Abstract
We herein present a case of spontaneous rupture of intrahepatic bile duct in a patient with perihilar cholangiocarcinoma, which were successfully treated by curative resection. A 60-year-old male patient with perihilar cholangiocarcinoma was decompressed with single percutaneous transhepatic biliary drainage. Two days after right portal vein embolization, the patient suffered from paralytic ileus with marked abdominal distension. Imaging study revealed that marked fluid collection around the liver and whole abdomen, suggesting intrahepatic bile duct rupture. With abdominal drainage and biliary decompression for 2 weeks, the biliary rupture was controlled. To enhance the safety of right hepatectomy, additional right hepatic vein embolization was performed. The patient underwent routine surgical procedures for right hepatectomy, caudate lobectomy and bile duct resection, and recovered uneventfully and discharged 18 days after surgery. This is the first report of a case of spontaneous rupture of intrahepatic bile duct in a patient with perihilar cholangiocarcinoma.
Occlusion of perihilar bile duct leads to dilatation of the intrahepatic bile ducts. When slow gradual occlusion happens as like in perihilar cholangiocarcinoma, such dilatation becomes insidious thus showing diffuse dilatation of the involved intrahepatic bile ducts. In contrast, if rapid gradual occlusion is associated with friable liver parenchyma such as rapidly regenerated remnant livers or partial liver grafts following living donor liver transplantation, such pressure increase in the intrahepatic bile duct can induce intrahepatic biloma formation.1-4 In any situation, spontaneous rupture of the intrahepatic duct or biloma has not been reported yet in literature.
We herein present a case of spontaneous rupture of intrahepatic bile duct in a patient with perihilar cholangiocarcinoma following portal vein embolization, which were successfully treated by curative resection.
A 60-year-old male patient was referred to our institution under the diagnosis of perihilar cholangiocarcinoma. Computed tomography (CT) findings were compatible to those of hilar cholangiocarcinoma Bismuth-Corlette type IIIa with encasement of the right hepatic artery (Fig. 1). A percutaneous transhepatic biliary drainage (PTBD) tube was inserted into the right hepatic duct, and crossed over the hilar stenotic portion and then passed into the ampulla of Vater for probably simultaneous internal drainage. Since we were not accustomed to such placement of PTBD tube and total bilirubin level decreased gradually like in the usual perihilar cholangiocarcinoma cases, we did not perform any other procedure for biliary drainage.
In order to induce regeneration of the future remnant left liver, we performed right portal vein embolization (Fig. 2). Two days after this procedure, the patient suffered from paralytic ileus with marked abdominal distension (Fig. 3). Emergency CT scan revealed that marked fluid collection around the liver and whole abdomen, thus percutaneous drainage was performed with insertion of a pigtail catheter over the left liver. The pigtail drainage output was bilious in nature, thus leading the diagnosis of intrahepatic bile duct rupture. Follow-up CT scan showed residual fluid collection in the other area of the abdomen, thus another pigtail catheter was inserted into the pelvis. At this time, we recognized that the underlying cause of intrahepatic bile duct rupture was ineffective drainage of the left hepatic duct with overproduction of bile after right portal vein embolization. Therefore, a PTBD tube was inserted into the left liver (Fig. 4).
To enhance the safety of right hepatectomy, we performed additional right hepatic vein embolization to facilitate left liver regeneration (Fig. 5).
