Abstract
Brucellosis is caused by gram-negative, aerobic, non-motile, facultative, intracellular coccobacilli belonging to the genus Brucella. A 50-year-old man working as an employee was admitted to neurosurgery clinic with severe low back, radicular right leg pain and hypoesthesia in right L4-5 dermatomes for 2 months. Brucella tube agglutination (Wright) test was positive in serum sample of the patient with a titer of 1/640. Brucella melitensis was isolated from blood culture. X-ray and MRI of the lomber spine showed massive collapse of L4 vertebral body. Neural tissue was decompressed and then posterior L3-5 short segment transpedicular screw fixation and stabilization was performed. Brucella melitensis was isolated from microbiologic culture of pathologic specimen. Antibiotic therapy was given as doxycycline 200 mg/day and rifampicin 600 mg/day for 6 months. Brucellosis is a systemic zoonotic infection and still an important public health problem in many geographical parts of the world. Vertebral body collapse caused by brucellosis occurs very rarely but represents a neurosurgical emergency because of its potential for causing rapidly progressive spinal cord compression and permanent paralysis. Neurosurgeons, emergency department personnel as well as infectious disease specialists should always keep a high index of suspicion and include brucellosis in the differential diagnosis of vertebral body collapse.
Brucellosis is caused by gram-negative, aerobic, non-motile, facultative, intracellular coccobacilli belonging to the genus Brucella. Brucellosis is spread from animals to humans by direct contact with infected tissue or by ingestion of milk or dairy products. In developed countries, human brucellosis is an occupation-related disease and occurs more commonly among farmers, veterinarians and laboratory workers. Osteoarticular involvement including spondylitis, sacroiliitis, osteomyelitis, peripheral arthritis, bursitis and tenosynovitis is the most common complication of brucellosis affecting up to 85% of patients9,10). We present a very rare case of brusella-related lumbar vertebral collapse.
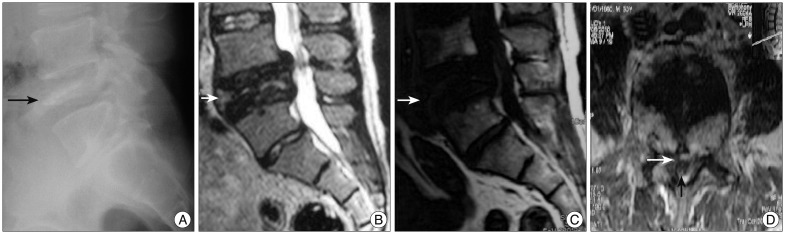
A 50-year-old man working as an employee was admitted to neurosurgery clinic with severe low back, radicular right leg pain and hypoesthesia in right L4-5 dermatomes for 2 months. His past history revealed that he had weight loss, night sweats and chills, fatigue and severe malaise for 4 months, and he consumed unpaesteurized milk and dairy products. On neurological examination there was 3/5 motor strength of right ankle dorsiflexion and hypoesthesia in distribution of right leg L4-5 dermatomes. Brucellosis was common in the area where the patient was living and brucella tube agglutination (Wright) test was routinely studied in suspected patients coming from that area. Brucella tube agglutination (Wright) test was studied in serum sample of the patient and was positive with a titer of 1/640. Brucella melitensis was isolated from blood culture. X-ray of the lumber spine showed massive collapse of L4 vertebral body (Fig. 1A). Magnetic resonance imaging (MRI) revealed fracture and collapse of the body of L4 vertebrae (Fig. 1B, C). The spinal canal was narroved by posterior elements of the vertebrae, therefore neural tissue was compressed (Fig. 1D).
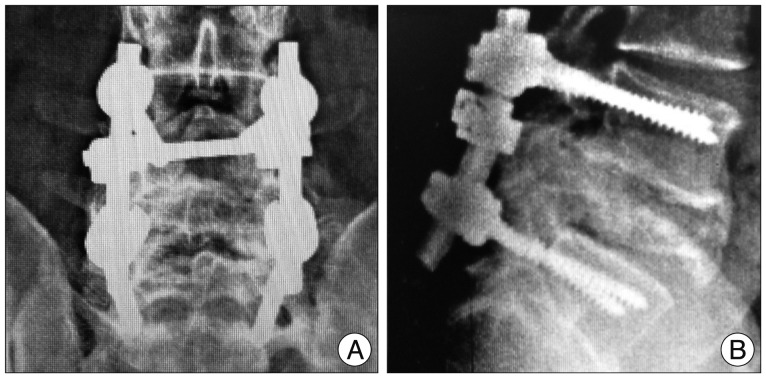
The patient was taken to the operation emergently a posterior midline approach and bilateral hemilaminotomy were done. Grey-yellow colored pathologic specimen was obtained from vertebral body and epidural space. Neural tissue was decompressed and then posterior L3-5 short segment transpedicular screw fixation and stabilization was performed (Fig. 2). Tricortical iliac crest wedge obtained from the same patient (autograft) was used for fusion. Neurological signs and symtoms of the patient were recovered after the operation. Brucella melitensis was isolated from microbiologic culture of pathologic specimen. Antibiotic therapy was given for brucellar infection as doxycycline 200 mg/day and rifampicin 600 mg/day for 6 months.
Brucellosis is a systemic zoonotic infection and still an important public health problem in many geographical parts of the world including the Mediterranean basin, the Arabian Gulf, South America countries, Mexico, North Africa, and Western and Central Asia 5,6,8,11). Brucellosis is caused by small, non-motile gram-negative facultative intracellular coccobacilli of the genus Brucella : Brucella melitensis, Brucella abortus, Brucella suis or Brucella canis11).
Brucellosis infection spreads hematogenously to tissues and mainly affects organs rich in mononuclear phagocytes, such as the liver, the spleen, the lymph nodes and the bone marrow. Osteo-articular involvement is the most common complication of chronic brucellosis. The type of skeletal involvement depends on the patient's age. The spine is the targeted site in the elderly, while the sacroiliac joints and knee predominate in children and young adults2-4,7,11). Brucellar spondylitis occurs most commonly in the lumbar region. Vertebral collapse due to brusellosis is very rarely reported1,11). In the present report we present a very rare form of brucellosis causing vertebral collapse.
A correct early diagnosis of brucellosis is important because it is an aggressive disease which requires immediate treatment. Both medical history of the patient and results of laboratory tests should be evaluated with detailed clinical information for diagnosis of brucellosis. Consumption of milk or dairy products are informative.
Standart brucella tube agglutination (Wright) test, blood culture and microbiologic culture of the pathologic specimen give exact diagnosis. The predominant radiological finding of spinal brucellosis is spondylitis or spondylodiscitis. Spinal brucellosis (spondylitis or spondylodiscitis) is a slowly progressive disease, similar with tuberculosis. Computed tomography scan and MRI have allowed more accurate and frequent detection of spinal brucellosis.
Different combinations of antimicrobial drugs are used to treat brusellosis. They are rifampicin, doxycycline, streptomycine, tetracycline, and ofloxacin. In addition to antibrucellar antibiotic therapy as a gold standard of treatment, the surgical removal of the lesion is also very important in the presence of compression. However, some cases are treated with instrumentation or a fixation procedure for spinal instability or collapse. Sometimes antibrucellar antibiotic therapy alone is enough if the correct diagnosis can be made without surgery.
Preventive measures are more important than therapeutic interventions to eradicate brucellosis. Patients at high risk for brucellosis should be subjected to long follow-up in order to diagnose and treat the disease at an early stage.
Vertebral body collapse caused by brucellosis occurs very rarely but represents a neurosurgical emergency because of its potential for causing rapidly progressive spinal cord compression and permanent paralysis. Neurosurgeons, emergency department personel as well as infectious disease specialists should always keep a high index of suspicion and include brucellosis in the differential diagnosis of vertebral body collapse.
References
1. Cebesoy FB, Balat O, Mete A. An extraordinary cause of vertebral fracture in pregnant woman : brucellosis. Arch Gynecol Obstet. 2009; 280:301–303. PMID: 19107498.

