Abstract
Objective
The risk of complications is high for patients with a large cranial defect and hydrocephalus, undergoing cranioplasty and ventriculoperitoneal (VP) shunt operation. The purpose of this study is to examine retrospectively such cases with complications and contrive an operative technique to reduce complications.
Methods
Nineteen patients underwent cranioplasty and VP shunt operation due to large cranial defects and hydrocephalus. These patients were divided into two groups: Group A with 10 patients who underwent staged-operations, and Group B with 9 patients who underwent one-stage operation. Their complications in each group were retrospectively reviewed. Another five patients underwent a one-stage operation with temporary occlusion of the distal shunt catheter to improve on the technique and were categorized as Group C. Complications in these groups were compared and analyzed.
Results
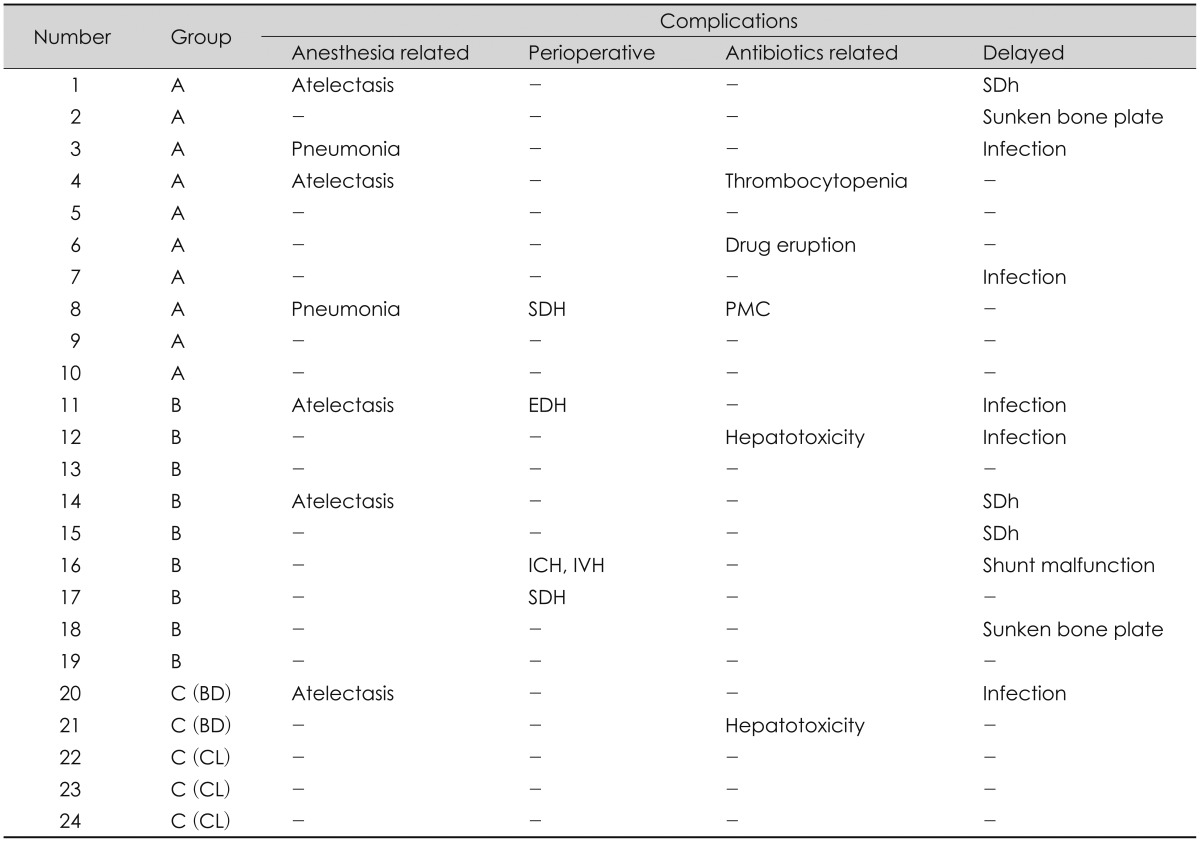
The results of the data analysis revealed that complications related to anesthesia (40%) and those related to antibiotic prophylaxis (30%) were high in Group A, while non-infectious delayed complications (45%) and perioperative complications such as intracranial hematoma (33%) were high in Group B. However, for patients in Group C, it showed less complication with the operative technique devised by these authors, as opposed to two previous procedures.
Decompressive craniectomy (DC) is one of the widely utilized imperative methods in the treatment of refractory intracranial hypertension. The benefits of DC, in the aspect of decreasing intracranial pressure (ICP), are well-documented in several studies.1345822) Furthermore, DC is known to improve cerebral compliance, cerebral oxygen supply, and cerebral perfusion pressure (CPP).412152729) With respect to operative technique, DC is a simple procedure. Nevertheless, there are numerous reported complications such as postoperative herniation through the cranial defect, subdural fluid collection, postoperative intracranial bleeding,1) postoperative infection, "syndrome of the trephined," and hydrocephalus.38111519242729)
In addition to the etiology that leads to having DC, a cranial defect alone may cause neurologic symptoms referred to as the "syndrome of the trephined" or "sinking skin flap syndrome." It is known to occur due to changes in the hydrodynamics of cerebrospinal fluid (CSF) in association with a postoperative cranial defect.382729) The "syndrome of the trephined" and hydrocephalus are the most frequent complications that develop after DC.3) It has been reported that the incidence rates of post-traumatic hydrocephalus, secondary to a head trauma, are in the range of 0.7% to 86%.611) It is known that the incidence rate of hydrocephalus, which may develop following DC, is about 10% to 40%.11428) The etiology of the hydrocephalus following DC may be not only post-traumatic but also original disease related hydrocephalus, such as post spontaneous subarachnoidal hemorrhagic hydrocephalus. In cases with hydrocephalus secondary to large craniectomy, they may require cranioplasty with a ventriculoperitoneal (VP) or a subdural-peritoneal (S-P) shunt. Patients would have a higher risk of