During laparotomy, we found that the ruptured area was the diaphragmatic side of the segment II because the superficial liver parenchyma at that area was definitely torn out. After confirmation of respectability with limited dissection of the hepatoduodenal ligament, we carried out routine surgical procedures for right hepatectomy, caudate lobectomy and bile duct resection and reconstruction. Intraabdominal biloma debris and abscess pockets were removed. Multiple abdominal drains were inserted to evacuate residual fluid in the abdomen and pelvis. The patient recovered uneventfully and discharged 18 days after surgery (Fig. 6).
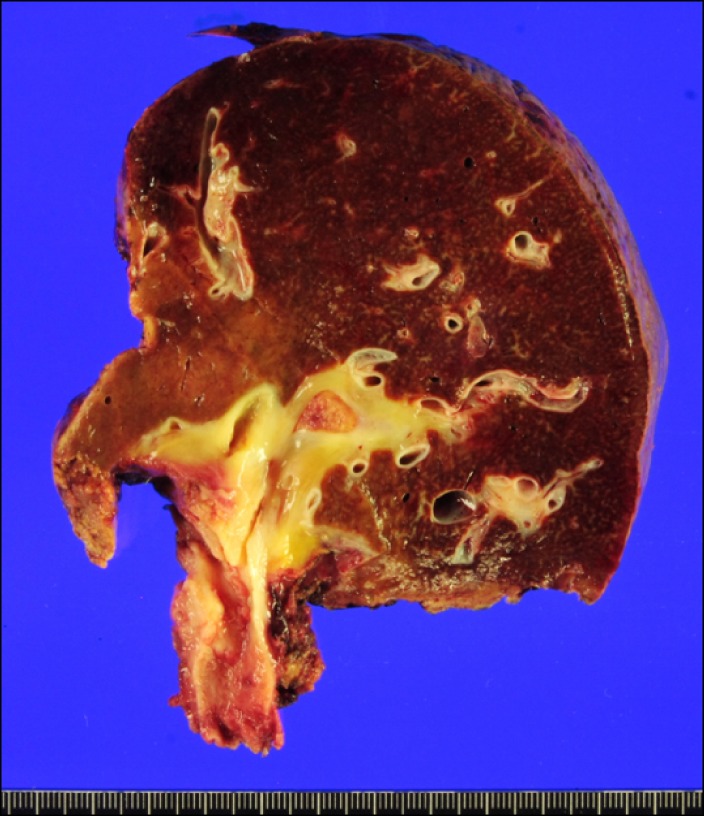
Pathological reports showed that the tumor was a 2.1 cm-sized cholangiocarcinoma with extension to perifibromuscular connective tissue and positive lymphovascular invasion (Fig. 7). There was no lymph node metastasis. No adjuvant treatment was carried out.
The underlying cause of intrahepatic bile duct rupture in this case was ineffective drainage of the left hepatic duct superimposed to overproduction of bile from the left liver following right portal vein embolization. To our knowledge, spontaneous rupture of the intrahepatic duct or biloma at any cause has not been reported yet in literature.
In this case, there was no possibility of iatrogenic intrahepatic duct injury because right portal vein embolization was performed through an ipsilateral approach, thus making no touch to the left liver.
For preoperative evaluation of bile duct involvement in perihilar cholangiocarcinoma, frequent serial surveillance of all dilated intrahepatic ducts is very beneficial for effective biliary decompression. We strongly suggest performing dynamic liver CT scan a few days before surgery to finally evaluate the liver status.
Biliary obstruction due to malignancies of the hepatobiliary system often requires biliary drainage through percutaneous or endoscopic approach. PTBD has been widely used for a long time, but has various drawbacks including procedure-related complications and tumor spread along the PTBD tract, leading to the adoption of endoscopic biliary drainage as the primary method.1-5 Endoscopic biliary drainage including endoscopic naso-biliary drainage for external drainage and endoscopic retrograde biliary drainage for internal drainage has been shown effective for biliary decompression of distal bile duct cancer, reducing the need for PTBD. In patients with perihilar cholangiocarcinoma, however, endoscopic naso-biliary drainage is often infeasible or ineffective due to the complexity of the biliary obstruction patterns. Thus, PTBD is still frequently performed in patients with perihilar cholangiocarcinoma, with complementary application of endoscopic naso-biliary drainage in patients with less advanced cancers.6,7
Portal vein embolization induces shrinkage of the embolized lobe and compensatory enlargement of the non-embolized lobe, but it does not always induce sufficient liver regeneration. There was no effective method to accelerate liver regeneration in addition to portal vein embolization yet. The early experience of first 12 cases on the effect of ipsilateral hepatic vein embolization performed after portal vein embolization was presented before.8 In a total of 30 cases of sequential portal vein embolization-ipsilateral hepatic vein embolization in our recent series, the proportions of future liver remnant volume to total liver volume increased further after hepatic vein embolization without occurrence of any procedure-related complications. We are sure that preoperative sequential application of sequential portal vein embolization-ipsilateral hepatic vein embolization is safe and effective in facilitating contralateral liver regeneration by inducing more severe liver damage than portal vein embolization alone.8-10
This is the first report of a case of spontaneous rupture of intrahepatic bile duct following portal vein embolization in a patient with perihilar cholangiocarcinoma.
References
1. Takahashi Y, Nagino M, Nishio H, et al. Percutaneous transhepatic biliary drainage catheter tract recurrence in cholangiocarcinoma. Br J Surg. 2010; 97:1860–1866. PMID: 20799295.

