 is important because it is the actual working area used during placement of an interspinous spacer. We consider only a circular portion of the supraspinous ligament and this area is known as the article (πr2=cross-sectional area in mm2)8). We calculated the thickness of sup-raspinous ligament (2r=zone 2). After calculating, zone 3 was 20.58 mm at L1-2, 24.15 mm at L2-3, 25.61 mm at L3-4, and 24.45 mm at L4-5 (Table 3).
Zone 4 was 6.21 mm at L1-2, 6.39 mm at L2-3, 6.11 mm at L3-4, 4.47 mm at L4-5, and 2.30 mm at L5-S1. Zone 5 was 15.90 mm at L1-2, 14.60 mm at L2-3, 13.58 mm at L3-4, 13.66 mm at L4-5, and 15.45 mm at L5-S1. Zones 4 and 5 were not influenced by age and gender. The thickness of zone 4 is important for placement of interspinous spacers due to the necessity of dural sac protection during insertion.
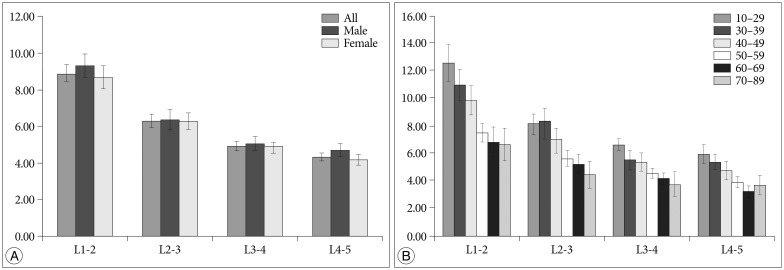
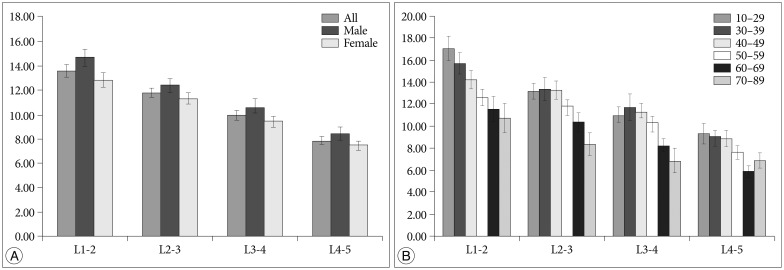
Zone 6 was 8.90 mm at L1-2, 6.32 mm at L2-3 and 4.9 mm at L3-4, and 4.36 mm at L4-5. Zone 7 was 13.61 mm at L1-2, 11.81 mm at L2-3, 9.97 mm at L3-4, and 7.85 mm at L4-5. Zones 6 and 7 were decreased by the aging process as seen in Fig. 6, 7. But no differences in age to a statistically-significant degree (p>0.05). Zone 6 is also important because it is the entry point for most interspinous spacer placement procedures. Zone 7 is the actual operative working area.
There is limited published morphometric data on the interspinous space. Neumann et al.5) discusses the interspinous distance between spinous processes in the spine. In our investigation, the interspinous regions relative to the orientation of interspinous spacer placement were defined. These regions were calculated by the use of anatomic data taken from plain films and MRI of the lumbar spine. The data can prove helpful in the performance of conventional operative procedures and are essential for interspinous implant design, modeling, and workspace definition with regard to an interspinous spacer.
The measurement error of radiographic variables stems from several causes, notably poor definition of anatomic measuring points, changes in patient position, and intra- and interobserver variations1,9). Thus, measurements of these variables should be accurate, so as to enable comparisons between radiographs from repeated examinations.
Regarding radiographical measurements, there were marked differences between observers in other studies, as well. The data presented in the findings of Pope et al.9), Anderson et al.1) and Hayes et al.3) showed that the quantitative assessment of disc height is unreliable by X-ray. Taken together, these circumstances warrant the conclusion that comparisons based on numerical measurements of the disc height by X-ray should only be made with caution.
This is in contrast to the results of repeated measurements, which showed complete interobserver correspondence. Thus, for X-ray measurements, this semiquantiative method is recommended. A limitation of our study is that the measurements were carried out three times by only one observer rather than by multiple observers.
Skin depth differs according to sex and age. Thus, in this study, the results of skin depth measurements, i.e., zone 1, were divided into the two groups of sex and age. Lumber female skin was found to be thicker than in the male (p<0.05) in our study. Zone 1 increased until the age of 40-49 years, after which it decreased (Fig. 5). No statistically-significant differences (p>0.05) were found. The skin depth (zone 1) values varied greatly. When the interspinous spacers are placed at our institution, the skin depth is measured by midsagittal MRI films or the procedure is performed using C-arm guidance. We would like to develop minimal invasive operation technique. So skin thickness is important because of depth of operation instrument.
The preservation of the supraspinous ligament is crucial for interspinous spacer insertion because the supraspinous ligament affords more support than if it were cut, from a biomechanical standpoint. Zone 4 is vital for interspinous spacer insertion because damage to the cauda equina must be avoided. We consider zone 6 as the entry point in the interspinous spacer procedure. Zone 7 is regarded as the real working area. In this study, the distance of zone 3, i.e., real working space, zone 6, i.e., entry point, and zone 7, i.e., real working space, were most important in the placement of the interspinous spacer.
The three limitation of this study were remained. In the first, population of these data is not separated by ages and races. So these data were small size. Second was zone 2 and 3 were not separated because of limitation of MRI imaging. Even if, preservation of the supraspinous ligament is crucial for interspinous spacer insertion because the supraspinous ligament affords more support than if it were cut, from a biomechanical standpoint. In the third, there were no data about dynamic factor, for example differences between flexion and extension.
Acknowledgements
We thank Woong Yoon, M.D., for his assistance in the preparation of the manuscript.
References
1. Andersson GB, Schultz A, Nathan A, Irstam L. Roentgenographic measurement of lumbar intervertebral disc height. Spine (Phila Pa 1976). 1981; 6:154–158. PMID: 7280816.

