Abstract
The cerebrospinal fluid tap test (CSFTT) is recommended as a key step in the diagnosis of idiopathic normal pressure hydrocephalus (iNPH). While there is no generally accepted evaluation period for ascertaining a CSFTT responder, a substantial number of patients are evaluated only once within 24 hours of the test for improvement in gait. We report an iNPH patient with a favorable response to shunt surgery, who was first judged a non-responder by this standard, though subsequently was judged a responder in virtue of repetitively testing gait over 7 days. A 68-year-old man presented with progressive impairment of gait, balance, and memory. He was diagnosed as iNPH with an Evans' ratio of 0.35. At first hospitalization, change in gait was evaluated 24 hours after the CSFTT. He didn't show any significant improvement and was judged as a non-responder. However, at the second CSFTT, we repetitively tested his change in gait over seven days. Forty-eight hours after the tap, he showed significant improvement in his gait. He was then confirmed as a responder. After the operation, the gait difficulties were almost fully resolved. Further studies developing the standard procedure of the CSFTT should be considered.
Idiopathic normal pressure hydrocephalus (iNPH) is an adult-onset syndrome of uncertain origin involving nonobstructive enlargement of the cerebral ventricles in combination with one or more of the symptoms of gait disturbance, urinary dysfunction, and cognitive impairment1). Because of the treatable nature of iNPH, selection of patients potentially benefitting from cerebrospinal fluid (CSF) shunt surgery is important.
The CSF tap test (CSFTT) is a simple procedure proven to have a high positive predictive value when correlated to successful shunt surgery23). Furthermore, many neurosurgical centers recommend using it as a key tool in the diagnosis of iNPH5). However, despite its excellent track record in predicting successful shunt surgery, the test has a relatively low sensitivity in diagnosing iNPH14). Most clinicians evaluate change in gait, a key component in the diagnosis of iNPH following the CSFTT only once, most often within 24 hours of the tap11,21).
From this point of view, we report an iNPH patient with delayed improvement after the CSFTT, following Japanese standards5,6). In general, the Japanese standards are considered popular and reasonable criteria in Asia for evaluating response to the CSFTT5,6). We proceeded with shunt surgery in virtue of a second CSFTT with an extended evaluation period over several days revealing the patient as a responder. The patient significantly recovered from his symptoms postoperatively.
A 68-year-old man presented to our hospital for evaluation of progressive impairment of gait, balance, and memory. Twenty months earlier, he had developed a short-stepped gait and impaired balance without urinary symptoms. There was progressive deterioration in his gait, and he suffered a few falls recently. His daughter described a 12-month gradual decline in his ability to express himself and, more recently, difficulties in carrying out complex tasks. She reported that his short-term memory had been functionally impaired over the past few months. There was reduced interest in completing instrumental activities of daily living.
He had accumulated a 40-pack-year smoking habit, but he had stopped smoking 5 years before presentation. His alcohol intake was restricted to social functions. He did not have a history of stroke or other neurological, metabolic, or neoplastic disorders which might produce dementia symptoms, or parkinsonism, or a history of hospitalization for depression. The patient was positive for diabetes mellitus.
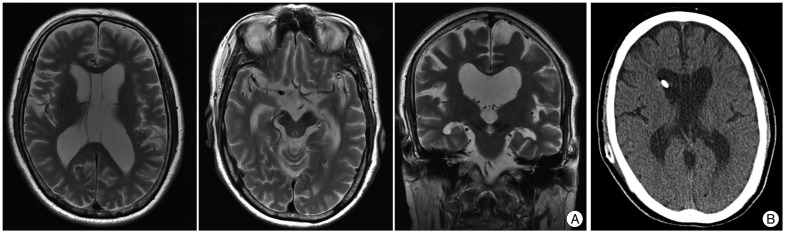