2. Maguchi H, Takahashi K, Katanuma A, et al. Preoperative biliary drainage for hilar cholangiocarcinoma. J Hepatobiliary Pancreat Surg. 2007; 14:441–446. PMID: 17909711.

3. Arakura N, Takayama M, Ozaki Y, et al. Efficacy of preoperative endoscopic nasobiliary drainage for hilar cholangiocarcinoma. J Hepatobiliary Pancreat Surg. 2009; 16:473–477. PMID: 19300895.

4. Lee SG, Lee YJ, Park KM, et al. One hundred and eleven liver resections for hilar bile duct cancer. J Hepatobiliary Pancreat Surg. 2000; 7:135–141. PMID: 10982605.

5. Lee SG, Song GW, Hwang S, et al. Surgical treatment of hilar cholangiocarcinoma in the new era: the Asan experience. J Hepatobiliary Pancreat Sci. 2010; 17:476–489. PMID: 19851704.

6. Hwang S, Song GW, Ha TY, et al. Reappraisal of percutaneous transhepatic biliary drainage tract recurrence after resection of perihilar bile duct cancer. World J Surg. 2012; 36:379–385. PMID: 22159824.

7. Kim TH, Lee SK, Han JH, et al. The role of endoscopic retrograde cholangiography for biliary stricture after adult living donor liver transplantation: technical aspect and outcome. Scand J Gastroenterol. 2011; 46:188–196. PMID: 20955089.

8. Hwang S, Lee SG, Ko GY, et al. Sequential preoperative ipsilateral hepatic vein embolization after portal vein embolization to induce further liver regeneration in patients with hepatobiliary malignancy. Ann Surg. 2009; 249:608–616. PMID: 19300228.

9. Hwang S. Right hepatectomy in a patient with hepatocellular carcinoma after induction of hepatic parenchymal atrophy through subsequent portal and hepatic vein embolizations. Korean J Gastroenterol. 2011; 58:162–165. PMID: 21960106.