2. Gilad I, Nissan M. A study of vertebra and disc geometric relations of the human cervical and lumbar spine. Spine (Phila Pa 1976). 1986; 11:154–157. PMID: 3704802.

3. Hayes MA, Howard TC, Gruel CR, Kopta JA. Roentgenographic evaluation of lumbar spine flexion-extension in asymptomatic individuals. Spine (Phila Pa 1976). 1989; 14:327–331. PMID: 2711247.

4. Johnson GM, Zhang M. Regional differences within the human supraspinous and interspinous ligaments : a sheet plastination study. Eur Spine J. 2002; 11:382–388. PMID: 12194001.

5. Neumann P, Wang Y, Kärrholm J, Malchau H, Nordwall A. Determination of inter-spinous process distance in the lumbar spine. Evaluation of reference population to facilitate detection of severe trauma. Eur Spine J. 1999; 8:272–278. PMID: 10483828.
6. Nissan M, Gilad I. Dimensions of human lumbar vertebrae in the sagittal plane. J Biomech. 1986; 19:753–758. PMID: 3793749.

7. Nissan M, Gilad I. The cervical and lumbar vertebrae-an anthropometric model. Eng Med. 1984; 13:111–114. PMID: 6542880.
8. Panjabi MM, Greenstein G, Duranceau J, Nolte LP. Three-dimensional quantitative morphology of lumbar spinal ligaments. J Spinal Disord. 1991; 4:54–62. PMID: 1807531.
9. Pope MH, Hanley EN, Matteri RE, Wilder DG, Frymoyer JW. Measurement of intervertebral disc space height. Spine. 1977; 2:282–286.

10. Schultz AB, Belytschko TB, Andriacchi TP, Galante JO. Analog studies of forces in the human spine : mechanical properties and motion segment behavior. J Biomech. 1973; 6:373–383. PMID: 4732937.

