Abstract
Objective
We analyzed the clinical and radiologic features of posterior apophyseal ring separation (PARS) with lumbar disc herniation and suggest the proper management options according to the PARS characteristics.
Methods
We reviewed case series of patients with PARS who underwent surgery of lumbar disc herniation. Preoperative symptoms, neurologic status, Body Mass Index, preoperative and postoperative Visual Analogue Scale (VAS) and Korean-Oswestry Disability Index (K-ODI) scores, operation types were obtained. PARS size, locations, the degree of resection were assessed.
Results
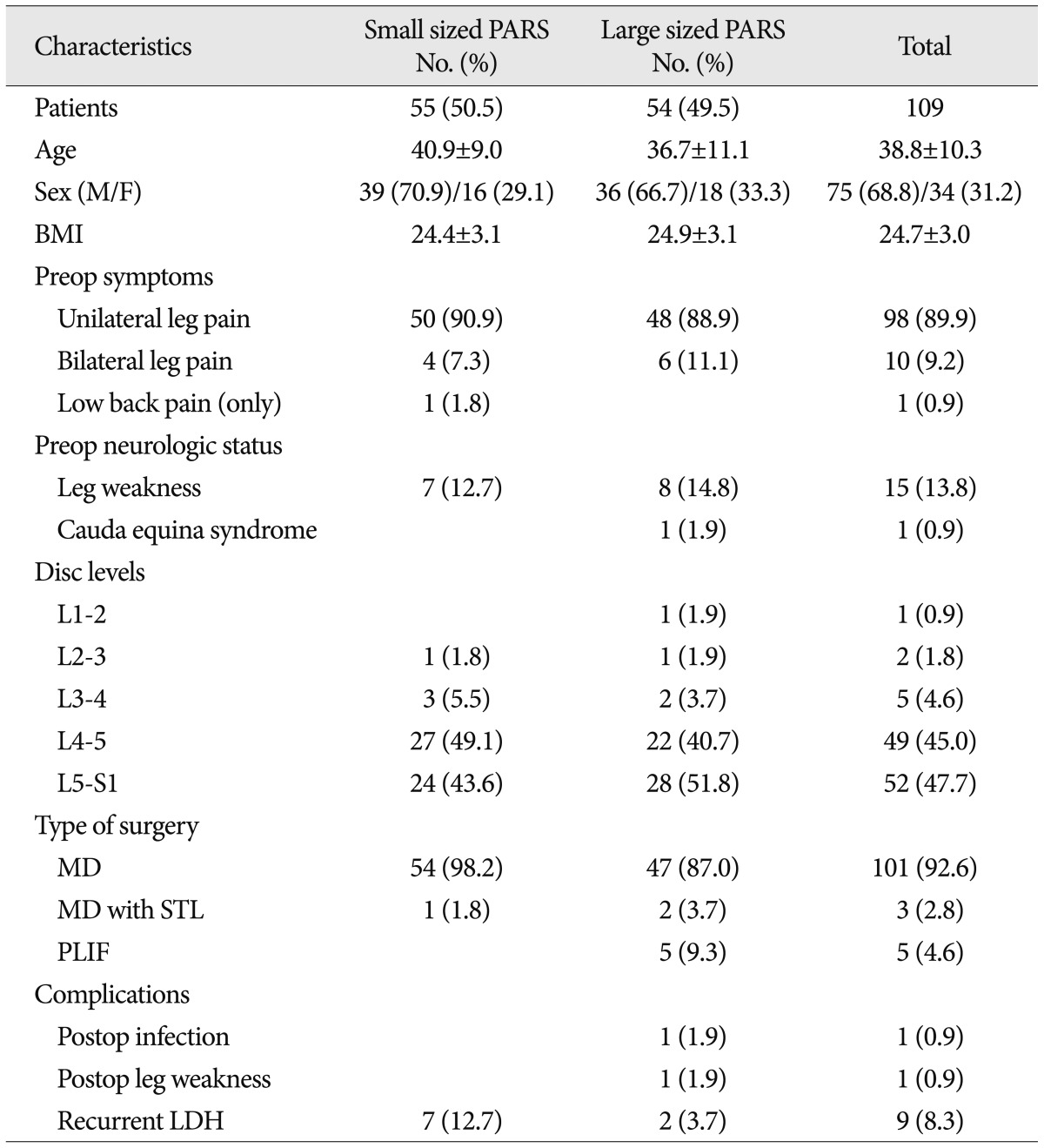
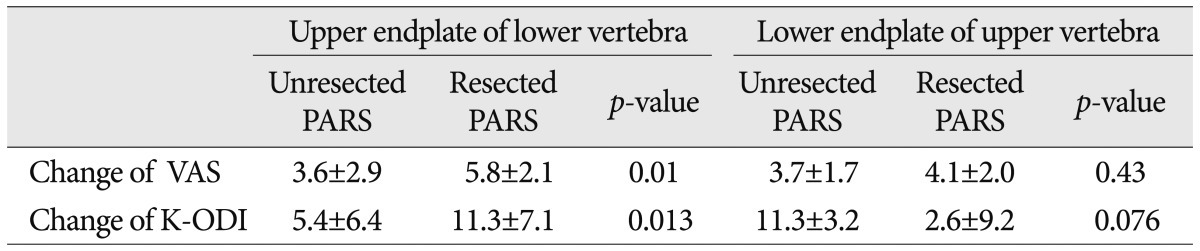
PARS was diagnosed in 109 (7.5%) patients among 1448 patients given surgical treatment for single level lumbar disc herniation. There were 55 (50.5%) small PARS and 54 (49.5%) large PARS. Among the large PARS group, 15 (27.8%) had lower endplate PARS of upper vertebra at the level of disc herniation. Thirty-nine (72.2%) were upper endplate PARS of lower vertebra. Among the group with upper endplate PARS of lower vertebra, unresected PARS was diagnosed in 12 (30.8%) cases and resected PARS was diagnosed in 27 (69.2%) cases. VAS and K-ODI scores changes were 3.6±2.9 and 5.4±6.4 in the unresected PARS group, 5.8±2.1 and 11.3±7.1 in the resected PARS group. The group with upper endplate PARS of lower vertebra showed significant difference of VAS (p=0.01) and K-ODI (p=0.013) score changes between unresected and resected PARS groups.
Lumbar posterior apophyseal ring separation (PARS) combined with disc herniation is uncommon. It has been called by variety names including "vertebral limbus fracture", "posterior extramarginal disc herniation", "vertebral endplate separation" and "posterior Schmorl node"1,10-12). There are some controversies whether to remove PARS concomitantly when discectomy is done. Epstein and Epstein11) suggested surgical excision of the fractured ring apophysis when neurologic deficit existed. Otherwise, another author reported comparable satisfactory results in cases that had discectomy with or without excision of PARS19). The type of surgery that is most appropriate for patients with PARS lesion also has been a matter of controversy. Takata et al.21) emphasized that most small PARS was mobile and mandatory to remove. Many other authors also proposed that small and mobile PARS should be removed1,19,21). Large PARS still remained problematic whether to remove or not. Therefore, we analyzed the clinical and radiologic features of PARS with lumbar disc herniation, especially large PARS and suggested proper management options according to the PARS characteristics.
We reviewed 109 patients (109 levels) with PARS associated with lumbar disc herniation who underwent surgery in the author's hospital between December 2006 and November 2008. Severe spinal stenosis, spondylolysis, spinal infection, systemic diseases that affect bone and joint, and revision operation cases were excluded.