10. Ko GY, Hwang S, Sung KB, et al. Interventional oncology: new options for interstitial treatments and intravascular approaches: right hepatic vein embolization after right portal vein embolization for inducing hypertrophy of the future liver remnant. J Hepatobiliary Pancreat Sci. 2010; 17:410–412. PMID: 19890603.
Fig. 1
Imaging finding of a patient with perihilar cholangiocarcinoma. (A) Initial computed tomography image; (B) Initial magnetic resonance cholangiography; (C) A percutaneous transhepatic biliary drainage (PTBD) tube was inserted into the right hepatic duct; (D) The PTBD tube was crossed over the hilar stenotic portion and then passed into the ampulla of Vater.
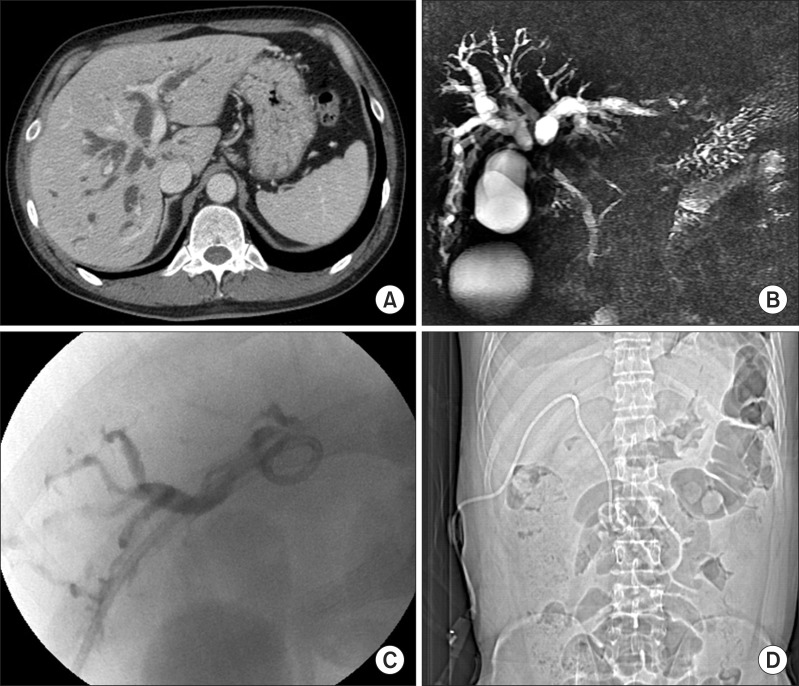
Fig. 2
Preoperative right portal vein embolization with ipsilateral approach (A) and post-embolization direct portogram (B).
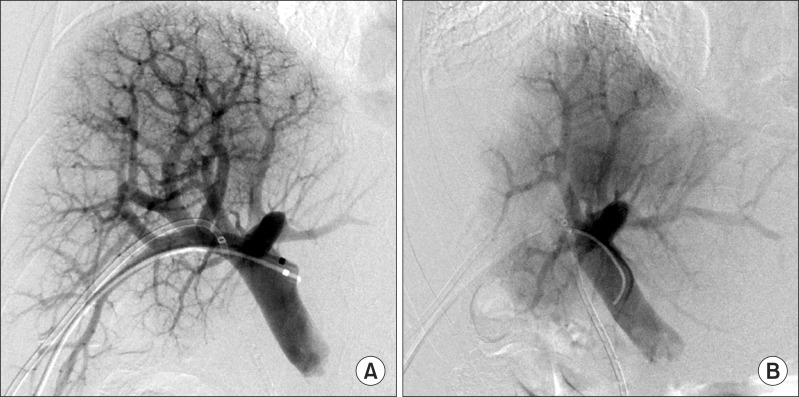
Fig. 3
