Abstract
Objective
This retrospective study aimed to compare clinical outcomes in terms of pain relief and recurrence rate between fragmentectomies and conventional microdiscectomies in patients with lumbar disc herniation (LDH).
Methods
Between January 2008 and May 2011, a total of 175 patients met the inclusion criteria of this study. The visual analogue scale (VAS) scores of back and radicular pains were recorded before surgery, 2 and 6 weeks after surgery. Recurrence was defined when a patient had the same pattern of preoperative symptoms and was confirmed with magnetic resonance imaging.
Results
Seventy-four patients (42.3%) were suitable for fragmentectomy, and 101 patients underwent conventional microdiscectomy. There were no significant differences in VAS scores between the fragmentectomy and conventional microdiscectomy groups 2 and 6 weeks after surgery. During the follow-up period, 3 patients (4.05%) in the fragmentectomy group and 7 patients (6.93%) in the conventional microdiscectomy group relapsed.
In 1977 Caspar5) and Yasargil20) introduced an interlaminar approach with partial resection of bony structures and the ligamentum flavum followed by the removal of the intervertebral disc materials6). Since then, various techniques have been developed for the treatment of lumbar disc herniation (LDH), but most patients still undergo the conventional microdiscectomy2). Surgeons, who perform the conventional microdiscectomy, take into consideration the fact that degenerative disc materials left in the intervertebral disc space have a high incidence of reherniation14,15). Thus, surgeons have tried to remove as much disc materials as possible from the intervertebral disc space17). However, there is no definite criteria for the extent of disc materials which should be removed. Furthermore, aggressive discectomy often causes postoperative loss of disc height with subsequent loosening of ligaments and articular capsules11,12). This may result in segmental instability and thus accelerate spondylosis, which contributes to a significant proportion of failed back surgery syndrome after lumbar microdiscectomy1,6,7,14,15,17). For these reasons, in 1978, Williams19) proposed a conservative microsurgical approach to virgin herniated lumbar discs by making only a blunt perforation in the fibrous annular ring without an incision or curettage of the disc space. Tissue from the intervertebral disc space should be removed with only a small pituitary forcept without curettage of the disc space. Since then, there have been some reports regarding the use of the sequestrectomy, fragmentectomy, or limited microdiscectomy instead of the conventional microdisectomy. Though several terms are available to describe the procedure, fragmentectomy may be the most accurate expression. Conservative microdiscectomy is usually carried out for free-fragment LDH, which is sequestrated from the defect of the posterior longitudinal ligament (PLL). However, fragmentectomy can also be performed in the contained-fragment LDH which has intact PLL without sequestration18). The difference between the fragmentectomy and conventional microdiscectomy is the removal or preservation of normal disc materials apart from already extruded discs. Fragmentectomy showed good success rates of greater than 90%, according to some studies7,14,16). However, such results cause spinal surgeons to debate whether recurrent disc herniation would increase after fragmenectomy6). Therefore, this retrospective study was conducted to compare the clinical outcomes of fragmentectomy and conventional microdiscectomy in patients with single-level LDH in terms of pain relief and recurrence rate.
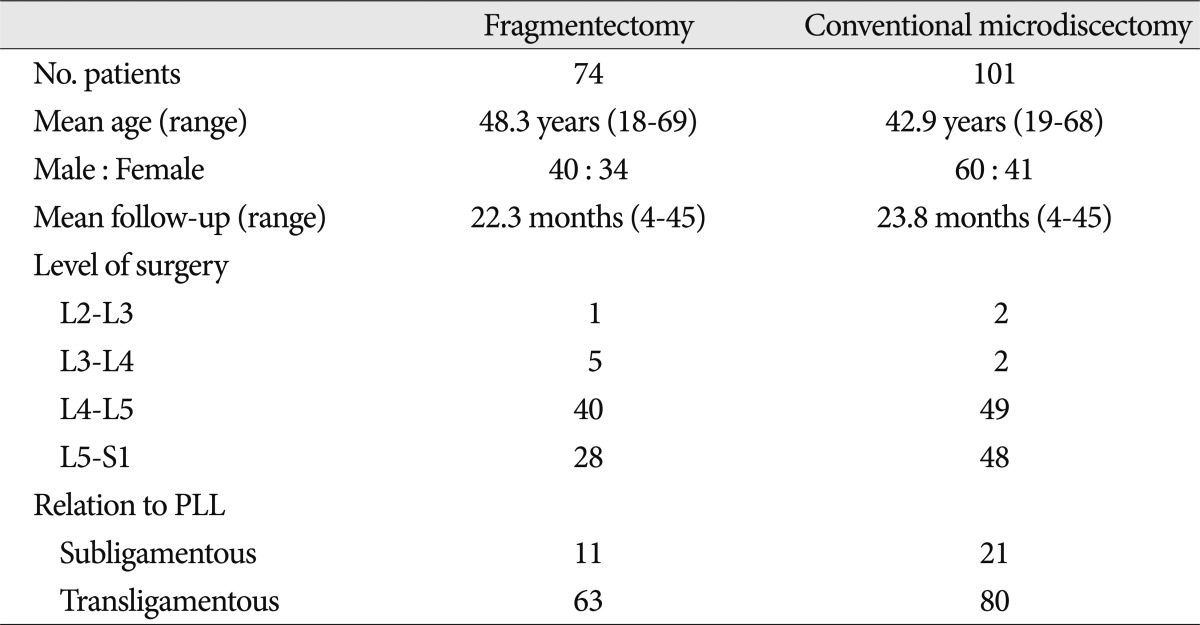
