1. Malamed SF. Handbook of Local Anesthesia. 6th ed. St. Louis: Mosby;Elsevier;2013.
2. Wong JK. Adjuncts to Anesthesia: Separating Fact to Fiction. J Can Dent Assoc. 2001; 67:391–397. PMID:
11468097.
3. Graetz C, Fawzy-El-Sayed KM, Graetz N, Dorfer CE. Root damage induced by intraosseous anesthesia. An in vitro investigation. Med Oral Patol Oral Cir Bucal. 2013; 18:e130–e134. PMID:
23229260.
4. Woodmansey KF, White RK, He J. Osteonecrosis related to intraosseous anesthesia: Report of a case. J Endod. 2009; 35:288–291. PMID:
19166792.

5. Remmers T, Glickman G, Spears R, He J. The efficacy of IntraFlow intraosseous injection as a primary anesthesia technique. J Endod. 2008; 34:280–283. PMID:
18291275.

6. Nusstein J, Reader A, Nist R, Beck M, Meyers WJ. Anesthetic efficacy of the supplemental intraosseous injection of 2% lidocaine with 1:100,000 epinephrine in irreversible pulpitis. J Endod. 1998; 24:487–491. PMID:
9693577.

7. Reisman D, Reader A, Nist R, Beck M, Weaver J. Anesthetic efficacy of the supplemental intraosseous injection of 3% mepivacaine in irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997; 84:676–682. PMID:
9431539.

8. Bigby J, Reader A, Nusstein J, Beck M, Weaver J. Articaine for supplemental intraosseous anesthesia in patients with irreversible pulpitis. J Endod. 2006; 32:1044–1047. PMID:
17055903.

9. Parente SA, Anderson RW, Herman WW, Kimbrough WF, Weller RN. Anesthetic efficacy of the supplemental intraosseous injection for teeth with irreversible pulpitis. J Endod. 1998; 24:826–828. PMID:
10023263.

10. Pereira LA, Groppo FC, Bergamaschi Cde C, Meechan JG, Ramacciato JC, Motta RH, et al. Articaine (4%) with epinephrine (1:100,000 or 1:200,000) in intraosseous injections in symptomatic irreversible pulpitis of mandibular molars: anesthetic efficacy and cardiovascular effects. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 116:e85–e91. PMID:
22841432.

11. Demir E, Ataoglu H. Clinic evaluation of efficacy of transcotical anesthesia for extraction of impacted third molars. Br J Oral Maxillofac Surg. 2016; 54:e100.

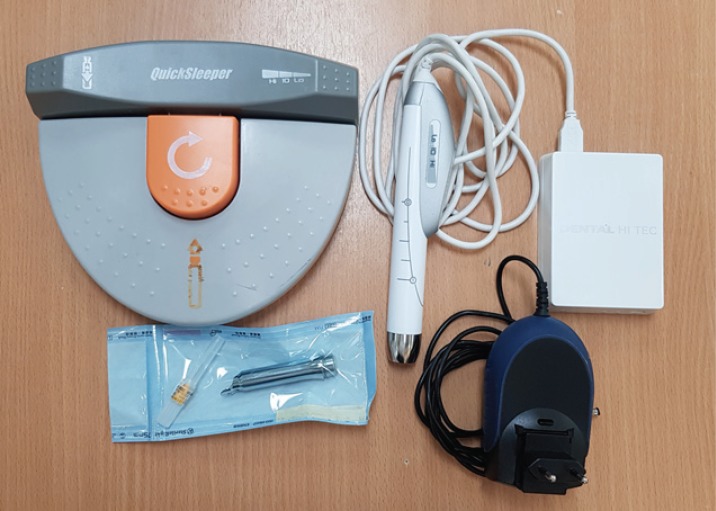
12. Kiattavorncharoen S, Wongsirichat N, Boonsiriseth K. The anesthesia efficacy of intraosseous injection with Quicksleeper® and conventional injection in the lower third molar surgery. M Dent J. 2013; 33:137–143.
13. Ozer S, Yaltirik M, Kirli I, Yargic I. A comparative evaluation of pain and anxiety levels in 2 different anesthesia techniques: locoregional anesthesia using conventional syringe versus intraosseous anesthesia using a computer-controlled system (Quicksleeper®). Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 114(5 suppl):S132–S139. PMID:
23063389.
14. Smail-Faugeron V, Muller-Bolla M, Sixou JL, Courson F. Split-mouth and parallel-arm trials to compare pain with intraosseous anaesthesia delivered by the computerised Quicksleeper system and conventional infiltration anaesthesia in paediatric oral healthcare: protocol for a randomised controlled trial. BMJ Open. 2015; 5:e007724.