Through the medical records, we checked the preoperative symptoms, neurologic examination, Visual Analogue Scale (VAS), Korean-Oswestry Disability Index (K-ODI), Body Mass Index (BMI) and underlying disease. Preoperative computed tomogram (CT) and magnetic resonance imaging (MRI) were obtained from all the patients. PARS lesions were classified by location (lower endplate of upper vertebra or upper endplate of lower vertebra at the level of disc herniation, central or lateral location in the spinal canal) and size (small or large, defined by 50% width of spinal canal6)). If PARS lesions were smaller than 50% width of spinal canal and located at central canal area, those were classified with small central PARS (Fig. 1A). If small PARS lesions were located at lateral recess zone, those were classified with small lateral PARS (Fig. 1B). Unilateral lateral recess zone involved PARS lesions with larger than 50% width of spinal canal were defined by large unilateral PARS (Fig. 1C), only central canal involved large PARS lesions were classified with large central PARS (Fig. 1D), and bilateral lateral recess zone involved large PARS lesions were classified with large bilateral PARS (Fig. 1E).
We reviewed surgical records to assess the occurrence of intraoperative complications. Outcome measures were defined by the change of large PARS patients' VAS and K-ODI between pre and postoperation. The degree of PARS removal was checked through the postoperative imaging studies. Resected PARS group included total resection of PARS lesion.
The statistical analyses were conducted using SPSS 12.0 for Windows (SPSS, Inc., Chicago, IL, USA). Numerical variables were expressed as the mean±standard error of the mean. Student's t-test, Mann-Whitney U test and Pearson correlation coefficients were calculated. Null hypotheses of no difference were rejected if p-value were less than 0.05.
There were 1448 patients given the surgery for single level lumbar disc herniation in the author's hospital between December 2006 and November 2008. PARS was diagnosed in 109 (7.5%) of 1448 patients given the surgical treatment for lumbar disc herniation (Table 1). Small PARS was 55 (50.5%) and large PARS was 54 (49.5%). The PARS group was composed of 75 (68.8%) males and 34 (31.2%) females. The mean age of patients was 38.8±10.3 years old. The mean BMI was 24.7±3.0 (In Asia, BMI of 18.5 to 22.9 indicates optimum weight; BMI above 23 indicates the person is overweight; a number above 25 indicates the person is obese20)). All the PARS patients had lower back and leg pain, except one with severe low back pain. Ten (9.2%) patients showed bilateral leg pain symptoms. Fifteen (13.8%) patients had unilateral leg weakness and 1 (0.9%) patient had bilateral leg weakness. One patient presented with right side foot drop and cauda equina syndrome (L4/5 level, large PARS with huge ruptured disc herniation). Five patients suffered from pulmonary tuberculosis, 11 had hypertension past history. Three patients had diabetes mellitus and one was hepatitis B carrier.
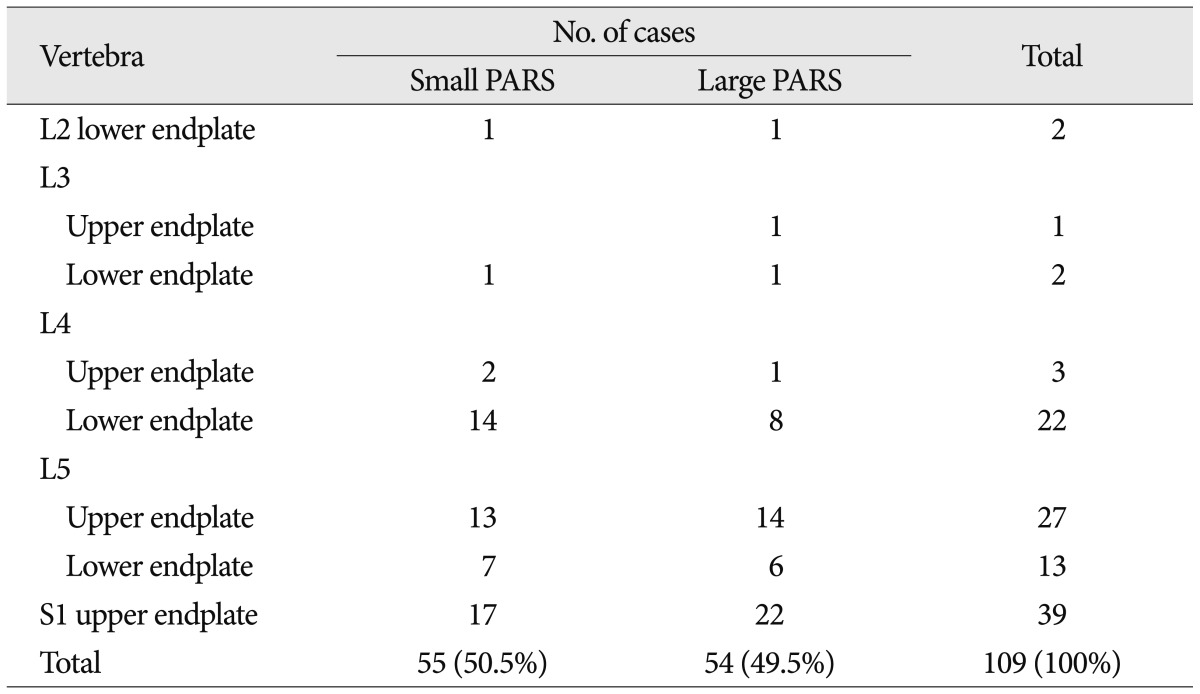