On initial examination, the patient's cognitive function was impaired [Korean Mini-Mental State Examination (K-MMSE) score 23 out of 30 and Clinical Dementia Rating Scale 1], and a frontal release sign (palmomental reflex) was present2,8). He exhibited a short-stride gait with shuffling. The patient had no rigidity in the limbs or neck. His postural reflexes were slightly impaired. Formal neuropsychological evaluation showed a deficit in visuospatial function (copy of the Rey-Osterrieth Complex Figure) and memory (Korean Hopkins Verbal Learning Test and recall and recognition of the Rey-Osterrieth Complex Figure) with frontal dysfunctions (Frontal Assessment Battery). All laboratory test results, including a blood-chemistry panel, complete blood count, thyroid function tests, measurement of vitamin B12 levels, and screening for inflammatory and infectious diseases such as neurosyphilis, were unremarkable. Brain magnetic resonance imaging revealed communicating hydrocephalus with an Evans' ratio of 0.354), and also showed CSF signal void in the cerebral aqueduct and enlargement of the temporal horns of the lateral ventricles (Fig. 1). He showed no evidence of a related antecedent event, such as head trauma, intracerebral hemorrhage, meningitis, or another known cause of secondary hydrocephalus. He was diagnosed as having iNPH following the consensus criteria of Relkin et al.17).
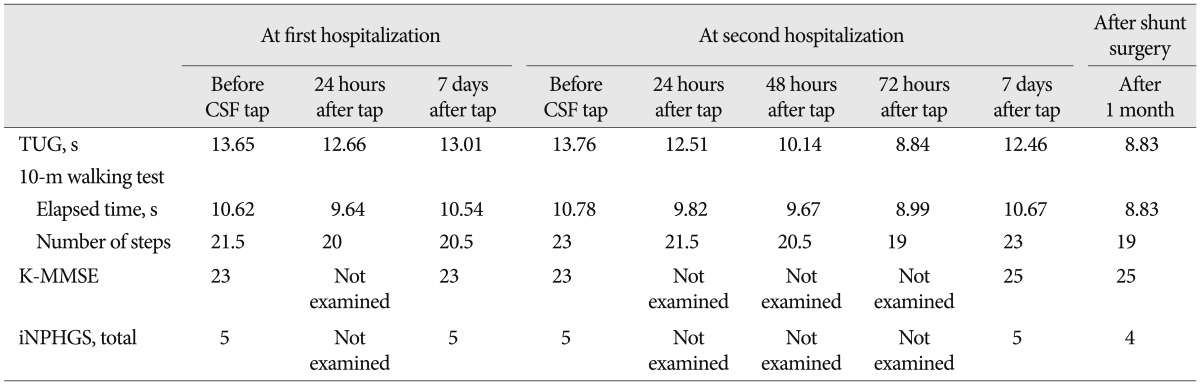
The following several psychological tests and walking tests were applied following the CSFTT. The iNPH Grading Scale (iNPHGS) is a clinician-rated scale for assessing the severity of each of the 3 disorders of iNPH (cognitive impairment, gait disturbance and urinary disturbance)9). A five-point subscale was used to rate the severity of each fundamental symptom of iNPH after an interview with patients and caregivers. The gait assessment included measurements of time and number of steps on the Timed Up and Go Test (TUG) and the 10-m walking test15,19). These are valid tests of functional mobility used in many studies to evaluate walking ability15,19). Both tests were separately performed four times, and the mean score was used.
At first hospitalization, a lumbar tap with removal of 40 mL of CSF was performed. Before and after the tap, he was evaluated using the iNPHGS, K-MMSE, TUG, and 10-m walking tests (Table 1). Change in gait was evaluated 24 hours after the tap11,21), while change in cognition and urination was evaluated at one week9). All trials were videotaped and analyzed by 2 experienced neurologists. Response to the CSFTT was evaluated using three major scales : iNPHGS, TUG and K-MMSE. The following criteria were used to identify responders : improvement of one point or more on the iNPHGS, more than 10% improvement in time on TUG, or more than 3 points improvement on the K-MMSE. These criteria were frequently used in previous studies5,6). He did not show sufficient improvement by these criteria, and was judged as a non-responder (Table 1). The subjective impression of the patient and his family members, as well as 2 experienced neurologists, regarding overall change in gait after the CSFTT was 'no improvement' within 24 hours. However, his daughter reported that his gait appeared to improve 2 or 3 days after the tap, and again became progressively worse at one week when he visited our clinic for the follow-up cognition test. At that time, the patient and his family wanted conservative treatment with observation instead of operation.
Over the next 3 months, there was deterioration in his gait and balance again. Trials of levodopa, with dosage up to 600 mg/day, offered no benefit. He suffered multiple falls during the ensuing month. He finally required assistance when walking on an uneven road.
At the second hospitalization for the CSFTT, we examined his change in gait over seven days in more detail, considering the findings from the first hospitalization (Table 1). It was noticed that his gait began to improve 24 hours after tap and more so 48 hours after tap, and eventually he did show improvement by the criteria : more than 10% improvement in time on TUG. His gait got worse again at one week. The patient and his family were repeatedly asked about their subjective impressions regarding overall improvement after the CSFTT. They agreed that there was temporary improvement 72 hours after tap. The diagnosis was then confirmed as a responder and he underwent shunt surgery. After the operation he improved gradually. The gait difficulties were almost fully resolved, and the balance problem disappeared after 1 month (Table 1). The K-MMSE score also improved to 25.
Although the surgical procedure for iNPH is generally considered technically easy, there are risks of complications, both short term and long term10,20). Thus, methods for dynamic measurements of CSF circulation as well as various clinical tests have been used to predict the outcome of a shunt operation. In general, response to a CSFTT is considered to be useful for predicting a favorable response to shunt surgery, particularly in iNPH patients. And because it is easy and quite safe to perform in practice, the Japanese guidelines for management of iNPH recommended the CSFTT as one of the most important diagnostic tests5). This test also has the advantage of being simple to perform without any specialized equipment. Therefore, the CSFTT is generally recommended as a key step in the diagnosis of iNPH.