complications by undergoing two procedures simultaneously than by undergoing each procedure in staged operations.18) However, patients undergoing staged operations also are imposed with considerable complications, such as having more chances of undergoing general anesthesia and surgical procedure, higher cost of surgery, longer hospital stay, and adverse reactions of antibiotic prophylaxis. In this study, these authors report an improved one-stage operation with minimization of complications associated with the aforementioned complications of one-stage or staged operations.
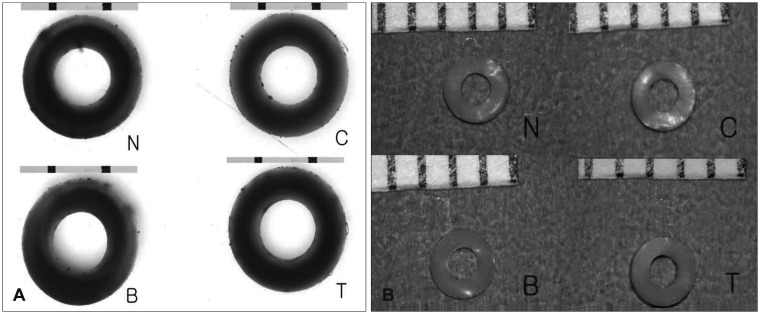
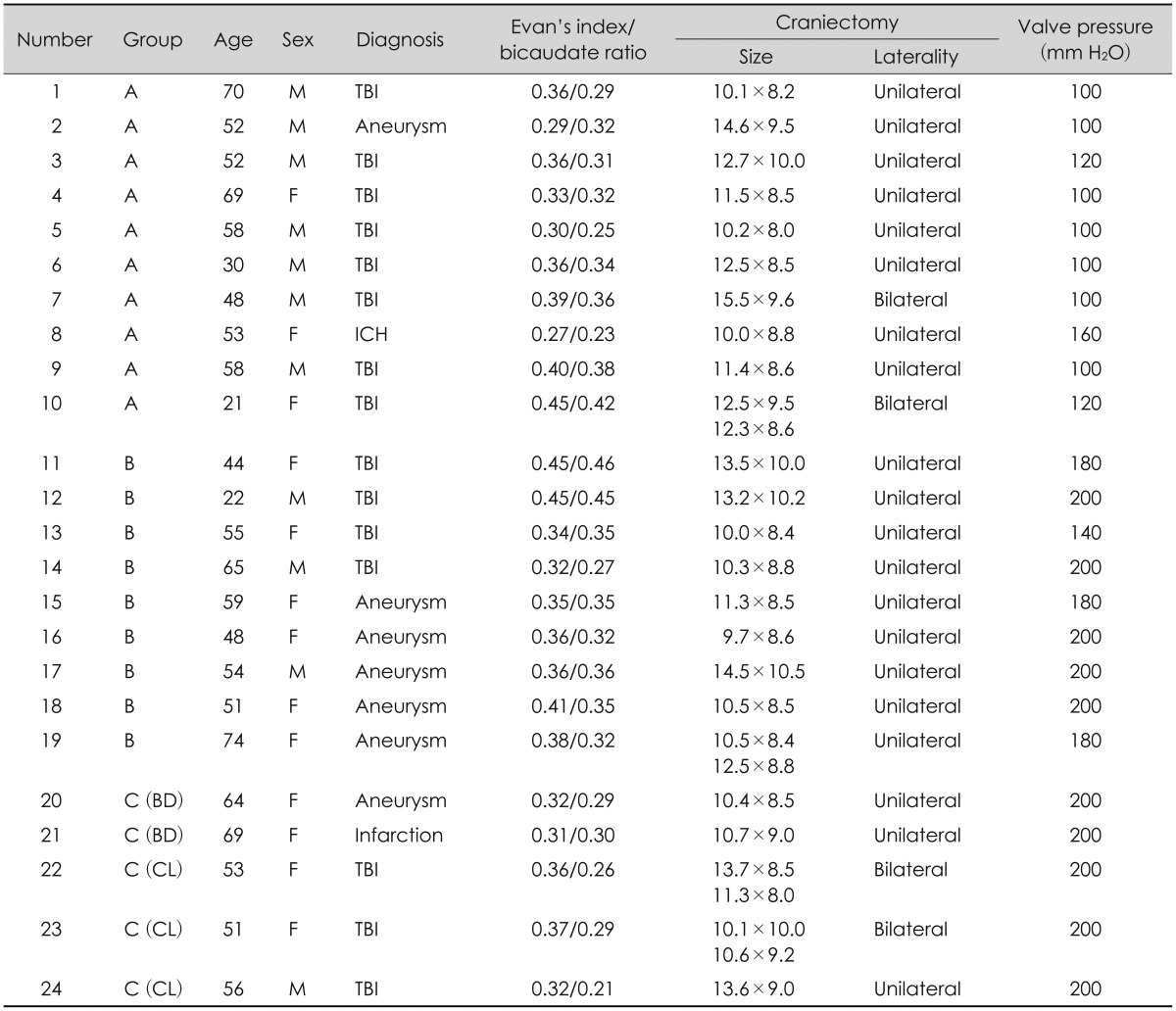
From May 2006 through December 2012, 91 patients underwent DC, due to refractory intracranial hypertension after they had suffered a traumatic brain injury or a vascular lesion, in our hospital. Furthermore, cranioplasty and CSF shunting operation were carried out for those patients that developed hydrocephalus. Of these 91 patients who underwent cranioplasty after DC, 23 received both cranioplasty and CSF shunt operation, and were reviewed, but 4 cases with an S-P shunt were excluded. The medical records of these 19 subjects were retrospectively investigated. These 19 patients were divided into two groups: the group of 10 patients who underwent staged-operations (Group A), and the group of 9 patients who underwent one-stage operation (Group B). Their complications in each group were retrospectively reviewed. From April 2013 through December 2014, another 5 patients underwent a one-staged operation with temporary occlusion of the distal shunt catheter to improve on the technique, and therefore were categorized as Group C. The complications in each group were compared and analyzed. This study also examined the following parameters: 1) age and sex, 2) size and laterality of cranial defects, and 3) clinical condition after surgery (Glasgow Outcome Scale). In this study, the hydrocephalus criteria were established as follows: 1) Evan's index >0.3, 2) bicaudate ratio >0.25 (means significant ventriculomegaly), 3) enlargement of the temporal horn or the third ventricle, 4) presence of periventricular low density, 5) clinical features, and 6) responses to preoperative continuous lumbar drainage (>150 mL/day). All patients underwent early cranioplasty (5 to 8 weeks after DC), while an autologous bone flap, which was kept at -80℃ in the bone bank, was utilized as the material for cranioplasty. After cranioplasty, using the ipsilateral Kocher's point or Keen's point (in case of bilateral cranioplasty, we used the right side), a VP shunt was performed. Only a programmable shunt valve type (Codman-Medos programmable VP shunt, Medos SA, Le Loche, Switzerland) was used in VP shunt implantation.6) Prior to surgery, owing to the possibility of temporary occlusion with the device affecting the mechanical structure of the shunt catheter wall, an experiment was carried out to find out whether any structural change of the shunt catheter wall could occur after occlusion. Complete occlusion was verified by infusing 10 mL of normal saline in a syringe into each of the following: 1) a case of occlusion with a Yasargil aneurysm clip (Aesculap