Abstract
Background
A possible risk factor for brain tumor might be measles, since late neurologic sequelae are part of measles pathology. Subacute sclerosing panencephalitis, a devastating neurologic illness, is prone to develop years after measles infection.
Methods
Because measles damage to the brain might increase the risk of brain tumor, we examined the relationship of measles incidence in 1960 and brain tumor incidence in 50 US States and the District of Columbia, 2004-2007. Data on number of cases of measles by state in 1960 are from the Morbidity and Mortality Weekly Report. In 1960 measles was a childhood illness. We calculated measles incidence by obtaining the population of each state from the 1960 US Census and then age adjusting our results to the cumulative percent of the state population under age 21, since this would have been the measles-infected group. Data on the percentage white population by state are from the US Census (www.census.gov). Age-adjusted incidence (to the 2000 US standard population) of brain tumors is from the Central Brain Tumor Registry of the United States 2011 report.
Results
There was a significant correlation between 1960 measles incidence and incidence of malignant brain tumors in persons 20 and older in 2004-2007 (r=0.321, p=0.026). Because glioblastoma is more frequent in whites and males, multivariate linear regression was performed with tumor incidence as the dependent variable, measles incidence, percent white population, and sex ratio by state as independent variables. Measles incidence was significantly correlated with malignant brain tumor incidence (β=0.361, p<0.001) and independent of the effect of race (β=0.734, p<0.001) and sex ratio m/f (β=-0.478, p<0.001). There was no correlation of measles incidence with brain tumor incidence in persons younger than 20.
Primary brain tumors account for 2% of cancer deaths. Gliomas make up 60% of these tumors and are frequently malignant. Meningioma is a benign tumor that represents 20% of brain neoplasms. Hereditary syndromes are well established risk factors for both glioma and meningioma [1].
Meningioma incidence increases with age. Ionizing radiation and head trauma may be risk factors [2]. Glioblastoma multiforme is the most common and most aggressive type of primary brain tumor, accounting for 52% of all primary brain tumor cases and 20% of all intracranial tumors. Gliomas are more common in whites, and appear to be sporadic, most without any genetic predisposition. Ionizing radiation is a risk factor [1]. No conclusive links have been found between gliomas and smoking, diet, cellular phones, or electromagnetic fields. Recently, evidence for a viral cause for glioblastoma multiforme, human cytomegalovirus (CMV), has been postulated, although the evidence is inconsistent [3456].
A possible risk factor for brain tumor might be measles, since late neurologic sequelae are part of measles pathology. Subacute sclerosing panencephalitis, a devastating neurologic illness, is prone to develop years after measles infection [7]. The measles virus has immunosuppressive properties [8] that could promote the development of tumors. Moreover, Cattaneo et al. [9] have found biased hypermutation and other genetic changes in defective measles viruses in human brain infections. Clusters of mutations favor the propagation of the virus within the brain.
Because measles damage to the brain might increase the risk of brain tumor, we examined the relationship of measles incidence in 1960 and brain tumor incidence in 49 US States and the District of Columbia, 2004-2007. Measles was a non-notifiable infectious disease in Kansas, 1960, and so this one state is not included.
Data on number of cases of measles by state in 1960 are from Table 5 of Morbidity and Mortality Weekly Report [10]. In 1960 measles was a childhood illness. We calculated measles incidence by obtaining the population of each state from the 1960 US Census and then age adjusting our results to the cumulative percent of the state population under age 21, since this would have been the measles-infected group. The 1960 data were chosen because they are the only published data on measles incidence in the US before the advent of measles vaccine.
Data on the percentage white population and sex ratio by state are from the US Census (www.census.gov). Age-adjusted incidence (to the 2000 US standard population) of brain tumors 2004-2007 is from Table 10 of the Central Brain Tumor Registry of the United States 2011 report [11]. We chose this set of tumor data because it is the most recent available broken down by age group.
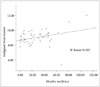
There was a significant correlation between 1960 measles incidence and incidence of malignant brain tumors in persons 20 and older in 2004-2007 (r=0.321, p=0.026) (Fig. 1). Because glioblastoma is more frequent in whites and males, multivariate linear regression was performed with tumor incidence as the dependent variable, measles incidence, percent white population, and sex ratio by state as independent variables. Measles incidence was significantly correlated with malignant brain tumor incidence (β=0.361, p<0.001) and independent of the effect of race (β=0.734, p<0.001) and sex ratio m/f (β=-0.478, p<0.001). There was no correlation of measles incidence with brain tumor incidence in persons younger than 20.
There was a significant correlation between 1960 measles incidence and incidence of non-malignant brain tumors (r=0.305, p=0.035) in persons 20 and older in 2004-2007. However, in a multivariate analysis, the correlation of measles incidence and non-malignant brain tumor incidence only approached significance (β=0.286, p=0.063) and was unrelated to race (β=0.071, p=0.643) or sex ratio m/f (β=-0.004, p=0.981).
There have been attempts to implicate various viruses in the genesis of brain tumors. Polyomaviruses, including the JC virus, the BK virus, and simian virus 40, have been identified in human glioma tissues and have induced brain tumors in animals [12]. A herpes virus, human CMV, is implicated in glioblastoma, and one report found CMV circulating in the peripheral blood of 80% of patients [5]. Although we were unable to replicate this finding [4], a consensus holds that CMV plays a role [13].
Measles virus might also predispose to brain tumors. The inflammation of subacute sclerosing panencephalitis, even subclinical cases, could well promote tumor formation, since many tumors arise from sites of infection, chronic irritation and inflammation [14]. Moreover, inflammation is a critical component of tumor progression.
The absence of correlation of measles incidence with brain tumor incidence in persons younger than 20 is expected. These people would not have been included in the 1960 Morbidity and Mortality Weekly Report, and would be, in general, too young to be significantly affected by meningioma or glioma.
A weakness in our analysis, presented above, is possible confounding by the ecological fallacy (or ecological inference fallacy), a logical fallacy in the interpretation of statistical data where inferences about the nature of individuals are derived from inference for the group to which those individuals belong [15]. In this case, inferences about individuals are being drawn from the characteristics of US states where they reside, rather than from the individuals themselves. Another problem with our analysis is that populations are mobile and there is no way to factor in such movements over a forty-five year latency period. Finally, an intrinsic difficulty with correlational studies is that two variables may be associated, even if there is no causal link between them, if each is associated with some other variable.
It would be desirable to analyze measles incidence data from other decades to see if results are consistent or depend on lag period. However, no other measles incidence data sets are publicly available.
Malignant brain tumors are highly heterogeneous and ideally should not be lumped together as one category. Analyses would be best performed separately for tumor types and grades, and also by demographic variables where data are available. However, these parameters are not available tabulated by state, and this type of analysis was not possible with the data at hand.
It would be worthwhile to adjust for proportions of each major racial group, rather than only percentage white population. However, US 2010 census data are broken down by proportion of each major racial group overall, but only by non-Hispanic white alone versus minority on a state by state basis.
The first live virus measles vaccine (Rubeovax by Merck) was licensed in 1963, and measles was declared to be eliminated in the United States in 2000. But importation of measles cases and limited local transmission continue to occur [7]. Parents who refuse to vaccinate their children because of fears of autism and other chimerical sequelae of vaccination have made the situation worse. And the vaccine is not 100% effective, leading to outbreaks even in highly vaccinated groups, especially if vaccination rates fall below 95% and community immunity drops [16]. Therefore, further study of a possible measles-brain tumor association would be worthwhile.
Figures and Tables
References
1. Bondy ML, Scheurer ME, Malmer B, et al. Brain tumor epidemiology: consensus from the Brain Tumor Epidemiology Consortium. Cancer. 2008; 113:7 Suppl. 1953–1968.

