Abstract
Terson syndrome was originally used to describe a vitreous hemorrhage arising from aneurysmal subrarachnoid hemorrhage. Terson syndrome can be caused by intracranial hemorrhage, subdural or epidural hematoma and severe brain injury but is extremely rare in intraventricular hemorrhage associated with moyamoya disease. A 41-year-old man presented with left visual disturbance. He had a history of intraventicular hemorrhage associated with moyamoya disease three months prior to admission. At that time he was in comatose mentality. Ophthalmologic examination at our hospital detected a vitreous hemorrhage in his left eye, with right eye remaining normal. Vitrectomy with epiretinal membrane removal was performed. After operation his left visual acuity was recovered. Careful ophthalmologic examination is mandatory in patients with hemorrhagic moyamoya disease.
Terson syndrome was originally used to describe a vitreous hemorrhage arising from aneurysmal subrarachnoid hemorrhage (SAH). Numerous studies have been published regarding the incidence of not only subhyaloid but more generally of vitreous and retinal hemorrhages associated with aneurysmal SAH. Terson syndrome can be caused by coagulopathy-induced intracranial hemorrhage, subdural or epidural hematoma and severe brain injury. Terson syndrome due to intraventricular hemorrhage (IVH) associated with moyamoya disease has been reported just one case in prior literatures. Recently, we experienced a rare case of Terson syndrome caused by IVH in a patient with moyamoya disease.
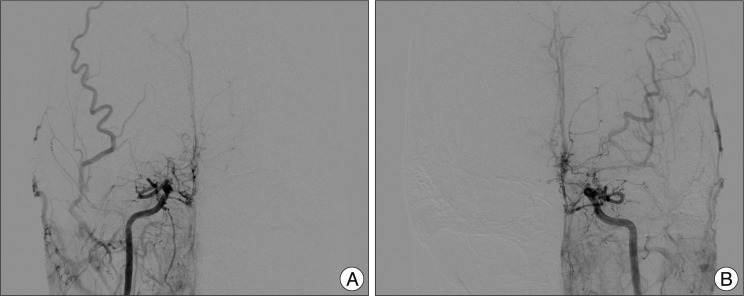
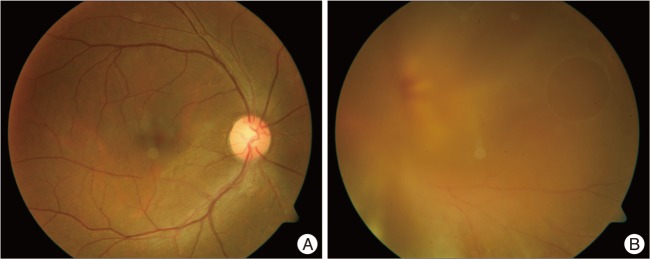
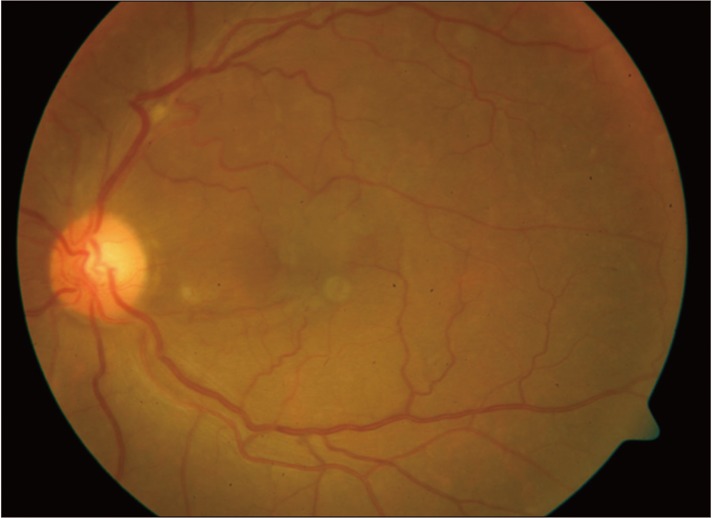
A 41-year-old man complaining of left visual disturbance visited our department. He had a history of IVH associated with moyamoya disease three months ago. He was comatose at the initial presentation. Computed tomography (CT) at the first visiting hospital demonstrated IVH with hydrocephalus (Fig. 1). Cerebral angiography showed severe bilateral stenosis at the distal internal carotid artery and basal moyamoya vessels. It was compatible with moyamoya disease (Fig. 2). Emergent extraventricular drainage was performed. His mentality gradually improved to alert. Ophthalmologic examination at our hospital detected a vitreous hemorrhage in his left eye (Fig. 3B), with right eye remaining normal (Fig. 3A). In spite of three months conservative care, his visual acuity was not improved. Vitrectomy with epiretinal membrane removal was performed (Fig. 4). After operation his left visual acuity was recovered.
Several pathogenetic theories have been proposed for explaining the development of Terson hemorrhage since its original description2-6,8,9,11,13,14,18). The most widely accepted pathogenetic mechanism suggests that a suddenly increased intracranial pressure (IICP) is propagated from the intracranial compartment to the orbit through a rapid effusion of cerebrospinal fluid via the optic nerve sheath2,5,13,14,16,18). The venous obstruction causes venous stasis, which results in distention and rupture of the fine retinal capillaries5,14). This pathogenetic mechanism explains the association of Terson hemorrhage with pathological conditions other than SAH.