Inc., South San Francisco, CA, USA), 2) a case of occlusion with a bulldog clamp (Lawton, Fridingen, Germany), and 3) a case of occlusion by making a direct tie of the shunt catheter with a black silk 4-0 suture material. Complete occlusion was verified in the above 2 cases, where saline passage was not observed even though strong positive pressure was applied with a syringe. Nevertheless, slight saline passage was evident when occlusion was carried out with an aneurysm clip. Then, the distal end of the clip blades was reinforced with a black silk tie, increasing the ending force, which resulted in complete occlusion (Figure 1). The distal shunt catheter was occluded by using 1) an aneurysm clip, 2) a bulldog clamp, and 3) by making a direct tie using a black silk 4-0 suture material. The slides of thin sections of the region, which had been occluded for 7 days in each case, were observed under an optical microscope (×100) and a surgical microscope (×13). These were compared with that of the normal shunt catheter for which nothing had been done. There was no difference between the wall structure of the above 3 shunt catheters and that of a normal shunt catheter (Figure 2). However, cutting the direct tie with a sharp knife could damage the wall integrity of the shunt catheter if the clip would be tied directly to the shunt catheter by a black silk suture material. Thus, a direct tie with a black silk suture material was not carried out in actual surgery. Three patients in Group C used a Yasargil aneurysm clip (Aesculap Inc., South San Francisco, CA, USA), which was used to occlude the distal aspect of the shunt catheter in the anterior chest area, and had their distal end of the clip tied to a black silk suture material to reinforce the ending force to occlude the catheter. Two patients in the same group used a bulldog clamp (Lawton, Fridingen, Germany) to occlude the shunt catheter. These attempts of temporary occlusion lasted for 5 to 7 days. During the cranioplasty, a subdural type ICP monitoring catheter (Camino, Integra LifeSciences, Plainsboro, NJ, USA) was placed below the edge of bone margin to monitor the ICP during the period of temporary occlusion. The initial pressure of the programmable shunt valve was set at 200 mm H2O and the ICP was allowed to drop gradually as these patients were followed up by brain computed tomography (CT).
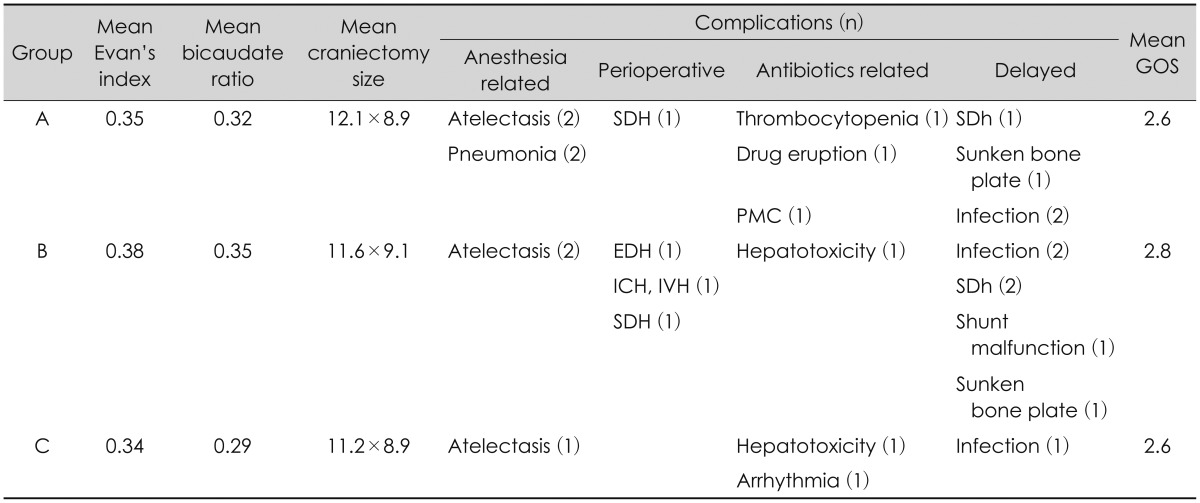
There were 11 males and 13 females while the mean age of these subjects was 53.1 years old with a range of 22 to 74 years. The etiologies of DC and CSF disorder included traumatic brain injury (13 cases), complicated clinical outcome after spontaneous subarachnoid hemorrhage secondary to cerebral aneurysmal rupture (9), malignant brain swelling following cerebral infarction (1), and spontaneous intracerebral hemorrhage (1). A unilateral cranial defect was observed in 20 patients, while a bilateral cranial defect was seen in 4 patients (Table 1). The mean sizes of cranial defect were 12.1×8.9 cm2 in Group A, 11.6×9.1 cm2 in Group B and 11.2×8.9 cm2 in Group C, respectively. There was no statistical difference in cranial defect size among groups. The preoperative hydrocephalus indices were as follows: 