Between January 2008 and May 2011, a total of 397 consecutive patients underwent single-level lumbar microdiscectomy by the same surgeon at our institute. Of these patients, 175 met the inclusion criteria of our study having undergone either fragmentectomy or conventional microdiscectomy (Table 1).
This study included patients who had unilateral single-level canalicular LDH from L2 through S1 and whose radiographic confirmation of LDH corresponded to clinical signs and symptoms refractory to conservative treatment. Patients with free fragments as well as those with subligamentous herniation and transannular herniation were also included. Patients were excluded if they had 1) histories of previous lumbar spinal operations at any level, 2) foraminal or extraforaminal LDH, 3) bulging discs which were treated with bipolar thermocoagulation, 4) combined spinal instability, and 5) postoperative infections or hematomas.
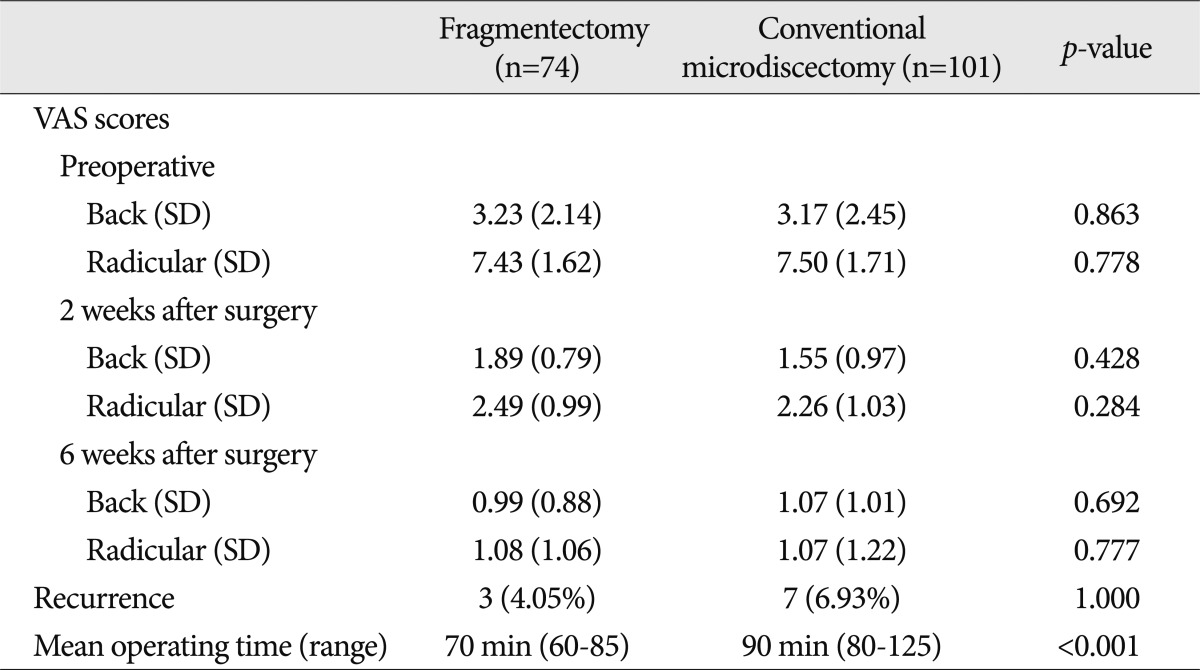
The visual analogue scale (VAS) scores of back and radicular pains were recorded before surgery, 2 and 6 weeks after surgery (Table 2). Although the mean follow-up duration was 23 months (range, 4-45 months), we did not include the VAS scores at the last follow-up in order to eliminate the influence of patients' environmental factors, especially occupational activities after the recuperation period.
The operating time from skin incision to skin closure was recorded for each patient. Recurrence was defined when a patient had the same pattern of preoperative symptoms and was confirmed with magnetic resonance imaging (MRI).
Decisive factors for performing either a fragmentectomy or conventional microdiscectomy were 1) the size of fibrous annular ring defect which was measured by a hook with 5-mm tip, 2) the presence of additional extrusion of nuclear materials during subannular probing with a hook, and 3) the stability of the fibrous annular ring, which was estimated by pressing against the PLL around the tear site with a hook. If there was no additional extrusion during compression, the fibrous annular ring was considered stable. These factors were examined not only in the lumbar kyphotic position with the Wilson frame but also in the lordotic position by releasing the Wilson frame and were identified repeatedly during the surgery. If the fibrous annular ring defect was less than 5 mm and there was no additional extrusion of nuclear materials from the annular defect during the compression of the PLL and subannular probing with a hook, we performed fragmentectomy. In case of subligamentous ruptured disc, we made an opening in the PLL with a laser (30C CO2 laser, Sharplan, FL, USA) and performed a fragmentectomy. Not in case of diffuse bulging discs which were treated with bipolar thermocoagulation, subligamentous ruptured discs had the detached disc fragments almost always. If no detached disc fragment was found through the PLL opening, the bulging area beneath the traversing nerve root was removed by piecemeal fashion, creating a large iatrogenic annulotomy.
The SPSS software package, version 12.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses of the data.
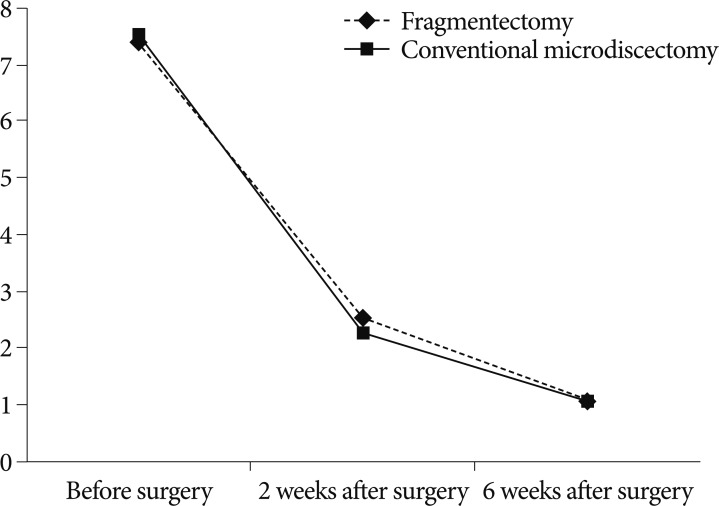
Of the 175 patients who satisfied the study design, 74 (42.3%) were suitable for fragmentectomy and 101 (57.7%) underwent conventional microdiscectomy. The mean age of the patients was slightly older in the fragmentectomy group than in the conventional microdiscectomy group (Table 1). The mean postoperative follow-up durations of the fragmentecomy and conventional microdiscectomy groups were 22.3 and 23.8 months, respectively (range, 4-45 months). The most frequent level of surgery was L4/5 in both groups. The proportion of the subligamentous type to the transligamentous type was 