Abstract
Objective
To clarify the landmark for deciding the entry point for C1 lateral mass screws via the posterior arch by using 3-dimensional (3D) computed images.
Methods
Resnick insisted that the C1 posterior arch could be divided into pure posterior and lateral lamina (C1 pedicle). Authors studied where this transition point (TP) is located between the posterior lamina and the C1 pedicle and how it can be recognized. The 3D computed images of 86 cadaver C1s (M : F=45 : 41) were used in this study.
Results
The superior ridge of the C1 posterior arch had 2 types of orientation. One was in the vertical direction in the C1 posterior lamina and the other was in the horizontal direction in the C1 pedicle. The TP was located at the border between the 2 areas, the same site as the posterior end of the groove of the vertebral artery. On posterior-anterior projection, the posterior arch was sharpened abruptly at TP. We were unable to identify the TP in 6.4% of specimens due to complete or partial osseous bridges. A total of 93.8% of the TP were located between the most enlarged point of the spinal canal and the medial wall of the vertebral artery.
Although there are various techniques for treating atlantoaxial instability, C1-C2 posterior fusion with screw and rod fixation has recently become the most common. This individual screw fixation, suggested by Goel and Laheri5) and Harms and Melcher6) has superiority over posterior transarticular screw fixation because C1-2 transarticular fixation has several limitations, including the position of the vertebral artery (VA), thoracic kyphosis, and obesity16,17). However, C1-C2 screw fixation is still challenging owing to the complexity of the anatomy of the C1-C2 area, bleeding from the venous plexus, and injury to the VA, and/or C2 nerve15,18). Therefore, there have been many studies on the anatomy of C1-C2 area, and there are several techniques for inserting lateral mass screws into the C12-4,6,10,15,17,18).
Resnick et al.17) and Tan et al.21) reported a technique called C1 pedicle screw fixation (screw insertion via the lateral laminar arch); this new technique has been shown to minimize bleeding from the venous plexus and reduce C2 nerve damages. Moreover, it is biomechanically superior to lateral mass screw fixation11). Resnick et al.17) used computed tomography (CT) navigation and Tan et al.21) used the posterior tubercle of the C1 as a landmark; however, there is a need for localizing the entry point for screw insertion because not every institute has a navigation system and, sometimes, the posterior tubercle of C1 arch is not suitable for a precise landmark. Thus, a more precise or an additional landmark of the posterior arch is essential for localizing the entry point for C1 pedicle screw insertion. Some previous studies described this entry point in the posterior arch and Ma et al.12) showed the landmark in other cervical levels for a C1 pedicle screw entry point8,10). However, these landmarks for the entry point are still uncertain in a real operating field. Therefore, this study was undertaken to clarify the landmark of the C1 itself for deciding the entry point of C1 pedicle screw.
This study was approved by the Institutional Review Board. This study details the entry point for C1 lateral mass screws via the C1 pedicle. Information in this study is based on digital Korean data. CT was carried out on the atlas of 86 Korean cadavers (45 men and 41 women). These CT images were obtained by using a slice thickness of 1 mm. The cadavers were identified on the basis of age and sex : the mean age of the subjects was 63.7 years (range, 21-72 years) in men and 66.3 years (range, 18-74 years) in women. The images were reconstructed to 3-dimensional (3D) structures by using Mimics® Version 14.01 (Materialise Inc.) and were measured by using Hypermesh® Ver8.0 (Altair Engeeniring Inc.).
Resnick et al.17) divided the lamina of the C1 into the posterior lamina and the C1 pedicle (lateral laminar), but no distinct the border was mentioned. Thus, in this study, it was prescribed that transition point (TP) was the border of the posterior laminar and the lateral laminar, and this border of both parts was the most posterior end of the groove of the VA, where the orientation of the lamina was changed from a vertical direction to a horizontal direction in the posterior view (Fig. 1).