However, even in the two most frequently used guidelines for iNPH, there are no standard protocols for evaluation following the CSFTT5,17). The procedure and evaluation of the CSFTT vary between centers. The optimal time for evaluation of the tap test has not been systematically examined. Thus, if evaluation is made at the wrong time, patients who would be indicated for surgery may be overlooked and considered as non-responders. Particularly, a challenge for the CSFTT is the high variability in the judgment of results (responder or non-responder). This might also explain the low sensitivity of the tap test (ranging from 26% to 62%)14). Our patient also did not show sufficient improvement by the aforementioned criteria 24 hours after the tap test, and was judged as a non-responder at the first hospitalization. The Japanese standards are generally considered popular and reasonable criteria for judgment of response to CSFTT in Asia5,6).
We think that the low sensitivity of the CSFTT is at least partly compensated for by repetitive testing over several days. As long as we do the tap test, we should cautiously analyze the results. If the patient shows delayed improvement after CSFTT, we must be more careful in the judgment of the results (responder or non-responder). Our iNPH patient with a favorable response to shunt surgery showed improvement by the criteria 48 hours after tap : more than 10% improvement in time on the TUG test. It was a delayed response to some degree, because in most previous studies involving the CSFTT, it is recommended that the change in gait can be evaluated only once within the first 24 hours11,21). In fact, most previous studies assessed the effect of the CSFTT on gait and mental impairment within eight hours after CSF removal3,7,13,16,18,22,23). Furthermore, we found delayed improvement after the CSFTT in our case because of repetitive testing over several days. The subjective impression of patient and his family members, as well as clinicians, regarding overall change in gait after a CSFTT can also change with time. And considering learning effects, it was also important for us in our diagnosis between a responder and non-responder that our patient's gait got worse at one week again. It might be essential to evaluate the response of a tap test repetitively for at least several days. In general, it was thought that the continuous external lumbar drainage (ELD) might achieve a clinically more useful diagnostic sensitivity than the CSFTT because the former test drained a larger CSF volume14). However, another explanation for the higher sensitivity of ELD could be the longer evaluation period allowing for more cautious analysis. However, ELD is an invasive and costly test.
As the disease progresses and the ventricles get larger, they may lose elasticity12). If the ventricles are slightly shrunken by CSF removal, the elasticity of the ventricles may recover along with symptomatic improvement over a certain period12). We suppose the recovery time might be variable depending on the individual differences or the state of illness. But, this has not been systematically studied.
This is an interesting report of an iNPH patient with a favorable response to shunt surgery who showed delayed improvement after the CSFTT, despite initially being classified as a non-responder. Repeated evaluation of change of gait over 7 days may increase the sensitivity in identifying CSFTT responders. However, further studies developing the standard procedure of the CSFTT should be considered to establish this hypothesis.
Acknowledgements
We thank Wade Martin of Medical Research International for his critical review of this manuscript.
This work was supported by Biomedical Research Institute grant, Kyungpook National University Hospital (2012).
References
1. Adams RD, Fisher CM, Hakim S, Ojemann RG, Sweet WH. Symptomatic occult hydrocephalus with "normal" cerebrospinal-fluid pressure.a treatable syndrome. N Engl J Med. 1965; 273:117–126. PMID: 14303656.

