Abstract
We recently experienced self-detachment of the Solitaire stent during mechanical thrombectomy of acute ischemic stroke. Then, we tried to remove the detached stent and to recanalize the occlusion, but failed with endovascular means. The following diffusion weighted image MRI revealed no significant increase in infarction size, therefore, we performed surgical removal of the stent to rescue the patient and to elucidate the reason why the self-detachment occurred. Based upon the operative findings, the stent grabbed the main thrombi but inadvertently detached at a severely tortuous, acutely angled, and circumferentially calcified segment of the internal carotid artery. Postoperative angiography demonstrated complete recanalization of the internal carotid artery. The patient's neurological deficits gradually improved, and the modified Rankin scale score was 2 at three months after surgery. In the retrospective case review, bone window images of the baseline computed tomography (CT) scan corresponded to the operative findings. According to this finding, we hypothesized that bone window images of a baseline CT scan can play a role in terms of anticipating difficult stent retrieval before the procedure.
Among the mechanical thrombectomy devices used for cases of acute ischemic stroke, the Solitaire stent (eV3, Plymouth, MN, USA) is one of the mostly used and reported device recently due to its fully retrievable and self-expandable property2,7). However, mechanical thrombectomy using the Solitaire stent is not always successful, and unexpected self-detachment is possible during the retrieval of the stent through severely tortuous or atherosclerotic vessels4). We recently experienced the self-detachment of a Solitaire stent and failed to recanalize the occlusion with endovascular method. Then, we performed surgical removal of the stent in order to rescue the patient and elucidate the reason why the self-detachment occurred. Based on the operative findings, the stent was likely to fail to pass the acutely angled and circumferentially calcified internal carotid artery (ICA) segment, and it finally detached inadvertently at the tortuous segment.
A 78-year-old female presented with left hemiparesis (2/5) at four hours from onset of symptoms. She was taking oral anticoagulation medication (Warfarin 2 mg daily) due to atrial fibrillation. The baseline National Institute of Health Stroke Scale score was 18. The computed tomography (CT) brain scan was normal, magnetic resonance imaging (MRI) showed acute infarction in diffusion weighted MRI and diffusion and perfusion mismatch (Fig. 1). Right ICA occlusion from the petrous segment was confirmed by cerebral angiography (Fig. 2A). In our practice, forced suction thrombectomy with the Penumbra reperfusion catheter (Penumbra, Alameda, CA, USA) is usually first undertaken to recanalize large vessel occlusion3), and if failure occurs, Solitaire stent assisted thrombectomy is then performed.
Under local anesthesia, forced suction thrombectomy with the 041 F Penumbra Reperfusion catheter was performed. Following two attempts of forced suction thrombectomy, a 10 mm sized visible clot was retrieved, and the ICA was fully recanalized. However, a distal M1 segment occlusion remained (Fig. 2B). We switched to Solitaire AB stent assisted thrombectomy after failure of the remained occlusion with previous technique. After confirming the location of the occlusion via distal angiography with a Prowler Selector Plus microcatheter (Cordis Neurovascular, Miami Lakes, FL, USA), a Solitaire stent 4×20 was deployed into the M1 and M2 segments through the occlusion site for the purpose of temporary opening and thrombus removal. The occluded M1 segment was opened with stent-deployment. We waited several minutes, then, the stent was carefully retrieved after partial withdrawal into the Prowler microcatheter under applying negative pressure through the guiding catheter. During the passage of the distal ICA and siphon, some resistance was encountered. So, the endovascular neurosurgeon reinforced to retrieve the stent, meanwhile, the stent was detached unexpectedly. Following angiography revealed that the detached stent was located from cavernous segment to communicating segment of the ICA, and partial radiolucent area was contained within the distal part of the stent, which suggested the thrombus was captured at the area (Fig. 2C). Then, we tried to remove the detached stent using micro-snare and to open the occlusion with another attempt of forced suction thrombectomy, but failed to achieve recanalization with endovascular means. After declaration of endovascular failure, we first verified no significant increase in infarction size using repeated diffusion weighted image MRI. Then, we decided to perform surgical removal of the stent. The patient was operated on immediately under informed consent. The time spent on the endovascular procedure was 1 hour, and the time from the declaration of endovascular failure to the induction of general anesthesia in an operating room was 50 minutes.
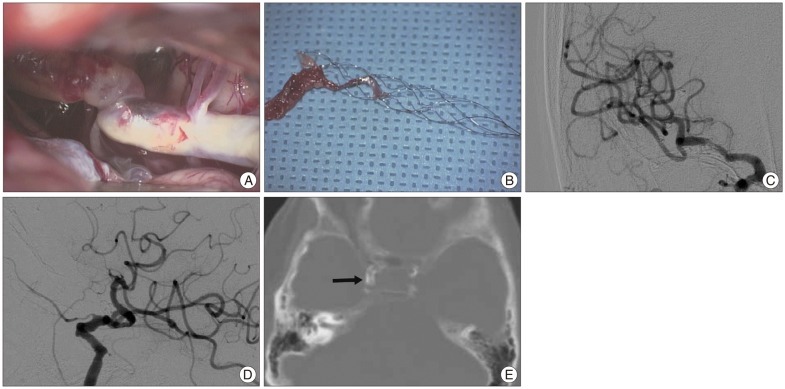