Computed tomography image showing diffuse fluid collection in the abdomen and pelvis. (A) Perihepatic fluid collection; (B) A percutaneous transhepatic biliary drainage (PTBD) was placed into the right hepatic duct; (C) A large amount of fluid was collected in the pelvis.
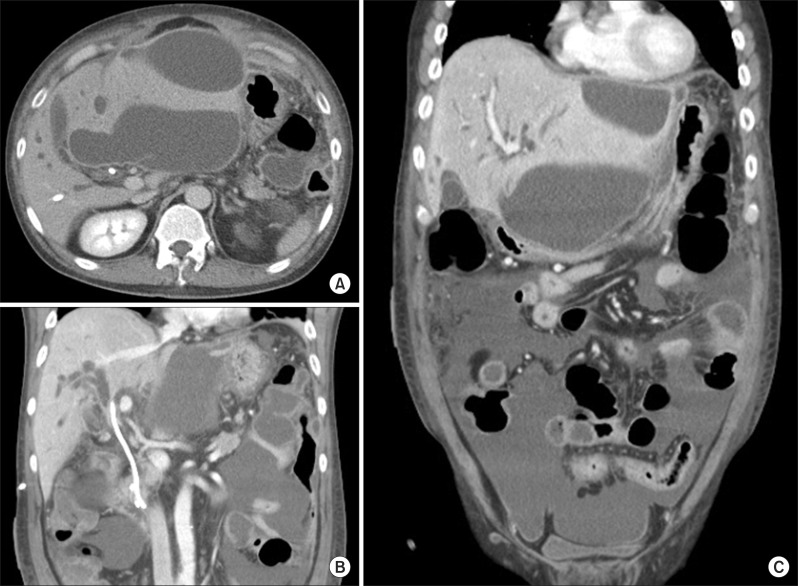
Fig. 4
Insertion of a new percutaneous transhepatic biliary drainage tube into the left hepatic duct.
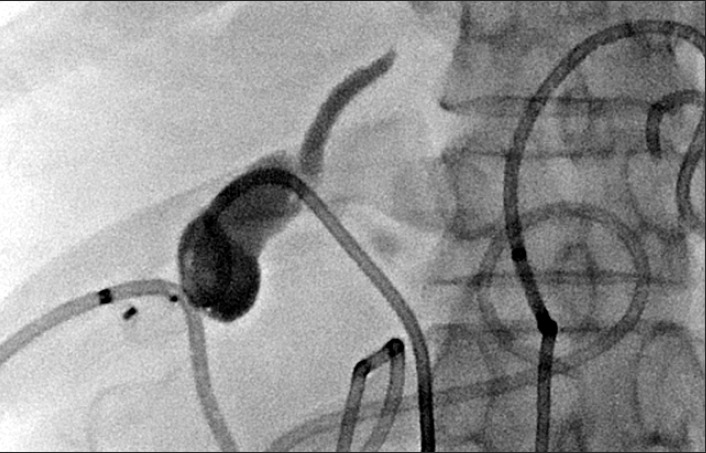
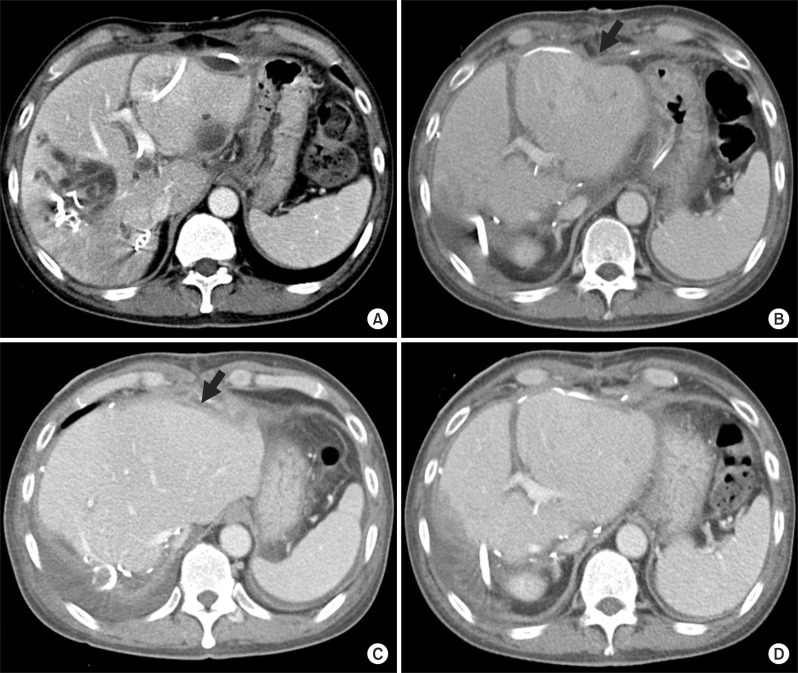
Fig. 6
Perioperative changes of computed tomography (CT) findings. (A) Liver CT taken 2 days before surgery; (B) Liver CT taken 5 days after surgery. An arrow indicates the dimpled site of liver rupture; (C) Liver CT taken 12 days after surgery. An arrow indicates the dimpled site of liver rupture; (D) Liver CT taken 12 days after surgery shows uneventful regeneration of the remnant left liver.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download