14.9% (11 of 74) in the fragmentectomy group and 20.7% (21 of 101) in the conventional microdiscectomy group. The mean VAS scores of back and radicular pains before surgery were 3.23 and 7.43, respectively, in the fragmentectomy group and 3.17 and 7.50, respectively, in the conventional microdiscectomy group. There were no significant differences between the 2 groups (p=0.863, p=0.778; t-test). At 2 weeks, the mean postoperative VAS scores of back and radicular pains in the fragmentectomy group were 1.89 and 2.49, respectively, and improved to 0.99 and 1.08, respectively, at 6 weeks. In the conventional microdiscectomy group, the mean VAS scores of back and radicular pains after surgery were 1.55 and 2.26, respectively, at 2 weeks, and improved to 1.07 and 1.07, respectively, at 6 weeks. There were no significant differences between the 2 groups in relief of back and radicular pains at 2 postoperative weeks (p=0.428 for back pain, p=0.284 for radicular pain) and 6 postoperative weeks (p=0.692 for back pain, p=0.777 for radicular pain). The 2 surgical methods were found to be similarly effective in pain relief (Fig. 1, 2).
During the follow-up period, 3 patients (4.05%) in the fragmentectomy group and 7 patients (6.93%) in the conventional microdiscectomy group relapsed (Table 2). Recurrence was defined as recurrent LDH at the same site of back or radicular pain as confirmed by MRI. All patients with recurrent LDH underwent revision surgery due to persistent pain despite the conservative treatment.
The mean operation times were 70 minutes (range, 60-85 minutes) in the fragmentectomy group and 90 minutes (range, 80-125 minutes) in the conventional microdiscectomy group. Because the disc space was not evacuated, the operation time for fragmentectomy was significantly reduced (p<0.001).
Traditionally, microdiscectomy-related neural decompression is conducted by excision of the herniated disc material, resection of as much disc materials as possible, and curettage of the endplates5,15). However, the amount of disc material which needs to be removed has been called into question. In fact, it is difficult to identify a distinct border between the rigid annulus fibrosus and the soft nucleus pulposus. Visualization of and instrument accessibility to the intervertebral disc space are limited. Furthermore, there is the possibility of the failed back syndrome related to diminished disc height1,6,7,14,15,17). Thus, we attempted to remove the normal disc materials as little as possible and eventually performed only fragmentectomy. If recurrence rates are not higher in the fragmentectomy group than in the conventional microdiscectomy group, fragmentectomy will show good results on account of maintaining the disc height. In line with this thinking, several neurosurgeons, including Williams19) have performed fragmentectomy according to their own criteria. Kast et al.9) performed fragmentectomies when the fibrous ring was stable without obvious bulging as measured by pressing against the fibrous ring with a dissector. They also reported that patients with stable fibrous rings and small defects (3 mm or less) had a good success rate. Fakouri et al.6) reported successful sequestrectomy in patients who met their inclusion criteria : the free disc fragment was localized posterior to the PLL and the annular tear was up to 5 mm without significant bulging of the disc. This decision was made intraoperatively by assessing the integrity of the annulus fibrosus and the PLL, but the determinations were very subjective and dependent on each surgeon's experience. We performed fragmentectomies in patients who had a defect of the fibrous annular ring less than 5 mm and no additional extrusion of nuclear materials from the annular