2. Longstreth WT Jr, Dennis LK, McGuire VM, Drangsholt MT, Koepsell TD. Epidemiology of intracranial meningioma. Cancer. 1993; 72:639–648.

3. Lehrer S, Green S, Ramanathan L, Rosenzweig K, Labombardi V. No consistent relationship of glioblastoma incidence and cytomegalovirus seropositivity in whites, blacks, and Hispanics. Anticancer Res. 2012; 32:1113–1115.
4. Lehrer S, Green S, Ramanathan L, Rosenzweig K, Rendo A. Virology of malignant brain tumours. Eur Assoc NeuroOncol Mag. 2013; 3:23–24.
5. Mitchell DA, Xie W, Schmittling R, et al. Sensitive detection of human cytomegalovirus in tumors and peripheral blood of patients diagnosed with glioblastoma. Neuro Oncol. 2008; 10:10–18.

6. Ostrom QT, Bauchet L, Davis FG, et al. The epidemiology of glioma in adults: a "state of the science" review. Neuro Oncol. 2014; 16:896–913.

7. Zipprich J, Hacker JK, Murray EL, et al. Notes from the field: measles - California, January 1-April 18, 2014. MMWR Morb Mortal Wkly Rep. 2014; 63:362–363.
8. Hsu EC, Iorio C, Sarangi F, Khine AA, Richardson CD. CDw150 (SLAM) is a receptor for a lymphotropic strain of measles virus and may account for the immunosuppressive properties of this virus. Virology. 2001; 279:9–21.

9. Cattaneo R, Schmid A, Eschle D, Baczko K, ter Meulen V, Billeter MA. Biased hypermutation and other genetic changes in defective measles viruses in human brain infections. Cell. 1988; 55:255–265.

10. Centers for Disease Control. Annual Supplement Reported Incidence of Notifiable Diseases in the United States, 1960. Morb Mortal Wkly Rep. 1961; 9:1–24.
11. Central Brain Tumor Registry of the United States. 2011 CBTRUS Statistical Report Tables. Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2004-2007. Hinsdale, IL: CBTRUS;2011.
12. Rollison DE, Helzlsouer KJ, Alberg AJ, et al. Serum antibodies to JC virus, BK virus, simian virus 40, and the risk of incident adult astrocytic brain tumors. Cancer Epidemiol Biomarkers Prev. 2003; 12:460–463.
13. Dziurzynski K, Chang SM, Heimberger AB, et al. Consensus on the role of human cytomegalovirus in glioblastoma. Neuro Oncol. 2012; 14:246–255.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download