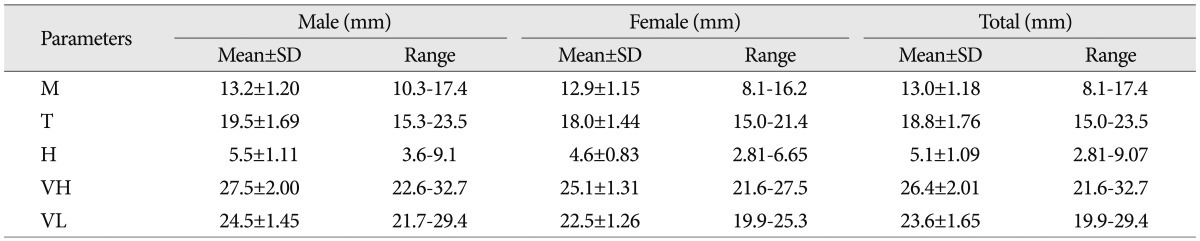
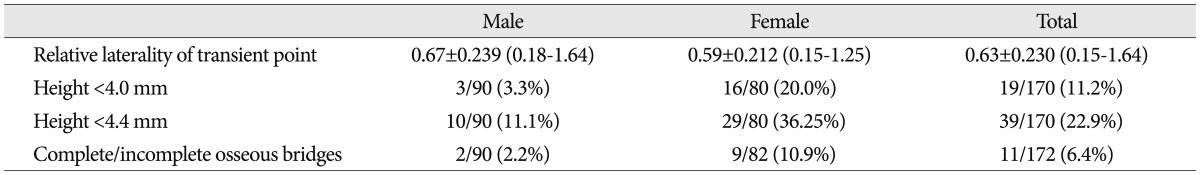
Linear parameters (left/right maximal canal diameter from midline, minimal C1 pedicle height, left/right distance from midline to the outlet of the transverse foramen, left/right distance from midline to the inlet of the transverse foramen, and left/right distance from midline to transient point) were measured using the Hypermesh® (Fig. 2). The cortical bone was defined as the area with a CT density of 250 Hounsfield units. An accuracy test of the estimated linear parameters was conducted by measuring the parameters of real vertebral bodies, which revealed an error rate of 0.89%. Calculation of the relative laterality ratios of TP is shown in Fig. 3. A ratio of 0 indicated that the laterality of the TP was located at the maximal lateral point of the spinal canal, whereas a ratio of 1 meant that the laterality of the TP was located at the medial end of the transverse foramen. Paired t test and independent t-test were used to determine the differences between each parameter (p<0.01).
We studied 172 C1 pedicles in 86 cadavers. The TP could not be found in 11 pedicles (6.4%) due to variations in the lateral laminar arches of the C1, such as ponticulus posticus or incomplete osseous bridges. The means and standard deviation of the means of all the measured linear parameters are presented in Table 1.
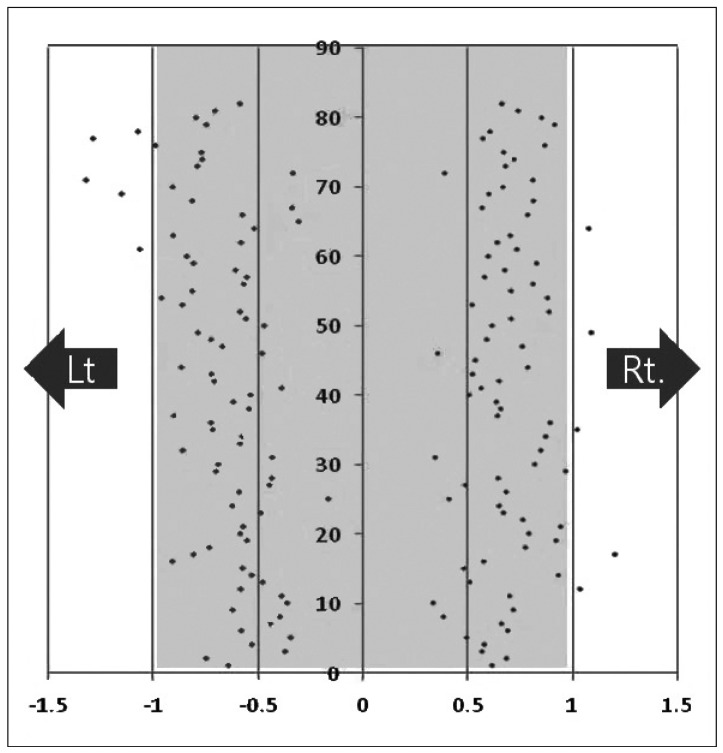
All parameters from male subjects, except canal diameter were significantly larger than those in female subjects (p<0.05). Maximal canal diameter from midline was larger in male subjects, but the difference was not significant because of large individual variations. The incidence of pedicle height <4.0 mm was 19 (11.2%; men 3.3%, women 20%) out of 170 pedicles (2 pedicles were excluded because of large ponticulus posticuses). Considering the limitation of CT image accuracy (0.404 mm; this possibility of error should be considered for minimizing possibility of overestimate in measuring with 3D CT images), the incidence of pedicle height <4.4 mm was 39 out of 170 pedicles (Table 2). The distance from midline to the transverse foramen showed a significant difference between the inlet and the outlet; the inlet was more medially located than was the outlet (p=0.000). The calculated data on the relative laterality of the TPs are presented in Fig. 3; almost all TPs were located within the C1 pedicle area (93.8%, 151 out of 161 C1 lateral laminar). It meant that TPs were always located nearby C1 pedicle area and TP could be a good landmark for determining entry point after checking preoperative 3D CT.
Atlantoaxial instability is a rare but a very serious condition that requires immediate rigid fixation of the C1-2. Goel and Laheri5) first reported on C1-2 fixation by using C1 lateral mass and C2 pedicles screw with plates and screws, Harms et al.6) modified the technique by using poly axial screws and top loading rods. Compared to other C1-2 fixation methods, this technique has more advantages but is still challenging. Thus, there were efforts to develop a safer method and to evaluate the risk factors that might cause serious complications13,15). Resnick et al.17) and Tan et al.21) reported on C1 lateral mass screw fixation via the C1 pedicle. This technique has several advantages over direct lateral mass screwing including biomechanical aspect; Stiffness and pullout strength of the unicortical C1 pedicle screw are similar to those of the bicortical lateral mass screw, and it can reduce the possibility of injury of carotid artery injury11,14). However, it has a potential risk of injury of the VA at vertebral groove (V3) and the C1 pedicle screw cannot be applied in some populations due to their anatomic condition1,8,10). Therefore, many studies have reported on pedicle height and its variations in their populations (Japanese, Chinese, etc.), but there has been no Korean C1 data8,20). Moreover, there has been only one study that reported concerning the laterality of the entry point of the C1 pedicle screw : Ma and colleagues used the C2-3 facet as a landmark for determining the laterality of the C1 pedicle screw12,13). However, the C1-2 is a very movable joint, especially with regard to rotation, even in normal condition. Therefore, it