Fig. 1
The geometry of the interspinous space is as follows : zone 1 : depth of skin level to spinous process; zone 2 : supraspinous ligament depth; zone 3 : interspinous ligament depth; zone 4 : the distance from the dural sheath to the surface of the ligamentum flavum (transversing the epidural fat+ligamentum flavum); zone 5 : the width of the thecal sac; zone 6 : interspinous distance (at the narrowest point); zone 7 : interspinous distance (at the widest point).
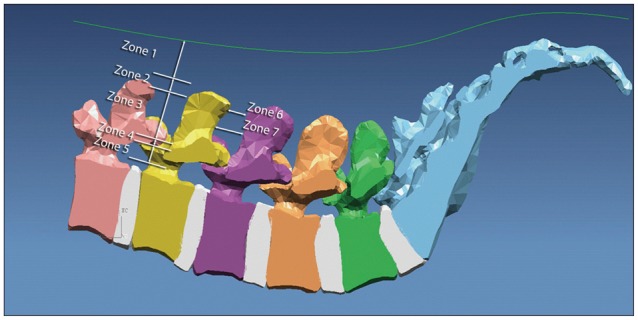
Fig. 2
The method of measuring zone 1 and zone 2+3 are shown in the above photographs. A : Zone 1, i.e., skin thickness, shown by the horizontal lines at each spinal level, is measured using a midline T2-weighted sagittal MRI image. B : Zone 2+3, the combination of supra- and interspinous ligaments, shown by the various measurements included above, is measured using a midline T2-weighted sagittal MRI image.
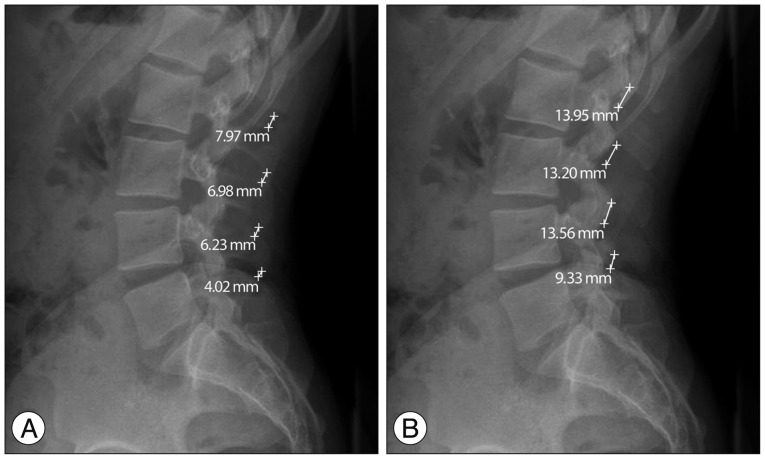
Fig. 3
The method of measuring zones 4 and 5. A : Zone 4, the distance from the dural sheath to the surface of the ligamentum flavum, is measured in this patient at L1-2 using a T2-weighted axial image. B : Zone 5, the anteroposterior width of the dural sac, is measured in an T2-weighted axial image shown here at L1-2.
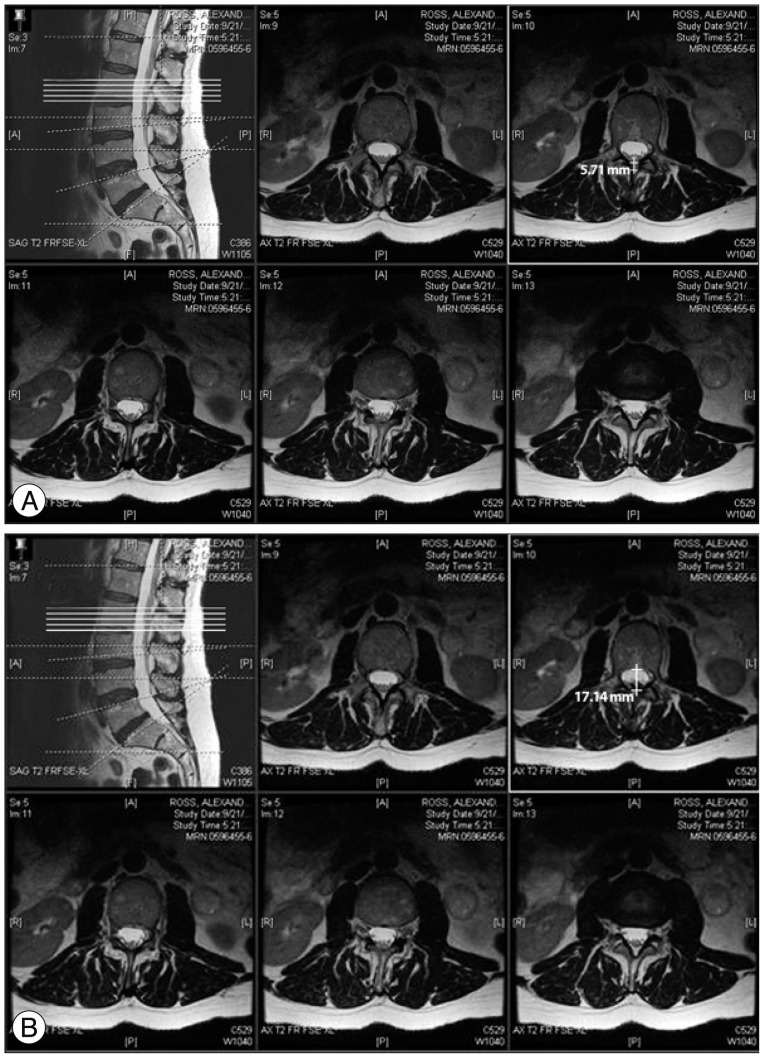
Fig. 4
The method of measuring zones 6 and 7. A : Zone 6, the interspinous distance at the narrowest point, is measured on plain X-ray, as shown. B : Zone 7, the interspinous distance at the widest point, is measured on plain X-ray, also shown here.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download