2. Chelli Bouaziz M, Ladeb MF, Chakroun M, Chaabane S. Spinal brucellosis : a review. Skeletal Radiol. 2008; 37:785–790. PMID: 17962938.
3. Franco MP, Mulder M, Gilman RH, Smits HL. Human brucellosis. Lancet Infect Dis. 2007; 7:775–786. PMID: 18045560.

4. Geyik MF, Gür A, Nas K, Cevik R, Saraç J, Dikici B, et al. Musculoskeletal involvement of brucellosis in different age groups : a study of 195 cases. Swiss Med Wkly. 2002; 132:98–105. PMID: 11971204.
5. González-Gay MA, García-Porrúa C, Ibañez D, García-País MJ. Osteoarticular complications of brucellosis in an Atlantic area of Spain. J Rheumatol. 1999; 26:141–145. PMID: 9918255.
6. Hasanjani Roushan MR, Mohrez M, Smailnejad Gangi SM, Soleimani Amiri MJ, Hajiahmadi M. Epidemiological features and clinical manifestations in 469 adult patients with brucellosis in Babol, Northern Iran. Epidemiol Infect. 2004; 132:1109–1114. PMID: 15635968.

7. Hashemi SH, Keramat F, Ranjbar M, Mamani M, Farzam A, Jamal-Omidi S. Osteoarticular complications of brucellosis in Hamedan, an endemic area in the west of Iran. Int J Infect Dis. 2007; 11:496–500. PMID: 17344084.

8. Sharif HS, Aideyan OA, Clark DC, Madkour MM, Aabed MY, Mattsson TA, et al. Brucellar and tuberculous spondylitis : comparative imaging features. Radiology. 1989; 171:419–425. PMID: 2704806.

9. Solera J, Lozano E, Martínez-Alfaro E, Espinosa A, Castillejos ML, Abad L. Brucellar spondylitis : review of 35 cases and literature survey. Clin Infect Dis. 1999; 29:1440–1449. PMID: 10585793.
10. Taşova Y, Saltoğlu N, Sahin G, Aksu HS. Osteoarthricular involvement of brucellosis in Turkey. Clin Rheumatol. 1999; 18:214–219. PMID: 11206346.

11. Turgut M, Turgut AT, Koşar U. Spinal brucellosis : Turkish experience based on 452 cases published during the last century. Acta Neurochir(Wien). 2006; 148:1033–1044. discussion 1044. PMID: 16944052.

Fig. 1
A : Lateral spine X-ray of the patient showing collapsed L4 vertebral body (arrow). B and C : Saggital T2 and T1-weighted MRI of the lumbar spine showing collapsed L4 vertebral body and compression of neural elements (white arrow). D : Axial T2-weighted MRI of the lumbar spine showing collapsed L4 vertebral body compressing neural elements (black arrow showing neural tissue, white arrow showing collapsed vertebral body).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download