All 109 patients underwent CT, MRI studies before the surgery. PARS and lumbar disc herniation were at the same level. The most common level was L5-S1 (52 cases, 47.7%) followed by L4-5 (49 cases, 45.0%) (Table 2). The upper endplate of S1 was the most common involved site (39 patients, 35.8%). The second most common site was L5 upper endplate (27 patients, 24.8%) followed by L4 lower endplate (22 patients, 20.2%). Thirty eight (34.9%) were lower endplate PARS of upper vertebra at the level of disc herniation. Seventy one (65.1%) had upper endplate PARS of lower vertebra. Central located small PARS were 27 (24.8%) and lateral side located small PARS was 28 (25.7%). Unilateral side located large PARS was 40 (36.7%), central was 10 (9.2%) and bilateral side involved PARS was 4 cases (3.6%). Microscopic lumbar discectomy was performed in 101 (92.7%) patients, decompressive subtotal laminectomy with microscopic discectomy was performed in 3 (2.7%) patients (two L2-3 levels and one L3-4 level) and total laminectomy with posterior lumbar interbody fusion operation was done in 5 (4.6%) patients (L1-2; 1 case, L4-5; 4 cases).
There were two complications, postoperatively. One was postoperative immediate leg weakness which resolved after about 6 months. The other was postoperative infection which was controlled two months later. Recurrent disc herniation occurred in 9 patients, between 6 months and 48 months later.
In the large PARS group with lumbar disc herniation, partial PARS resection was done in 10 (18.5%) patients and total resection was performed in 25 (46.3%). In 19 (35.2%) patients, PARS lesion was not resected. Preoperative mean VAS and K-ODI were 7.0±1.9 and 20.9±8.1. Postoperative mean VAS was 2.4±1.8 and K-ODI was 12.6±7.2. Among the group with lower endplate PARS of upper vertebra at the disc level (15 patients), unresected PARS after the surgery was 7 (46.7%) cases and resected PARS was 8 (53.3%). VAS and K-ODI score changes between pre and post operation were 3.7±1.7 and 11.3±3.2 in unresected PARS group, 4.1±2.0 and 2.6±9.2 in resected PARS group. Among the group with upper endplate PARS of lower vertebra (39 patients), unresected PARS was 12 (30.8%) cases and resected PARS was 27 (69.2%). VAS and K-ODI scores changes were 3.6±2.9 and 5.4±6.4 in the unresected PARS group, 5.8±2.1 and 11.3±7.1 in the group with resected PARS. There was no significant difference of upper body lower endplate PARS group's VAS and K-ODI score changes between unresected and resected PARS groups. Otherwise, the group with upper endplate PARS of lower vertebra showed significant difference of VAS (p=0.01) and K-ODI (p=0.013) score changes between unresected and resected PARS groups (Table 3).
Many studies reported that posterior ring apophysis separation occurs in children and adolescents mainly, because of the process of apophyseal ring formation6,17,19). Ossification of ring apophysis occurs at 6-9 years and ossified apophysis fuses with vertebral body at about 17 years and completely at about 20 years5). This attachment between posterior ring apophysis and vertebral body is relatively weak point until osseous union is complete, so that lumbar disc herniation may be associated with posterior apophyseal ring separation after acute or chronic trauma in children and adolescents4,5,10,22). Yen et al.24) reported a strong association of adolescent apophyseal ring fracture with overweight and obesity. We checked the BMI of the case series and