defect during the compression of the PLL and during subannular probing with a hook. Based on our results, it is thought that the defect size of the annular band is more important than that of the PLL. Carragee et al.3,4) reported that since a large annular defect measuring >6 mm resulted in a recurrence rate of 27.3%, such annular defects should require more aggressive discectomies. In our study, fragmentectomies were performed on patients with defects of the fibrous annular ring measuring less than 5 mm. Additionally, the annular defect was assessed by compression of the PLL around the annular defect site not only in the lumbar kyphotic position with the Wilson frame but also in the lordotic position by releasing the Wilson frame. Our method has not been introduced yet in previous studies of fragmentectomy. We were able to identify the additional extrusion of disc materials which has not been fully verified in the lumbar kyphotic position at initial operation. It is conceivable that this reconfirmation of additional disc extrusion by changing patient's position will help reduce the recurrence rates.
In this study, there was no significant difference in recurrence rates between the fragmentectomy and the conventional microdiscectomy groups. Kast et al.9) and Fakouri et al.6) reported a lower recurrence rate of 5% in their sequestrectomy group than the conventional microdiscectomy group. However Rogers13) reported a reoperation rate of 21% in patients undergoing fragmentectomy, which is the highest rate in the literature. In contrast, Faulhauer and Manicke7) reported the lowest recurrence rates of 2% in patients treated with sequestrectomy. In our study, 3 (4.05%) of the 74 patients in the fragmentectomy group relapsed, all of whom underwent reoperation such as conventional microdiscectomy. Of course, there were more reoperated patients who were not selected according to the exclusion criteria. They underwent reoperation due to infections or postoperative hematomas. Since these may have affected the VAS scores obtained 2 and 6 weeks after surgery, we excluded these patients from the study.
The mean recurrence time from the first operation was 4.7 months (range, 1-15 months). We could not determine whether the differences in recurrence rates were attributable to the operative method or other factors. One of the reasons for this difference may be that environmental factors, such as obesity, occupational activities, and posture. Additional prospective studies should be performed in these aspects as well as on the correlation between the preservation of the normal disc materials and the prevention of a series of disc degenerations.
In this study, we compared the VAS scores obtained 2 and 6 weeks after surgery. Patients who underwent fragmentectomy less frequently complained of back pain the day after surgery and ambulated more comfortably. However, there were no significant differences in VAS scores after surgery between the fragmentectomy and conventional microdiscectomy groups. Both surgical methods showed a remarkable improvement in the VAS scores for back and radicular pains.
From the results of this study, it is suggested that fragmentectomy may not increase recurrence rates or cause significant differences in postoperative VAS scores of back and radicular pains. If patients are selected according to well-defined criteria, fragmentectomy can be a good surgical option for LDH in that maintains the healthy intervertebral disc materials.
References
1. Barth M, Diepers M, Weiss C, Thomé C. Two-year outcome after lumbar microdiscectomy versus microscopic sequestrectomy : part 2 : radiographic evaluation and correlation with clinical outcome. Spine (Phila Pa 1976). 2008; 33:273–279. PMID: 18303459.