1) the mean Evan's index was 0.35 in Group A, 0.38 in Group B, and 0.34 in Group C; and 2) the bicaudate ratio was 0.32 in Group A, 0.35 in Group B, and 0.29 in Group C. The frequency of complications related to anesthesia (40%) and that of complications related to prophylactic antibiotics (30%) were high in Group A. The assumption is that high frequencies of development of these complications are due to more numbers of induction of general endotracheal anesthesia and operations as having staged operations. Patients in Group B had a higher frequency of perioperative complications (33%), such as intracranial hematomas and layed complications (45%), as opposed to those in other groups. Patients in Group C did not have significant complications in comparison with those of the other two groups have. Moreover, there was no significant difference in the incidences of postoperative infection among three groups (Tables 2 and 3).
The effectiveness of DC as a treatment approach to refractory intracranial hypertension, a consequence of failed medical treatment of traumatic brain injury or an intracranial vascular lesion, has been reported by several studies.1121425262729) Bor-Seng-Shu et al.4) reported their review article related to the contribution of DC in reducing ICP and increasing CPP among patients with refractory intracranial hypertension. They suggested that DC seems to be an effective treatment for reducing ICP and increasing CPP. Yamakami and Yamaura27) also reported a result of similar effects of DC with respect to increasing CPP. On the other hand, it was also reported that DC could exacerbate it by increasing focal cerebral blood flow, which might cause brain swelling.4102327) In addition, other post-DC complications may include: 1) perioperative complications such as expansion of contusion, new subdural and epidural hematomas contralateral to the decompressed hemisphere, and external cerebral herniation; and 2) delayed complications, such as subdural hygroma or wound infection.23) In the aspect of general brain protection and cosmesis, except for special cased, cranioplasty is the procedure indicated for almost all cases following DC.15) More recent reports have suggested that the rationale behind the performance of cranioplasty is not just a cosmetic matter but also therapeutic, through which cranioplasty helps to optimize neurological recovery.2391015212226) Fodstad et al.9) asserted in their report of 40 cases of cranioplasty that hydrodynamic changes of CSF before and after cranioplasty, including resting pressure, sagittal sinus pressure, buffer volume, elastance at resting pressure and pulse variations at resting pressure, are closely related to improvement of their symptoms after cranioplasty. Regardless, there have been quite a few literary considerations on various complications arising from post-DC cranioplasty.10131530) Gooch et al.10) analyzed the complications of cranioplasty following DC in their study of 62 cases of cranioplasty. They summarized postoperative wound infection, intracranial hematoma, bone resorption, sunken bone plate, intraoperative hemodynamic instability, deep vein thrombosis, etc. as complications that might develop after cranioplasty. The