found a negative correlation between age and BMI by using Pearson correlation coefficients (Pearson coefficient : -0.22, p=0.022). Two groups (younger than 30 years old patients, older than 30 years old or 30 years old patients) showed significantly different BMI (p=0.016). That also means the PARS of adolescent and young adult are more associated with BMI than the PARS of old adults. But this needs a more advanced statistical analysis to determine whether high BMI is a factor in adolescent PARS. However, we could focus on the possibility of a strong association between overweight or obesity and adolescent's posterior ring apophysis separation with lumbar disc herniation in our study.
Yang et al.23) reported that the prevalence of posterior ring apophysis separation associated with lumbar disc herniation was 5.7% among all age patients. Akhaddar et al.1) reported 5.35% in the adult patients. Otherwise, in children and adolescents, a high prevalence (19-42%) was reported compared with adults3,6-8,19). In our study, we found 7.5% incidence among all age patients. This relatively high incidence may be contributed to various neuroradiologic diagnostic tools (CT and MRI). CT scanning in particular could detect very small sized posterior ring apophysis separations15). Appropriately angled CT scans can show exact information about the site, size and shape of the bony fragment13,24). Akhaddar et al.1) suggested that CT scanning with sagittal reconstructions is the procedure of choice for diagnosis. We also agree that it is necessary to evaluate CT scans prior to surgery for lumbar disc herniation, because CT scan with sagittal reconstruction is very helpful to detect the accurate location of PARS and to differentiate PARS with other calcified lesion.
Some authors reported that L4/5 level was the most common level involving PARS with lumbar disc herniation in adolescents, and either L4/5 or L5/S1 in young adults9,14,16,21). Others reported that PARS occurred in L5/S1 level most commonly and S1 superior endplate was the most common affected lesion1,6,19). Our study also showed that L5/S1 level and S1 upper endplate were the most commonly affected level and endplate lesion. According to our study and others1,6,18), the upper endplate of the posterior vertebral body is more affected than the lower endplate, probably because it is most stressed from a functional point of view17).
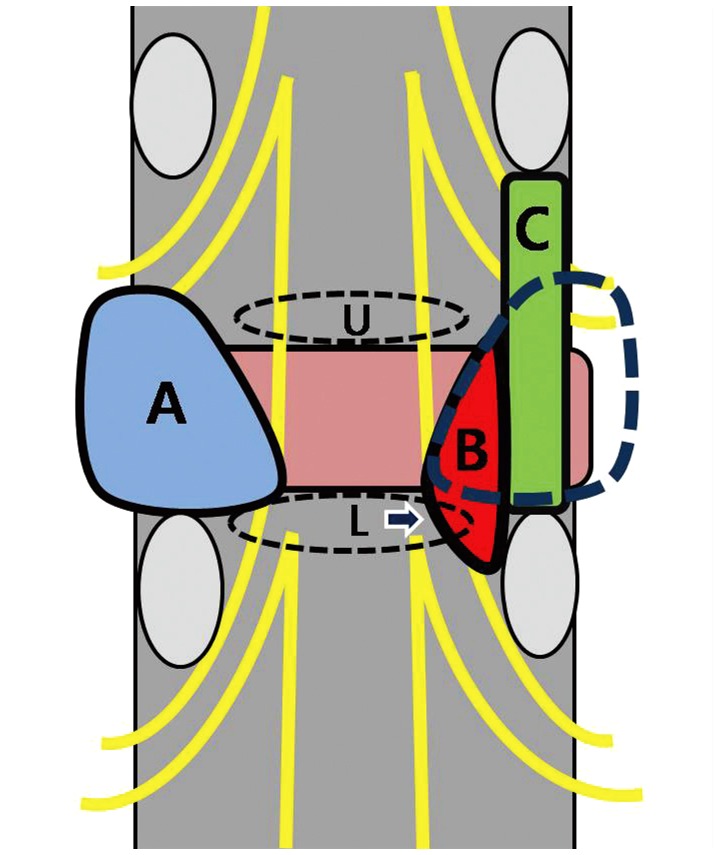
Takata et al.21) classified ring apophysis fracture into 3 types based on computed tomography : Type I fracture consist of a small arcuate fragment (pure avulsions of the posterior cortical vertebral margin) in the spinal canal with no attendant osseous defect of the vertebral body. Type II lesions comprised larger central fractures which included parts of the cortical and cancellous bony rim. Type III is a small localized fracture with a round defect in the end-plate (teardrop-shaped fracture). Epstein et al.12) have added a type IV limbus fracture involving the full axial length of the posterior margin of the vertebral body. Others classified posterior ring apophysis separation by the mobility of bony fragment1,19). They recommend that