2. Barth M, Weiss C, Thomé C. Two-year outcome after lumbar microdiscectomy versus microscopic sequestrectomy : part 1 : evaluation of clinical outcome. Spine (Phila Pa 1976). 2008; 33:265–272. PMID: 18303458.

3. Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica : the effects of fragment type and anular competence. J Bone Joint Surg Am. 2003; 85:102–108. PMID: 12533579.
4. Carragee EJ, Spinnickie AO, Alamin TF, Paragioudakis S. A prospective controlled study of limited versus subtotal posterior discectomy : short-term outcomes in patients with herniated lumbar intervertebral discs and large posterior anular defect. Spine (Phila Pa 1976). 2006; 31:653–657. PMID: 16540869.

5. Caspar W. Wullenweber R, Brock M, Hamer J, editors. A new surgical procedure for lumbar disc herniation causing less tissue damage through a microsurgical approach. Advances in Neurosurgery. 1977. Berlin: Springer-Verlag;p. 74–77.

6. Fakouri B, Patel V, Bayley E, Srinivas S. Lumbar microdiscectomy versus sequesterectomy/free fragmentectomy : a long-term (>2 y) retrospective study of the clinical outcome. J Spinal Disord Tech. 2011; 24:6–10. PMID: 20087226.
7. Faulhauer K, Manicke C. Fragment excision versus conventional disc removal in the microsurgical treatment of herniated lumbar disc. Acta Neurochir (Wien). 1995; 133:107–111. PMID: 8748751.

8. Goodkin R, Laska LL. Vascular and visceral injuries associated with lumbar disc surgery : medicolegal implications. Surg Neurol. 1998; 49:358–370. discussion 370-372. PMID: 9537654.
9. Kast E, Oberle J, Richter HP, Börm W. Success of simple sequestrectomy in lumbar spine surgery depends on the competence of the fibrous ring : a prospective controlled study of 168 patients. Spine (Phila Pa 1976). 2008; 33:1567–1571. PMID: 18552672.