is insecure to refer to other levels when determining the entry point in the C1 pedicle in case that there is such instability in the C1-C2 joint. Thus, exposure of the rear surface of the C1 lateral mass should be performed in that condition, even in case of C1 pedicle screwing without help of a navigation system, which means it is impossible to say that venous bleeding in C1 pedicle screw fixation is less than that in direct C1 lateral mass screw fixation. Therefore, it is very important to determine a landmark (TP) for the entry point of the C1 pedicle screw in the atlas itself. In our study, the transition point of the C1 lamina first was named and then recognized in anatomic feature of the transition point in the C1 lamina. Resnick et al.17), Tan et al.21), and Ma et al.12) mentioned the division of the C1 posterior arch into the pedicle and posterior laminae. Their comprehensive anatomic division was due to the similarity of the structure and surroundings between pedicles in other vertebrae and those of the atlas. However, no author has mentioned about the border. If there are 2 parts continuing structures, there must be a border between each other. Unfortunately, they thought the border was uncertain, but the posterior atlanto-occipital membrane, which is similar to the ligamentum flavum, expands laterally to the posterior end of the groove of the VA and suboccipital nerve (C1). This anatomic feature helped us to define the border (TP) between the pedicle and posterior lamina in the C1 (Fig. 4)22).
The result of this study showed that the TP could be determined in 93.6% due to some variation, such as complete or incomplete ponticulus posticus. The incidence of variation in the C1 of Korean subjects (6.4%) is similar to that in Japanese (7%) and Turkish (7.6%) : meanwhile, African (complete type, 14.2%) and European (complete type, 16.6%) subjects have a higher incidence of C1 variations than do Korean1,7-9,20). This lower incidence of variation in the C1 makes it more feasible to determine an entry point based on the TP during inserting lateral mass screws via the C1 pedicle in the Korean population. Transition points generally were located within the pedicle width (93.8%) in the posterior view, which means that operators can use this TP as a landmark by checking preoperative 3D CT images when they cannot depend on a navigation system (Fig. 5).
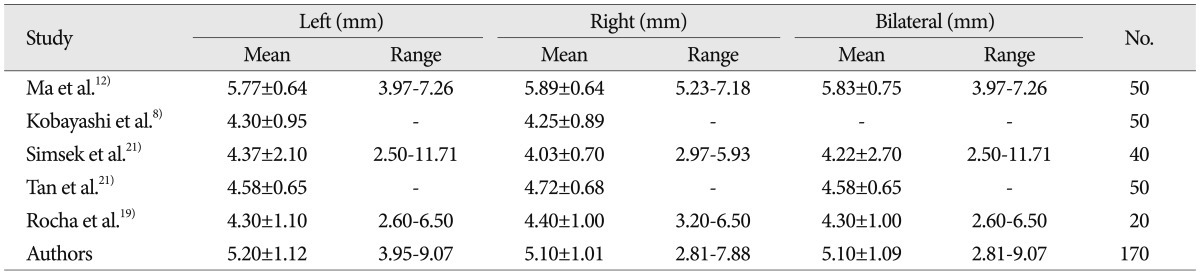
Comparison of the minimal pedicle height with previous studies is shown in Table 3. Although there were minor differences, our results were similar to previous studies. In our study, new parameters were added; distances from midline to the transverse foramen inlet and outlet were measured separately because the laterality of the transverse foramen inlet and outlet was different. Results showed that the outlet of the transverse foramen was located more laterally, which means that the lateral safety zone at the laminar level was larger than that just below the lamina (p<0.05) (Table 1).
The minimal height of the C1 pedicle is the most important limitation of C1 pedicle screwing because a 3.5-mm screw usually is used for lateral mass fixation. For this reason, some studies on the lateral C1 lamina have documented the height and rate of minimal height <4 mm. In our study, 11.2% of the specimens were <4 mm in height. Considering the limitation of the accuracy of CT images, 22.9% of specimens were <4.4 mm in height. This result seems to be similar to Ma et al.12) and Christensen et al.1) and a lower rate comparing another study8). Direct comparison of these studies is difficult because there are some biases, including differences between dried and fresh specimens and the limitation of CT images. However, it seems to be feasible to insert C1 lateral mass screw via the C1 pedicle in the majority of Korean population. Moreover, the entry point and suitability for screwing can be calculated by recognition of the TP between the C1 pedicle and C1 posterior lamina on preoperative 3D CT images.
Acknowledgements
This work was funded by Gangneung Asan Hospital (Biomedical Research Center Promotion fund).
References
1. Christensen DM, Eastlack RK, Lynch JJ, Yaszemski MJ, Currier BL. C1 anatomy and dimensions relative to lateral mass screw placement. Spine (Phila Pa 1976). 2007; 32:844–848. PMID: 17426627.