resection of a fragment during the discectomy may be needed when a fragment is mobile, because disc herniation and a simultaneous occurring mobile fragment are the main pathology of acute-onset sciatica. And others1,19,21) propose that small size posterior ring fracture correlated disc herniation should be removed because that is almost mobile and simultaneously occurs with the disc herniation and causes acute-onset pain. In our study, small PARS was also teardrop-shaped and correlated with disc herniation mostly. Therefore, we thought that small PARS removal correlated with disc herniation was mandatory, but large PARS still remains controversial. We also analyzed the surgical outcomes of large PARS according to the location and found a significant result that the upper endplate large separation of lower vertebra should be removed for satisfactory results. We postulated that large PARS of upper endplate in lower vertebra could compress the nerve root more easily than the lower endplate of upper vertebra. It is because that most nerve roots of lumbar spine usually originate near the upper endplate of lower vertebra from the thecal sac and upper endplate of lower vertebra is associated with lateral recess zone, so large PARS of upper endplate in lower vertebra makes lateral recess stenosis and compresses the nerve root more easily (Fig. 2).
Some authors2,5,18) suggested posterolateral arthrodesis to avoid secondary instability. In the high lumbar levels (L1/2, 2/3), our three patients were given extensive laminectomy and one (L1/2 level) was performed posterior lumbar interbody fusion procedure. Four other patients (L4/5 level) underwent posterior lumbar interbody arthrodesis because they presented with bilateral sciatica so needed extensive laminectomy and facetectomy to be able to occur postoperative instability. All of them showed good results and there were no complications postoperatively. Thus, we propose that high lumbar level lesion or bilateral side involved lesion associated with PARS has to be widely decompressed and arthrodesis procedure should be used, if needed. But, we need a larger patient series with-long term follow up period and a prospective randomized study to validate our results. Further studies are necessary to establish proper surgical tools according to the various characteristics of lumbar disc herniation associated with posterior ring apophysis separation.
Small PARS related to disc herniation was mandatory to be removed. Large PARS of upper endplate in lower vertebra should be resected during the surgery of lumbar disc herniation, as well. Otherwise, the PARS resection of lower endplate in upper vertebra associated with lumbar disc herniation is not always needed. High level of lumbar lesion or bilateral side involved lesion associated PARS should be widely decompressed and if there is a possibility of secondary instability, arthrodesis procedures are necessary.
References
1. Akhaddar A, Belfquih H, Oukabli M, Boucetta M. Posterior ring apophysis separation combined with lumbar disc herniation in adults : a 10-year experience in the surgical management of 87 cases. J Neurosurg Spine. 2011; 14:475–483. PMID: 21294611.