The patient underwent an extended superciliary approach as canvassed in a previous report by the present authors6). We first created a supraorbital craniotomy, and dissection of the proximal sylvian fissure revealed an intracranial ICA that was diffusely atherosclerotic and occluded with the Solitaire stent harboring the embolus (Fig. 3A). A part of superior wall of the ICA that was not atherosclerotic and contained the distal part of the stent was chosen for arteriotomy. A 5-mm longitudinal incision was required to remove the stent and associated embolus. The neurovascular surgeon first pulled the stent carefully but failed to remove, which was probably caused by some strut of the stent engaging a part of calcified lumen, then reinforced the pulling force resulted in successful removal of the stent finally. The stent grabbed the main thrombi at distal part of the stent and both proximal and distal markers of the stent were preserved (Fig. 3B). The arteriotomy site was repaired by a clip assisted micro-suture technique. Persistent arterial blood flow below the clip was ascertained with a microvascular Doppler. Postoperative angiography demonstrated complete recanalization of the ICA (Fig. 3C, D). The patient's neurological deficits improved, and the modified Rankin scale score was 2 at three months after surgery.
Based on the operative findings, the stent grabbed the main thrombi but was likely to fail to pass the acutely angled and circumferentially calcified ICA segment, and it finally detached inadvertently at the tortuous segment. Notably, bone window images of the baseline CT scan corresponded to the operative findings and showed severe and circumferential calcification at the supraclinoid ICA (arrow, Fig. 3E).
Among several mechanical thrombectomy techniques and devices, the Solitaire (self-expandable and fully retrievable) stent has several benefits, including possible immediate reperfusion in most patients after stent deployment and short procedure time. Hence, the reported clinical outcome of the Solitaire is promising2,5,7). However, the recanalization rate of Solitaire stent assisted thrombectomy cannot be 100%, and although rare, complications involving the stent are also possible. The present case is an example of a complication, reported elsewhere, involving the inadvertent detachment of the Solitaire stent4). In our case, we performed surgical removal of the stent including the thrombi grabbed within the stent, and we elucidated the reason why the inadvertent detachment occurred. Based on our experience, the detachable property, the most powerful benefit of the Solitaire, can harbor some risks in limited circumstances. If patients have anatomic features involving severely tortuous and acutely angled vessels coupled with circumferential calcification, some attention regarding difficult retrieval is required to prevent unexpected detachment.
It is notable that a baseline CT scan could have a potential role in anticipating this complication under those circumstances. In the present case, the surgical findings of a tortuous ICA with circumferential calcification corresponded to bone window images of the baseline CT scan (Fig. 3E). A baseline CT scan usually precedes an intraarterial procedure to screen for hemorrhagic stroke and/or intravenous rt-PA; therefore, we can easily obtain additional information related to the severity of preexisting atherosclerosis in a large artery. Also, if the findings are like the present case, more cautious retrieval is required to perform the Solitaire stent assisted technique and using another technique including forced suction thrombecotmy or intra-arterial chemical thrombolysis is also able to be considered.
However, the present case should be interpreted cautiously in several aspects. First, self-detachment of Solitaire stent can be caused by other reasons, for example, stent grabbed unusually large amount of thrombi and/or the problems of stent itself including the characteristics of detach zone or production process error. Second, ICA calcification is highly prevalent and can occur more than 50% on the CT scan1), therefore, the findings in this case can be regarded as additional information for minimizing the chance of such drastic complication if circumferential ICA calcifications coupled with severe tortuosity.
This study presents a case of inadvertent self-detachment of a Solitaire AB stent during mechanical thrombectomy involving a vessel with severe circumferential arteriosclerosis coupled with tortuous anatomy. Based upon our experience, some caution is required regarding difficult retrieval to prevent unexpected detachment in such circumstances. Additionally, we suggest that bone window images of a baseline CT scan can play a role in terms of anticipating difficult stent retrieval before the procedure.
References
1. Bos D, van der Rijk MJ, Geeraedts TE, Hofman A, Krestin GP, Witteman JC, et al. Intracranial carotid artery atherosclerosis: prevalence and risk factors in the general population. Stroke. 2012; 43:1878–1884. PMID: 22569939.
2. Castaño C, Dorado L, Guerrero C, Millán M, Gomis M, Perez de la Ossa N, et al. Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation: a pilot study. Stroke. 2010; 41:1836–1840. PMID: 20538693.