15. González-Castro O, Arias A. Controlled flow of dental anesthesia solution to reduce pain and anxiety. Int J Clin Anesthesiol. 2017; 5:1075.
16. Dunbar D, Reader A, Nist R, Beck M, Meyers WJ. Anesthetic efficacy of the intraosseous injection after an inferior alveolar nerve block. J Endod. 1996; 22:481–486. PMID:
9198431.

17. Replogle K, Reader A, Nist R, Beck M, Weaver J, Meyers WJ. Anesthetic efficacy of the intraosseous injection of 2% lidocaine (1:100,000 epinephrine) and 3% mepivacaine in mandibular first molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997; 83:30–37. PMID:
9007920.

18. Jensen J, Nusstein J, Drum M, Reader A, Beck M. Anesthetic Efficacy of a Repeated Intraosseous Injection Following a Primary Intraosseous Injection. J Endod. 2008; 34:126–130. PMID:
18215666.

19. Beneito-Brotons R, Penarrocha-Oltra D, Ata-Ali J, Penarrocha M. Intraosseous anesthesia with solution injection controlled by a computerized system versus conventional oral anesthesia: a preliminary study. Med Oral Patol Oral Cir Bucal. 2012; 17:e426–e429. PMID:
22143722.

20. Prohic S, Sulejmanagic H, Secic S. The efficacy of supplemental intraosseous anesthesia after insufficient mandibular block. Bosn J Basic Med Sci. 2005; 5:57–60. PMID:
15771604.
21. Terrer É TF, Coudrec G, Vialatte L, Tramini P, Tassery H. Anesthesie osteo-centrale versus locoregional du bloc du nerf dentaire inferieur. L’information Dentaire. 2014; 35:e007724.
22. Cabasse C, Marie-Cousin A, Huet A, Sixou JL. Computer-assisted intraosseous anaesthesia for molar and incisor hypomineralisation teeth. A preliminary study. Odontostomatol Trop. 2015; 38:5–9.
23. Couderc G, Weisrock G, Tassery H. L’anesthésie transcorticale dans la prise en charge des urgences d’un centre de soins hospitalo-universitaire. Le Fil Dentaire. 2009; 43.
24. Chang H, Noh J, Lee J, Kim S, Koo KT, Kim TI, et al. Relief of Injection Pain During Delivery of Local Anesthesia by Computer-Controlled Anesthetic Delivery System for Periodontal Surgery: Randomized Clinical Controlled Trial. J Periodontol. 2016; 87:783–789. PMID:
26991489.

25. Han K, Kim J. Intraosseous anesthesia using a computer-controlled system during non-surgical periodontal therapy (root planing): Two case reports. J Dent Anesth Pain Med. 2018; 18:65–69. PMID:
29556561.

26. Kim C, Hwang KG, Park CJ. Local anesthesia for mandibular third molar extraction. J Dent Anesth Pain Med. 2018; 18:287–294. PMID:
30402548.

27. Demir E, Ataoglu H. Clinic evaluation of efficacy of transcotical anesthesia for extraction of impacted third molars. Br J Oral Maxillofac Surg. 2016; 54:e100.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download