optimal time for cranioplasty after DC has not been determined yet. Previously, it is generally accepted that cranioplasty is carried out in 3 months after DC, but the procedures is performed 6 months after DC in cases of intracranial infection.20) Recently, however, there are reports that early cranioplasty of 5 to 8 weeks after DC can further facilitate neurologic recovery and also lead to less postoperative complications.1520) It is known that the frequency of hydrocephalus occurring in patients with large craniectomy is about 10 to 40%.11428) Pachatouridis et al.18) suggested that development of hydrocephalus after DC has been attributed to focal destructive lesions or ischemic insults, that lead to neuronal loss and severe atrophy of brain parenchyma, adhesive arachnoiditis of the basal cisterns, blood blocking and dysfunction of the arachnoid granulations, and gradient between the atmospheric pressure and ICP, which leads to inward displacement of the scalp and decrease of CSF flow over the convexity. In patients with a cranial defect and a CSF-circulation disorder, both cranioplasty and VP shunt operation may be necessary. It is known that performing two operations simultaneously has a higher risk of complications than performing them one at a time in staged operations.1318) Pachatouridis et al.18) also report that cranioplasty and ventriculostomy followed by a second stage placement of a VP shunt are associated with fewer complications in the treatment of hydrocephalus after DC. Oh et al.17) asserted in their report that the outcome of shunt operation after cranioplasty tends to be better than cranioplasty after shunt operation for patients with a large cranial defect and hydrocephalus. In patients with a severely depressed scalp flap after DC and VP shunt, there is a potential risk of developing an intracranial hematoma as a complication in performing cranioplasty. Liao and Kao16) tried to eliminate the dead space between the skull plate and the dura, and lessen the risk of complications related to intracranial hematoma that occurred secondary to cranioplasty. They suggested a method to minimize the dead space by inducing an expansion of the depressed brain. This was achieved by creating a temporary occlusion with an aneurysm clip in the distal catheter of the previously inserted VP shunt before they undertook cranioplasty. On the other hand, some authors reported that hydrocephalus in combination with a cranial defect can be generally treated with one-stage operations.730) Carvi and Höllerhage7) reported that cranioplasty combined with implementation of a shunt system allowed ICP changes to adjust dynamically after the procedures. The combined procedure reduced the number of required surgical procedures and complications. This study reviewed cases of one-stage operation of cranioplasty and shunt implantation, and cases of staged operation where each procedure was performed one at a time. Their complications were retrospectively examined and attempts were made to reduce complications that could develop in each. Complications of staged operation were associated with the number of general anesthesia and operation. Thus, both procedures were combined into a