2. Asazuma T, Nobuta M, Sato M, Yamagishi M, Fujikawa K. Lumbar disc herniation associated with separation of the posterior ring apophysis: analysis of five surgical cases and review of the literature. Acta Neurochir (Wien). 2003; 145:461–466. discussion 466. PMID: 12836070.

3. Banerian KG, Wang AM, Samberg LC, Kerr HH, Wesolowski DP. Association of vertebral end plate fracture with pediatric lumbar intervertebral disk herniation : value of CT and MR imaging. Radiology. 1990; 177:763–765. PMID: 2243985.

4. Baranto A, Ekström L, Hellström M, Lundin O, Holm S, Swärd L. Fracture patterns of the adolescent porcine spine : an experimental loading study in bending-compression. Spine (Phila Pa 1976). 2005; 30:75–82. PMID: 15626985.

5. Bick EM, Coper JW. The ring apophysis of the human vertebra; contribution to human osteogeny. II. J Bone Joint Surg Am. 1951; 33-A:783–787. PMID: 14850517.
6. Chang CH, Lee ZL, Chen WJ, Tan CF, Chen LH. Clinical significance of ring apophysis fracture in adolescent lumbar disc herniation. Spine (Phila Pa 1976). 2008; 33:1750–1754. PMID: 18628708.