2. Choi SH, Na DL, Lee BH, Hahm DS, Jeong JH, Yoon SJ, et al. Estimating the validity of the Korean Version of Expanded Clinical Dementia Rating (CDR) Scale. J Korean Neurol Assoc. 2001; 19:585–591.
3. Damasceno BP, Carelli EF, Honorato DC, Facure JJ. The predictive value of cerebrospinal fluid tap-test in normal pressure hydrocephalus. Arq Neuropsiquiatr. 1997; 55:179–185. PMID: 9629375.

4. Evans WA. An encephalographic ratio for estimating ventricular enlargement and cerebral atrophy. Arch Neurol Psychiatry. 1942; 47:931–937.

5. Ishikawa M, Hashimoto M, Kuwana N, Mori E, Miyake H, Wachi A, et al. Guidelines for management of idiopathic normal pressure hydrocephalus. Neurol Med Chir (Tokyo). 2008; 48(Suppl):S1–S23. PMID: 18408356.
6. Ishikawa M, Hashimoto M, Mori E, Kuwana N, Kazui H. The value of the cerebrospinal fluid tap test for predicting shunt effectiveness in idiopathic normal pressure hydrocephalus. Fluids Barriers CNS. 2012; 9:1. PMID: 22239832.

7. Kahlon B, Sundbärg G, Rehncrona S. Comparison between the lumbar infusion and CSF tap tests to predict outcome after shunt surgery in suspected normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry. 2002; 73:721–726. PMID: 12438477.

8. Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997; 15:300–308.
9. Kubo Y, Kazui H, Yoshida T, Kito Y, Kimura N, Tokunaga H, et al. Validation of grading scale for evaluating symptoms of idiopathic normal-pressure hydrocephalus. Dement Geriatr Cogn Disord. 2008; 25:37–45. PMID: 18025828.

10. Lee WC, Seo DH, Choe IS, Park SC, Ha YS, Lee KC. A comparative result of ventriculoperitoneal shunt, focusing mainly on gravity-assisted valve and programmable valve. J Korean Neurosurg Soc. 2010; 48:251–258. PMID: 21082054.

11. Lee WJ, Wang SJ, Hsu LC, Lirng JF, Wu CH, Fuh JL. Brain MRI as a predictor of CSF tap test response in patients with idiopathic normal pressure hydrocephalus. J Neurol. 2010; 257:1675–1681. PMID: 20512347.

12. Lim TS, Yong SW, Moon SY. Repetitive lumbar punctures as treatment for normal pressure hydrocephalus. Eur Neurol. 2009; 62:293–297. PMID: 19713705.

13. Malm J, Kristensen B, Karlsson T, Fagerlund M, Elfverson J, Ekstedt J. The predictive value of cerebrospinal fluid dynamic tests in patients with th idiopathic adult hydrocephalus syndrome. Arch Neurol. 1995; 52:783–789. PMID: 7639630.

14. Marmarou A, Bergsneider M, Klinge P, Relkin N, Black PM. The value of supplemental prognostic tests for the preoperative assessment of idiopathic normal-pressure hydrocephalus. Neurosurgery. 2005; 57(3 Suppl):S17–S28. discussion ii-v. PMID: 16160426.

15. Podsiadlo D, Richardson S. The timed "Up & Go" : a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991; 39:142–148. PMID: 1991946.

16. Ravdin LD, Katzen HL, Jackson AE, Tsakanikas D, Assuras S, Relkin NR. Features of gait most responsive to tap test in normal pressure hydrocephalus. Clin Neurol Neurosurg. 2008; 110:455–461. PMID: 18359152.

17. Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM. Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery. 2005; 57(3 Suppl):S4–S16. discussion ii-v. PMID: 16160425.

18. Sand T, Bovim G, Grimse R, Myhr G, Helde G, Cappelen J. Idiopathic normal pressure hydrocephalus : the CSF tap-test may predict the clinical response to shunting. Acta Neurol Scand. 1994; 89:311–316. PMID: 8085427.

19. Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people : Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002; 82:128–137. PMID: 11856064.

20. Udvarhelyi GB, Wood JH, James AE Jr, Bartelt D. Results and complications in 55 shunted patients with normal pressure hydrocephalus. Surg Neurol. 1975; 3:271–275. PMID: 1154252.
21. Virhammar J, Cesarini KG, Laurell K. The CSF tap test in normal pressure hydrocephalus : evaluation time, reliability and the influence of pain. Eur J Neurol. 2012; 19:271–276. PMID: 21801282.

22. Walchenbach R, Geiger E, Thomeer RT, Vanneste JA. The value of temporary external lumbar CSF drainage in predicting the outcome of shunting on normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry. 2002; 72:503–506. PMID: 11909911.
23. Wikkelsø C, Andersson H, Blomstrand C, Lindqvist G. The clinical effect of lumbar puncture in normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry. 1982; 45:64–69. PMID: 7062072.

Fig. 1
A : Preoperative brain MRI; T2-weighted axial images show the lateral ventricular enlargement with CSF signal void in the cerebral aqueduct. Thinning of the corpus callosum with enlargement of the temporal horns of the lateral ventricles is also demonstrated in T2-weighted coronal image. B : Postoperative brain CT image still shows the lateral ventricular enlargement. However, after the operation he improved gradually. The gait difficulties were almost fully resolved, and the balance problem disappeared after 1 month. CSF : cerebrospinal fluid.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download