one-stage simultaneous operation to reduce these numbers. The complications, such as intracranial hematoma and subdural hygroma, which develop often in a one-stage operation, were prevented by blocking the CSF drainage (temporary occlusion of the distal shunt catheter). This would avert the sunken down effect of the brain. With respect to complications, such as intracranial hematoma or subdural hygroma that develops often in a one-stage operation, the assumption was that the risk of complications of one-stage operation could be reduced by preventing the sunken down effect of the brain through blocking CSF drainage, and thus inducing adhesion between the dura mater and cranium after cranioplasty. In an attempt to prevent neuronal damage secondary to hydrocephalus that might develop in this period, an ICP monitor-ing catheter was inserted during surgery. The plan was to aspirate CSF from the reservoir bag of the VP shunt system as needed, but there was no increased ICP to the extent of requiring aspiration in this study. The occlusion device could easily be removed by a simple procedure at bedside, and there was no particular effect on the wall structure of the shunt catheter as shown in observations. The shunt valve pressure was initially set at 200 mm Hg, and was gradually decreased as patients were followed up with brain CT. The results were satisfactory and no other complication was observed, except for a mild wound infection that was pharmacologically treated.
Despite these many positives, some limitations to our conclusions exist. One variable that could affect the nature of our results would be the selection bias such as surgeon related complications and indications in application of a Yasargil clip or a Bulldog clamp. Our study was not designed to clarify such limitations. Furthermore, the number of patients in Group C was too small to be a statistical analysis. So the results of this study was not enough to generalize. Therefore, future studies should be performed with a large number in Group C to validate these results. Prospective studies are further planned to confirm the effects of these procedures in patients with large cranial defects and CSFcirculation disorder. Further long-term follow-up studies with a large number of patients are necessary.
There are risks of complications in both one-stage operation and staged operations of cranioplasty and VP shunt procedure, performed for patients with a large cranial defect and hydrocephalus. These complications of the above two operative methods can be reduced by utilizing the technique of a "one-stage operation with temporary occlusion of the distal shunt catheter with an aneurysm clip or a micro bull dog clamp, together with slowly lowering the pressure of the programmable shunt valve." Our preliminary results indicate that our modified one staged operation technique can be an effective alternative method to overcome the disadvantage of one-stage operation of cranioplasty and the VP shunt system.
References
1. Aarabi B, Hesdorffer DC, Ahn ES, Aresco C, Scalea TM, Eisenberg HM. Outcome following decompressive craniectomy for malignant swelling due to severe head injury. J Neurosurg. 2006; 104:469–479. PMID: 16619648.