7. Chen LH, Chang CH, Lee ZL, Niu CC, Lai PL, Tan CF, et al. Intervertebral disc herniation in adolescents. Chang Gung Med J. 2004; 27:22–28. PMID: 15074886.
8. Cheon MH, Lee MK, Kim DH, Kim HH, Kim DJ. Clinical analysis of posterior lymbar apophyseal ring fractures in young adults. J Korean Neurosurg Soc. 1996; 25:1964–1969.
9. Dake MD, Jacobs RP, Margolin FR. Computed tomography of posterior lumbar apophyseal ring fractures. J Comput Assist Tomogr. 1985; 9:730–732. PMID: 3160730.

10. Edelson JG, Nathan H. Stages in the natural history of the vertebral end-plates. Spine (Phila Pa 1976). 1988; 13:21–26. PMID: 3381133.

11. Epstein NE, Epstein JA. Limbus lumbar vertebral fractures in 27 adolescents and adults. Spine (Phila Pa 1976). 1991; 16:962–966. PMID: 1948383.

12. Epstein NE, Epstein JA, Mauri T. Treatment of fractures of the vertebral limbus and spinal stenosis in five adolescents and five adults. Neurosurgery. 1989; 24:595–604. PMID: 2710305.

13. Gomori JM, Floman Y, Liebergall M. CT of adult lumbar disc herniations mimicking posterior apophyseal ring fractures. Neuroradiology. 1991; 33:414–418. PMID: 1749472.

14. Handel SF, Twiford TW Jr, Reigel DH, Kaufman HH. Posterior lumbar apophyseal fractures. Radiology. 1979; 130:629–633. PMID: 424528.

15. Kaiser MC, Capesius P, Veiga-Pires JA, Sandt G. A sign of lumbar disk herniation recognizable on lateral CT generated digital radiograms. J Comput Assist Tomogr. 1984; 8:1066–1071. PMID: 6238982.

16. Leroux JL, Fuentes JM, Baixas P, Benezech J, Chertok P, Blotman F. Lumbar posterior marginal node (LPMN) in adults. Report of fifteen cases. Spine (Phila Pa 1976). 1992; 17:1505–1508. PMID: 1471010.
17. Martínez-Lage JF, Poza M, Arcas P. Avulsed lumbar vertebral rim plate in an adolescent : trauma or malformation? Childs Nerv Syst. 1998; 14:131–134. PMID: 9579870.