2. Chun HJ, Bak KH. Targeting a safe entry point for c2 pedicle screw fixation in patients with atlantoaxial instability. J Korean Neurosurg Soc. 2011; 49:351–354. PMID: 21887393.

3. Gebauer M, Barvencik F, Briem D, Kolb JP, Seitz S, Rueger JM, et al. Evaluation of anatomic landmarks and safe zones for screw placement in the atlas via the posterior arch. Eur Spine J. 2010; 19:85–90. PMID: 19882180.

4. Goel A, Kulkarni AG. Re : Tan M, Wang H, Wang Y, et al. : Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine. 2003;28:888-95. Spine (Phila Pa 1976). 2004; 29:1706. author reply 1706. PMID: 15284522.
5. Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien). 1994; 129:47–53. PMID: 7998495.

6. Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976). 2001; 26:2467–2471. PMID: 11707712.

7. Karau PB, Ogengo JA, Hassanali J, Odula P. Anatomy and prevalence of atlas vertebrae bridges in a Kenyan population : an osteological study. Clin Anat. 2010; 23:649–653. PMID: 20533509.

8. Kobayashi Y, Kikuchi S, Konno S, Sekiguchi M. Insertion of lateral mass screw of the atlas via the posterior arch : anatomical study of screw insertion using dry bone samples of the atlas from Japanese cadavers. J Orthop Sci. 2008; 13:452–455. PMID: 18843460.