2. Agner C, Dujovny M, Gaviria M. Neurocognitive assessment before and after cranioplasty. Acta Neurochir (Wien). 2002; 144:1033–1040. discussion 1040PMID: 12382131.

3. Annan M, De Toffol B, Hommet C, Mondon K. Sinking skin flap syndrome (or Syndrome of the trephined): a review. Br J Neurosurg. 2015; 29:314–318. PMID: 25721035.

4. Bor-Seng-Shu E, Figueiredo EG, Amorim RL, Teixeira MJ, Valbuza JS, de Oliveira MM, et al. Decompressive craniectomy: a meta-analysis of influences on intracranial pressure and cerebral perfusion pressure in the treatment of traumatic brain injury. J Neurosurg. 2012; 117:589–596. PMID: 22794321.

5. Bullock R, Hanemann CO, Murray L, Teasdale GM. Recurrent hematomas following craniotomy for traumatic intracranial mass. J Neurosurg. 1990; 72:9–14. PMID: 2294191.

6. Cardoso ER, Galbraith S. Posttraumatic hydrocephalus--a retrospective review. Surg Neurol. 1985; 23:261–264. PMID: 3975808.

7. Carvi Y, Nievas MN, Höllerhage HG. Early combined cranioplasty and programmable shunt in patients with skull bone defects and CSF-circulation disorders. Neurol Res. 2006; 28:139–144. PMID: 16551430.
8. Czosnyka M, Copeman J, Czosnyka Z, McConnell R, Dickinson C, Pickard JD. Post-traumatic hydrocephalus: influence of craniectomy on the CSF circulation. J Neurol Neurosurg Psychiatry. 2000; 68:246–248. PMID: 10702038.

9. Fodstad H, Love JA, Ekstedt J, Fridén H, Liliequist B. Effect of cranioplasty on cerebrospinal fluid hydrodynamics in patients with the syndrome of the trephined. Acta Neurochir (Wien). 1984; 70:21–30. PMID: 6741628.

10. Gooch MR, Gin GE, Kenning TJ, German JW. Complications of cranioplasty following decompressive craniectomy: analysis of 62 cases. Neurosurg Focus. 2009; 26:E9. PMID: 19485722.

12. Hase U, Reulen HJ, Meinig G, Schürmann K. The influence of the decompressive operation on the intracranial pressure and the pressure-volume relation in patients with severe head injuries. Acta Neurochir (Wien). 1978; 45:1–13. PMID: 742427.

13. Heo J, Park SQ, Cho SJ, Chang JC, Park HK. Evaluation of simultaneous cranioplasty and ventriculoperitoneal shunt procedures. J Neurosurg. 2014; 121:313–318. PMID: 24655097.

14. Kan P, Amini A, Hansen K, White GL Jr, Brockmeyer DL, Walker ML, et al. Outcomes after decompressive craniectomy for severe traumatic brain injury in children. J Neurosurg. 2006; 105(5 Suppl):337–342. PMID: 17328254.

15. Liang W, Xiaofeng Y, Weiguo L, Gang S, Xuesheng Z, Fei C, et al. Cranioplasty of large cranial defect at an early stage after decompressive craniectomy performed for severe head trauma. J Craniofac Surg. 2007; 18:526–532. PMID: 17538313.

16. Liao CC, Kao MC. Cranioplasty for patients with severe depressed skull bone defect after cerebrospinal fluid shunting. J Clin Neurosci. 2002; 9:553–555. PMID: 12383414.

17. Oh CH, Park CO, Hyun DK, Park HC, Yoon SH. Comparative Study of Outcomes between Shunting after Cranioplasty and in Cranioplasty after Shunting in Large Concave Flaccid Cranial Defect with Hydrocephalus. J Korean Neurosurg Soc. 2008; 44:211–216. PMID: 19096679.