18. Savini R, Di Silvestre M, Gargiulo G, Picci P. Posterior lumbar apophyseal fractures. Spine (Phila Pa 1976). 1991; 16:1118–1123. PMID: 1948402.

19. Shirado O, Yamazaki Y, Takeda N, Minami A. Lumbar disc herniation associated with separation of the ring apophysis : is removal of the detached apophyses mandatory to achieve satisfactory results? Clin Orthop Relat Res. 2005; 120–128. PMID: 15685064.
20. Shiwaku K, Anuurad E, Enkhmaa B, Nogi A, Kitajima K, Shimono K, et al. Overweight Japanese with body mass indexes of 23.0-24.9 have higher risks for obesity-associated disorders : a comparison of Japanese and Mongolians. Int J Obes Relat Metab Disord. 2004; 28:152–158. PMID: 14557832.

21. Takata K, Inoue S, Takahashi K, Ohtsuka Y. Fracture of the posterior margin of a lumbar vertebral body. J Bone Joint Surg Am. 1988; 70:589–594. PMID: 3356726.

22. Tamano K, Shinohara K, Mikami H. A clinical study of displaced ring apophysis. J C-S Orthop Assoc. 1994; 6:431–433.
23. Yang IK, Bahk YW, Choi KH, Paik MW, Shinn KS. Posterior lumbar apophyseal ring fractures : a report of 20 cases. Neuroradiology. 1994; 36:453–455. PMID: 7991090.

24. Yen CH, Chan SK, Ho YF, Mak KH. Posterior lumbar apophyseal ring fractures in adolescents : a report of four cases. J Orthop Surg (Hong Kong). 2009; 17:85–89. PMID: 19398801.

Fig. 1
PARS classification by the size and location. A : Small central PARS. B : Small lateral side PARS. C : Large unilateral located PARS. D : Large central PARS. E : Large bilateral involved PARS. PARS : posterior apophyseal ring separation.
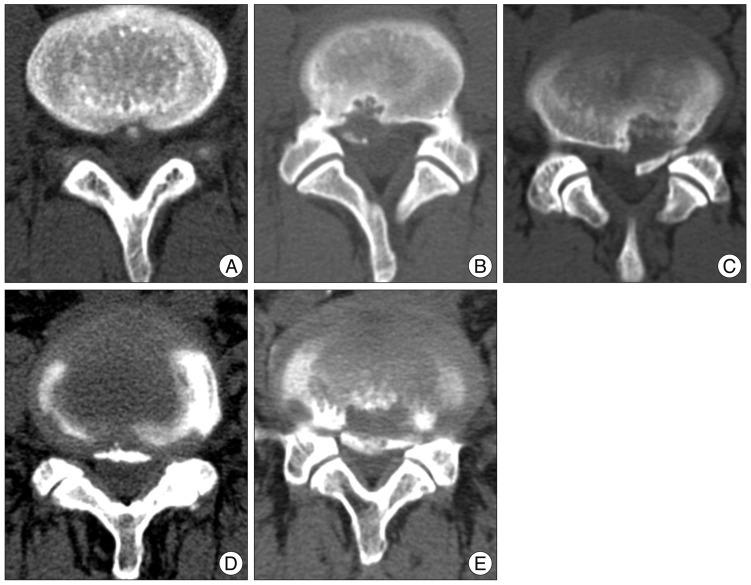
Fig. 2
The schematic figure shows the anatomical relationship between lateral recess zone and endplate separation of lower body endplate. The root is compressed more easily at the lower body endplate area rather than upper body endplate area. A and blue dotted line : superior facet of lower body, B : lateral recess zone, C : inter vertebral foramen, U : the zone of upper body endplate separation, L : the zone of lower body endplate separation, Arrow : the point of root origination from thecal sac.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download