9. Lamberty BG, Zivanović S. The retro-articular vertebral artery ring of the atlas and its significance. Acta Anat (Basel). 1973; 85:113–122. PMID: 4197316.

10. Lee MJ, Cassinelli E, Riew KD. The feasibility of inserting atlas lateral mass screws via the posterior arch. Spine (Phila Pa 1976). 2006; 31:2798–2801. PMID: 17108832.

11. Ma XY, Yin QS, Wu ZH, Xia H, Liu JF, Xiang M, et al. C1 pedicle screws versus C1 lateral mass screws : comparisons of pullout strengths and biomechanical stabilities. Spine (Phila Pa 1976). 2009; 34:371–377. PMID: 19214096.
12. Ma XY, Yin QS, Wu ZH, Xia H, Liu JF, Zhong SZ. Anatomic considerations for the pedicle screw placement in the first cervical vertebra. Spine (Phila Pa 1976). 2005; 30:1519–1523. PMID: 15990666.

13. Ma XY, Yin QS, Wu ZH, Xia H, Zhong SZ, Liu JF, et al. [Anatomic identification of the location of the pedicle of atlas with the lateral mass of C2 to C4 as the landmark]. Zhonghua Wai Ke Za Zhi. 2005; 43:774–776. PMID: 16083577.
14. Murakami S, Mizutani J, Fukuoka M, Kato K, Sekiya I, Okamoto H, et al. Relationship between screw trajectory of C1 lateral mass screw and internal carotid artery. Spine (Phila Pa 1976). 2008; 33:2581–2585. PMID: 19011539.

15. Pan J, Li L, Qian L, Tan J, Sun G, Li X. C1 lateral mass screw insertion with protection of C1-C2 venous sinus : technical note and review of the literature. Spine (Phila Pa 1976). 2010; 35:E1133–E1136. PMID: 20885280.
16. Resnick DK, Benzel EC. C1-C2 pedicle screw fixation with rigid cantilever beam construct : case report and technical note. Neurosurgery. 2002; 50:426–428. PMID: 11844283.

17. Resnick DK, Lapsiwala S, Trost GR. Anatomic suitability of the C1-C2 complex for pedicle screw fixation. Spine (Phila Pa 1976). 2002; 27:1494–1498. PMID: 12131706.

18. Rhee WT, You SH, Kim SK, Lee SY. Troublesome occipital neuralgia developed by c1-c2 harms construct. J Korean Neurosurg Soc. 2008; 43:111–113. PMID: 19096615.

19. Rocha R, Safavi-Abbasi S, Reis C, Theodore N, Bambakidis N, de Oliveira E, et al. Working area, safety zones, and angles of approach for posterior C-1 lateral mass screw placement : a quantitative anatomical and morphometric evaluation. J Neurosurg Spine. 2007; 6:247–254. PMID: 17355024.

20. Simsek S, Yigitkanli K, Comert A, Acar HI, Seckin H, Er U, et al. Posterior osseous bridging of C1. J Clin Neurosci. 2008; 15:686–688. PMID: 18378457.

21. Tan M, Wang H, Wang Y, Zhang G, Yi P, Li Z, et al. Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine (Phila Pa 1976). 2003; 28:888–895. PMID: 12942004.