10. Kim DS, Lee JK, Moon KS, Ju JK, Kim SH. Small bowel injury as a complication of lumbar microdiscectomy : case report and literature review. J Korean Neurosurg Soc. 2010; 47:224–227. PMID: 20379478.

11. Kjaer P, Leboeuf-Yde C, Korsholm L, Sorensen JS, Bendix T. Magnetic resonance imaging and low back pain in adults : a diagnostic imaging study of 40-year-old men and women. Spine (Phila Pa 1976). 2005; 30:1173–1180. PMID: 15897832.

12. Mochida J, Nishimura K, Nomura T, Toh E, Chiba M. The importance of preserving disc structure in surgical approaches to lumbar disc herniation. Spine (Phila Pa 1976). 1996; 21:1556–1563. discussion 1563-1564. PMID: 8817784.

13. Rogers LA. Experience with limited versus extensive disc removal in patients undergoing microsurgical operations for ruptured lumbar discs. Neurosurgery. 1988; 22:82–85. PMID: 3344091.

14. Striffeler H, Gröger U, Reulen HJ. "Standard" microsurgical lumbar discectomy vs. "conservative" microsurgical discectomy. A preliminary study. Acta Neurochir (Wien). 1991; 112:62–64. PMID: 1763685.

15. Thomé C, Barth M, Scharf J, Schmiedek P. Outcome after lumbar sequestrectomy compared with microdiscectomy : a prospective randomized study. J Neurosurg Spine. 2005; 2:271–278. PMID: 15796351.

16. Watters WC 3rd, McGirt MJ. An evidence-based review of the literature on the consequences of conservative versus aggressive discectomy for the treatment of primary disc herniation with radiculopathy. Spine J. 2009; 9:240–257. PMID: 18809356.

17. Wenger M, Mariani L, Kalbarczyk A, Gröger U. Long-term outcome of 104 patients after lumbar sequestrectomy according to Williams. Neurosurgery. 2001; 49:329–334. discussion 334-335. PMID: 11504108.

18. Wera GD, Dean CL, Ahn UM, Marcus RE, Cassinelli EH, Bohlman HH, et al. Reherniation and failure after lumbar discectomy : a comparison of fragment excision alone versus subtotal discectomy. J Spinal Disord Tech. 2008; 21:316–319. PMID: 18600139.

19. Williams RW. Microlumbar discectomy : a conservative surgical approach to the virgin herniated lumbar disc. Spine (Phila Pa 1976). 1978; 3:175–182. PMID: 663769.
Fig. 1
Visual analogue scale (VAS) scores of back pain in the fragmentectomy and conventional microdiscectomy groups were improved 2 and 6 weeks after surgery. The scores were more improved 2 weeks after surgery in the conventional microdiscectomy group, whereas they were slightly more improved 6 weeks after surgery in the fragmentectomy group.
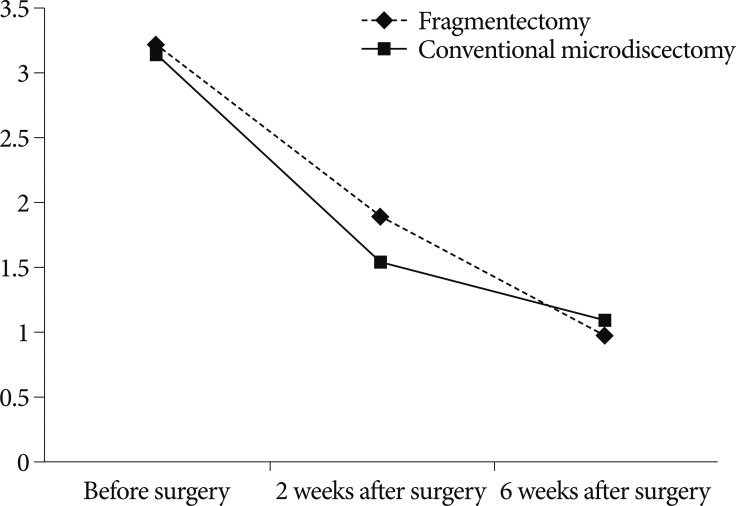
Fig. 2
Visual analogue scale (VAS) scores of radicular pain in fragmentectomy and conventional microdiscectomy groups were similarly improved 2 weeks and 6 weeks after surgery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download