The occurrence of Terson hemorrhage has been described in cases of moyamoya disease1), severe closed-head injuries5,11,18), intracerebral hemorrhage11), carotid artery occlusion11), cranial subdural hematoma17), lumbosacral myelomeningocele19), and as a complication associated with intraarterial angiography6).
The present case shows that IVH secondary to moyamoya disease can induce an abrupt increase in ICP resulting in Terson hemorrhage. If the only reason of Terson syndrome is venous congestion due to IICP, equal incidence of Terson hemorrhage as seen in SAH should be present in the other IICP conditions. But, the other IICP conditions do not show the same incidence of SAH associated Terson hrmorrhage. Therefore, the other factors may be associated with the development of Terson hemorrhage14,15,20).
Patients with moyamoya disease can exhibit various ocular symptoms which are mainly caused by stenotic and occulsive lesions in the occipital visual cortex or optic pathways or tract, but have relatively normal intraocular findings10,12).
Careful ophthalmological examination including meticulous fundoscopic evaluation remains the method of choice for detecting Terson hemorrhage. The ideal timing for performing an ophthalmological examination remains to be defined. Manschot8) reported that all Terson hemorrhages were present within one hour from the ictal event. However, delayed Terson hemorrhage might occur up to 47 days after the ictus.
Swallow et al.17) evaluated the potential of CT scans of the orbits for detecting Terson hemorrhages. They found that in the majority (66.7%) of patients with Terson hemorrhage, characteristic retinal nodularity and retinal crescentic hyperdensities were evident on their CT scans17). However, in our case we could not see the evidence of retinal or orbital hemorrhage on initial CT scans.
The visual outcome was excellent in the majority of cases of Terson hemorrhage. In rare instances, however, Terson hemorrhage can be associated with the development of proliferative retinopathy, retinal breaks, retinal detachment, and cataract20). Surgical intervention is reserved for those cases in which there is no visual acuity improvement within 6 months from the ictal event5,18). The surgical treatment of choice, when indicated, is pars plana vitrectomy7).
Moyamoya disease may accompany various ocular symptoms such as visual field defect, amaurosis fugax, decreased visual acuity and scintillating scotoma. Majority of these visual symptoms are usually result from ischemic lesions in the visual cortex and optic pathways.
Terson syndrome can be a rare cause of visual diturbance of patients with hemorrhagic moyamoya disease. Careful ophthalmologic examination is mandatory in these patients.
References
1. Arakawa Y, Goto Y, Ishii A, Ueno Y, Kikuta K, Yoshizumi H, et al. Terson syndrome caused by ventricular hemorrhage associated with moyamoya disease--case report. Neurol Med Chir (Tokyo). 2000; 40:480–483. PMID: 11021082.