22. Williams PL, Warwick R, Dyson M, Bannister LH. Gray's Anatomy. ed 37. New York: Churchill Livingstone, Inc;1989. p. 494.
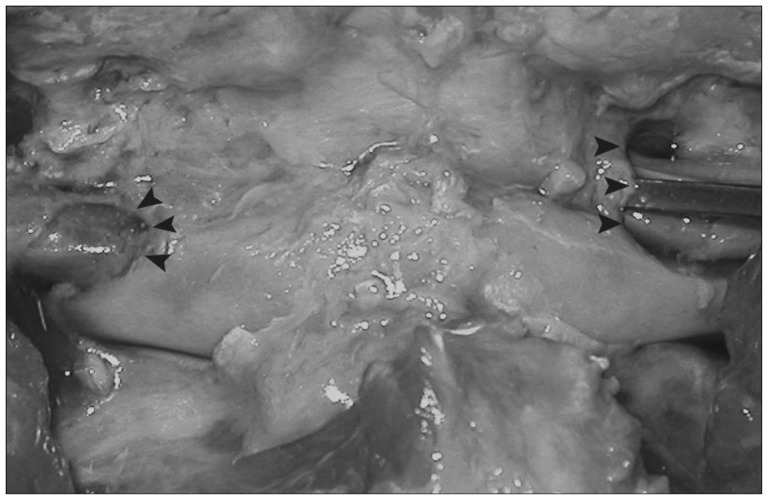
Fig. 1
Definition of the transition point (TP). A : The posterior end (asterisk) of the groove of the vertebral artery can be seen in the posterior view from slightly above the lamina by 10-15°. B : The same site (arrow head) is denoted in the superior view of the atlas. C-F : Images are posterior views of C1 in various angles (C : +30°, D : +15°, E : 0°, F : -30°, asterisk : TP).
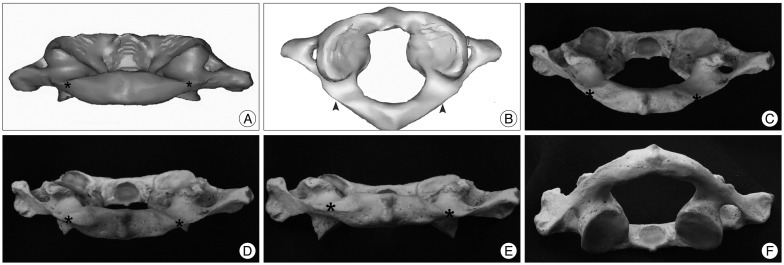
Fig. 2
Two orthogonal views (A : top; B : posterior side) of an atlas. H : minimal height of the C1 lateral lamina (C1 pedicle), Lt/Rt : left and right, M : maximal spinal canal diameter from midline, T : distance from midline to TP, VH : distance from midline to the medial side of the transverse foramen outlet, VL : distance from midline to the medial side of the transverse foramen inlet.
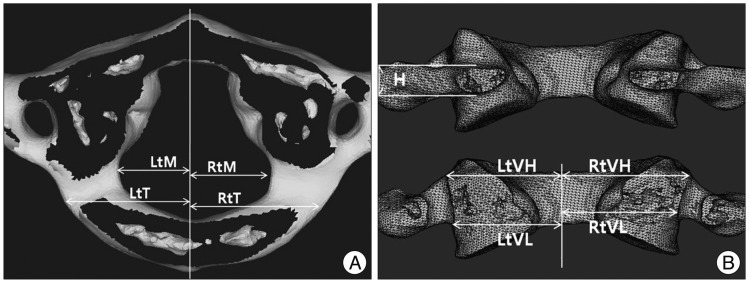
Fig. 3
Relative laterality ratio of a TP. This shows where a transition point is located comparing the safety zone between the spinal canal and the transverse foramen. Ratio=T/(VL - M). TP : transition point, VL : distance from midline to the medial side of the transverse foramen inlet, T : distance from midline to TP, M : maximal spinal canal diameter from midline.
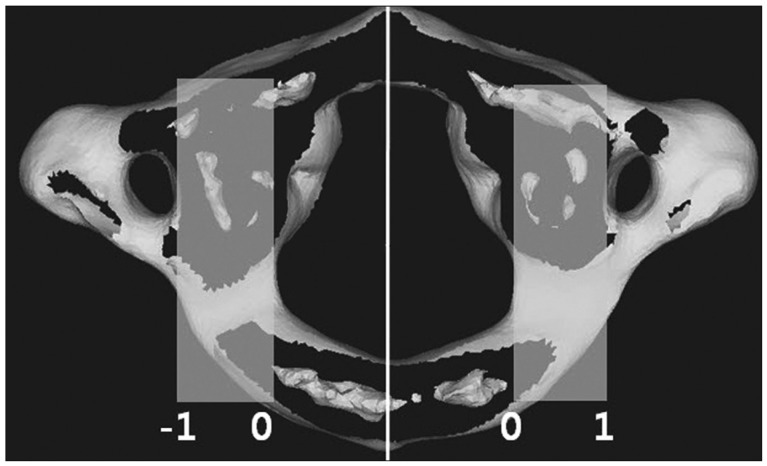
Fig. 5
Distribution of TPs. Individual dots show the relative laterality ratio of TP. X-axis : the relative laterality ratio, Y-axis : cadaver number, TP : transition point.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download