18. Pachatouridis D, Alexiou GA, Zigouris A, Michos E, Drosos D, Fotakopoulos G, et al. Management of hydrocephalus after decompressive craniectomy. Turk Neurosurg. 2014; 24:855–858. PMID: 25448200.
19. Phuenpathom N, Ratanalert S, Saeheng S, Sripairojkul B. Post-traumatic hydrocephalus: experience in 17 consecutive cases. J Med Assoc Thai. 1999; 82:46–53. PMID: 10087738.
20. Schimidek H. Operative neurosurgical technique: cranioplasty: indications, technique and prognosis. ed 4. Singapore: Elsevier Science;2000.
21. Segal DH, Oppenheim JS, Murovic JA. Neurological recovery after cranioplasty. Neurosurgery. 1994; 34:729–731. discussion 731PMID: 8008174.

22. Sobani ZA, Shamim MS, Zafar SN, Qadeer M, Bilal N, Murtaza SG, et al. Cranioplasty after decompressive craniectomy: an institutional audit and analysis of factors related to complications. Surg Neurol Int. 2011; 2:123. PMID: 22059118.

23. Stiver SI. Complications of decompressive craniectomy for traumatic brain injury. Neurosurg Focus. 2009; 26:E7. PMID: 19485720.

24. Waziri A, Fusco D, Mayer SA, McKhann GM 2nd, Connolly ES Jr. Postoperative hydrocephalus in patients undergoing decompressive hemicraniectomy for ischemic or hemorrhagic stroke. Neurosurgery. 2007; 61:489–493. discussion 493-494PMID: 17881960.

25. Whitfield PC, Patel H, Hutchinson PJ, Czosnyka M, Parry D, Menon D, et al. Bifrontal decompressive craniectomy in the management of posttraumatic intracranial hypertension. Br J Neurosurg. 2001; 15:500–507. PMID: 11814002.

26. Winkler PA, Stummer W, Linke R, Krishnan KG, Tatsch K. Influence of cranioplasty on postural blood flow regulation, cerebrovascular reserve capacity, and cerebral glucose metabolism. J Neurosurg. 2000; 93:53–61. PMID: 10883905.

27. Yamakami I, Yamaura A. Effects of decompressive craniectomy on regional cerebral blood flow in severe head trauma patients. Neurol Med Chir (Tokyo). 1993; 33:616–620. PMID: 7505400.

28. Yang XF, Wen L, Shen F, Li G, Lou R, Liu WG, et al. Surgical complications secondary to decompressive craniectomy in patients with a head injury: a series of 108 consecutive cases. Acta Neurochir (Wien). 2008; 150:1241–1247. discussion 1248PMID: 19005615.

29. Yang XJ, Hong GL, Su SB, Yang SY. Complications induced by decompressive craniectomies after traumatic brain injury. Chin J Traumatol. 2003; 6:99–103. PMID: 12659705.
30. Zhou Q, Zhang SZ, Xu RX, Wang JQ, Tu YY. [One-stage operation of ventriculo-peritoneal shunt and cranioplasty: analysis of 54 cases]. Di Yi Jun Yi Da Xue Xue Bao. 2005; 25:254–255. PMID: 15771986.
FIGURE 1
Photographs of occluded distal shunt catheter by using different occlusion devices. A: By making a direct tie of the shunt catheter with a black silk 4-0 suture material. B: By applying a Yasargil aneurysm clip. Note that the distal end of the clip blades is reinforced with a black silk tie to increase the ending force. C: With a bulldog clamp.
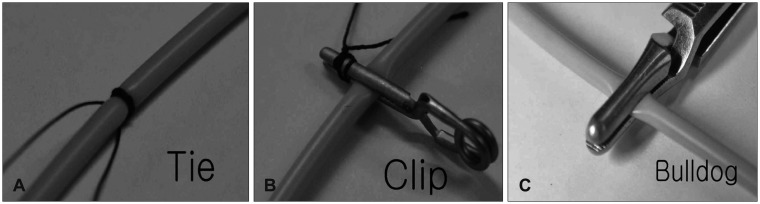
FIGURE 2
The slides of thin sections of the region, which have been occluded for 7 days, are observed under an optical microscope (×100) (A) and a surgical microscope (×13) (B). Note that there is no difference between the wall structure of the 3 differently occluded shunt catheters and that of a normal shunt catheter. N: none occluded, C: clipped, B: bulldog clamped, T: tied.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download