2. Ballantyne AJ. The ocular manifestations of spontaneous subarachnoid hemorrhage. Br J Ophthalmol. 1943; 27:383–414. PMID: 18169953.
3. Clarkson JG, Flynn HW Jr, Daily MJ. Vitrectomy in Terson's syndrome. Am J Ophthalmol. 1980; 90:549–552. PMID: 7424753.

4. Frizzell RT, Kuhn F, Morris R, Quinn C, Fisher WS 3rd. Screening for ocular hemorrhages in patients with ruptured cerebral aneurysms: a prospective study of 99 patients. Neurosurgery. 1997; 41:529–533. discussion 533-534. PMID: 9310968.

5. Garfinkle AM, Danys IR, Nicolle DA, Colohan AR, Brem S. Terson's syndrome: a reversible cause of blindness following subarachnoid hemorrhage. J Neurosurg. 1992; 76:766–771. PMID: 1564539.

6. Hedges TR Jr, Walsh FB. Optic nerve sheath and subhyaloid hemorrhage as a complication of angiocardiography. AMA Arch Ophthalmol. 1955; 54:425–427. PMID: 13248305.

7. Kuhn F, Morris R, Witherspoon CD, Mester V. Terson syndrome. Results of vitrectomy and the significance of vitreous hemorrhage in patients with subarachnoid hemorrhage. Ophthalmology. 1998; 105:472–477. PMID: 9499778.
8. Manschot WA. Subarachnoid hemorrhage; intraocular symptoms and their pathogenesis. Am J Ophthalmol. 1954; 38:501–505. PMID: 13197505.
9. McCarron MO, Alberts MJ, McCarron P. A systematic review of Terson's syndrome : frequency and prognosis after subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 2004; 75:491–493. PMID: 14966173.

10. Miyamoto S, Kikuchi H, Karasawa J, Nagata I, Ihara I, Yamagata S. Study of the posterior circulation in moyamoya disease. Part 2 : Visual disturbances and surgical treatment. J Neurosurg. 1986; 65:454–460. PMID: 3760953.
11. Muller PJ, Deck JH. Intraocular and optic nerve sheath hemorrhage in cases of sudden intracranial hypertension. J Neurosurg. 1974; 41:160–166. PMID: 4366848.

12. Noda S, Hayasaka S, Setogawa T, Matsumoto S. Ocular symptoms of moyamoya disease. Am J Ophthalmol. 1987; 103:812–816. PMID: 3591879.

13. Ogawa T, Kitaoka T, Dake Y, Amemiya T. Terson syndrome : a case report suggesting the mechanism of vitreous hemorrhage. Ophthalmology. 2001; 108:1654–1656. PMID: 11535467.
14. Pfausler B, Belcl R, Metzler R, Mohsenipour I, Schmutzhard E. Terson's syndrome in spontaneous subarachnoid hemorrhage : a prospective study in 60 consecutive patients. J Neurosurg. 1996; 85:392–394. PMID: 8751622.

15. Roux FX, Panthier JN, Tanghe YM, Gallina P, Oswald AM, Mérienne L, et al. [Terson's syndrome and intraocular complications in meningeal hemorrhages (26 cases)]. Neurochirurgie. 1991; 37:106–110. PMID: 1852236.
16. Schultz PN, Sobol WM, Weingeist TA. Long-term visual outcome in Terson syndrome. Ophthalmology. 1991; 98:1814–1819. PMID: 1775315.

17. Swallow CE, Tsuruda JS, Digre KB, Glaser MJ, Davidson HC, Harnsberger HR. Terson syndrome : CT evaluation in 12 patients. AJNR Am J Neuroradiol. 1998; 19:743–747. PMID: 9576666.
18. Vanderlinden RG, Chisholm LD. Vitreous hemorrhages and sudden increased intracranial pressure. J Neurosurg. 1974; 41:167–176. PMID: 4842785.

19. Weaver RG, Davis CH Jr. Subhyaloid hemorrhage. Am J Ophthalmol. 1961; 52:257–259. PMID: 13783552.

20. Wiethölter S, Steube D, Stotz HP. [Terson syndrome : a frequently missed ophthalmologic complication in subarachnoid hemorrhage]. Zentralbl Neurochir. 1998; 59:166–170. PMID: 9816667.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download