3. Kang DH, Hwang YH, Kim YS, Park J, Kwon O, Jung C. Direct thrombus retrieval using the reperfusion catheter of the penumbra system: forced-suction thrombectomy in acute ischemic stroke. AJNR Am J Neuroradiol. 2011; 32:283–287. PMID: 21087940.

4. Nayak S, Ladurner G, Killer M. Treatment of acute middle cerebral artery occlusion with a Solitaire AB stent: preliminary experience. Br J Radiol. 2010; 83:1017–1022. PMID: 21088087.

5. Park H, Hwang GJ, Jin SC, Bang JS, Oh CW, Kwon OK. Intra-arterial thrombolysis using double devices: mechanicomechanical or chemicomechanical techniques. J Korean Neurosurg Soc. 2012; 51:75–80. PMID: 22500197.

6. Park J, Hwang YH, Kim Y. Extended superciliary approach for middle cerebral artery embolectomy after unsuccessful endovascular recanalization therapy: technical note. Neurosurgery. 2009; 65:E1191–E1194. discussion E1194. PMID: 19934937.
7. Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012; 380:1241–1249. PMID: 22932715.

Fig. 1
Baseline images of the patient including (A) CT scan, (B) diffusion-weighted image MRI, and (C) mean transit time map of MRI are showing.
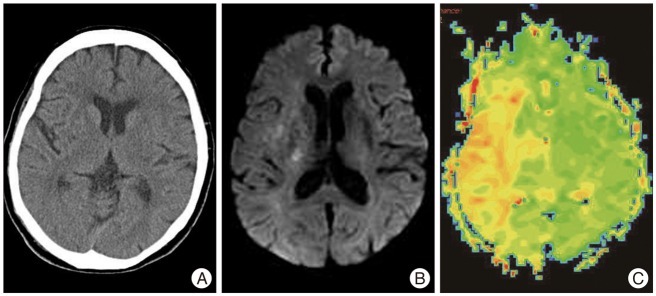
Fig. 2
A: Angiography shows occlusion at cavernous segment of the internal carotid artery on the right. B: A-P angiography shows that Solitaire AB stent is used as a temporary bypass for the remaining middle cerebral artery occlusion after recanalization of the ICA. C: Final lateral angiography shows inadvertent detachment of the stent and the remaining distal ICA occlusion. ICA: internal carotid artery.
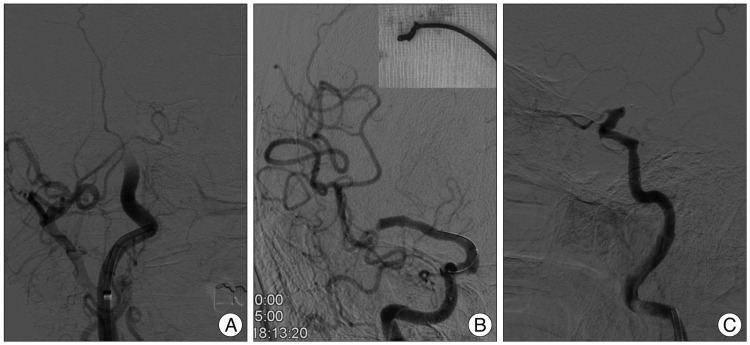
Fig. 3
Surgical finding of the acutely angled and circumferentially calcified distal ICA (A) before arteriotomy is showing. Surgically removed Solitaire AB stent is containing the main thrombi at the distal part of the stent strut (B). A-P and lateral angiography immediately after surgery is showing full recanalization of the occlusion (C and D). Bone window image of a baseline CT scan shows severely and circumferentially calcified supraclinoid segment of the ICA (arrow), which corresponds to the surgical finding (E). ICA: internal carotid artery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download