Abstract
Background
Normal pressure hydrocephalus (NPH) is a poorly understood condition, which typically presents with the triad of gait disturbance, urinary incontinence and cognitive decline. Diagnosis of NPH is often challenging due to its varied presentation and overlap with other neurodegenerative diseases including multiple system atrophy (MSA).
Case Report
A 68-year-old male developed rapidly progressive gait difficulty, urinary incontinence and memory impairment. Neurologic examination showed parkinsonism affecting the right side and impaired postural reflexes. Brain MRI showed enlargement of the ventricles and narrowing of the high convexity cerebrospinal fluid (CSF) spaces with relative dilated Sylvian fissure, the supporting features of NPH. 18F-fluorinated-N-3-fluoropropyl-2-b-carboxymethoxy-3-b-(4-iodophenyl) nortropane (18F-FP-CIT) PET showed decreased FP-CIT binding in the left posterior putamen and 18F-fluorodeoxyglucose PET showed decreased metabolism in the left basal ganglia, consistent with findings of MSA. CSF removal was performed and the symptoms were improved. The patient underwent ventriculo-peritoneal shunt and his gait and cognition improved.
Normal pressure hydrocephalus (NPH) usually presents with progressive dementia, gait disturbance, and urinary incontinence. The usual treatment includes installation of a shunt to drain excess cerebrospinal fluid (CSF) into the peritoneum. This treatment can reverse the symptoms and restore normal functioning.1 However, it is difficult to diagnose NPH because the symptoms are common to several other diseases including Parkinson's disease and multiple system atrophy (MSA).
MSA is a rare and presumably sporadic neurodegenerative disorder, and it is clinically characterized by a combination of parkinsonian, autonomic, cerebellar, or pyramidal signs. The motor symptoms in MSA are highly resistant to pharmacologic treatment. In addition, no effective disease-modifying or neuroprotective treatment is available for MSA.2 Therefore, it is important to differentiate this condition from other treatable diseases. We report a case of a MSA patient with coexistent hydrocephalus who improved after CSF drainage and underwent ventriculo-peritoneal (VP) shunt operation.
A 68-year-old male was admitted with a one-year history of progressive difficulty in walking. Parkinson's syndrome had been diagnosed by a neurologist who commenced treatment with levodopa, but despite the medication his walking continued to deteriorate. Three months before admission, he had numerous falls and developed urinary incontinence.
On neurologic examination, the patient's cognitive function was impaired (Korean Mini-Mental Status Examination score 17 out of 30). He showed parkinsonism features such as bradykinesia with rigidity and tremor predominant on the right side of the body. Tendon reflexes were normal, without bilateral extensor plantar responses. He showed a short-stride gait. His postural reflexes were impaired. There was no significant orthostatic blood pressure decline. He did not show any cerebellar symptoms. Autonomic failure involving urinary incontinence and poorly levodopa-responsive parkinsonism satisfied the requirements of criteria for the diagnosis of probable MSA with predominant parkinsonism (MSA-P).2
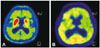
Hematological and biochemical screening and chest X-ray were normal. A brain MRI scan showed enlargement of the ventricles and narrowing of the high convexity CSF spaces with relative dilated Sylvian fissures (Fig. 1). The Evans ratio was 0.38 (Fig. 1B). There was no atrophy on the MRI scan of the putamen, middle cerebellar peduncle, pons, or cerebellum, as seen in MSA (Fig. 1). Further 18F-fluorinated-N-3-fluoropropyl-2-b-carboxymethoxy-3-b-(4-iodophenyl) nortropane positron emission tomography (18F-FP-CIT PET) neuroimaging study showed asymmetrically decreased FP-CIT binding in the left posterior putamen (Fig. 2A). 18F-fluorodeoxyglucose positron emission tomography (18F-FDG PET) demonstrated decreased metabolism in the left basal ganglia and preserved metabolism in the brainstem and cerebellum (Fig. 2B).
The patient was initially diagnosed with probable MSA-P based on the revised diagnostic criteria set forth in the 2008 MSA second consensus statement.2 Although the patient's clinical symptoms such as poorly levodopa responsive parkinsonism with autonomic failure and neuroimaging findings were consistent with MSA, there was a possibility that the patient's worsening gait, cognitive impairment, and urinary incontinence could be caused by the coexisting NPH. Therefore, 50 mL of CSF removal was performed. Cerebrospinal fluid pressure and contents were normal. After CSF drainage, the patient showed improvement in timed gait, although cognitive parameters remained in the abnormal range (Table 1). The patient also emphasized that he was more comfortable walking after CSF drainage. On the basis of this outcome, NPH could be responsible for the patient's gait and memory impairment, and VP shunt operation was performed, despite underlying MSA. At two weeks post-operatively, his gait and cognitive parameters were improved (Table 1).
We report a case of a patient in whom a diagnosis of MSA and NPH was considered and who showed a dramatic response to CSF drainage and VP shunt. Initially, our patient presented with gait disturbance, parkinsonism and urinary incontinence, which are the clinical features commonly associated with MSA. Functional neuroimaging findings that indicated decreased 18F-FP-CIT binding on dopamine transporter imaging and hypometabolism of the putamen on 18F-FDG PET supported the diagnosis of MSA. However, because the patient had cognitive impairment and a higher Evans index, which are the supporting features of NPH, CSF drainage was attempted and the symptoms were improved.
NPH is a potentially treatable neurological disorder in older adults, involving disturbances of gait and balance, control of micturition, and cognition (so-called classic triad of symptoms of the disease) in combination with enlargement of the cerebral ventricles. Gait and balance disturbances are the most common presenting findings and may occur alone or together with cognitive and urinary symptoms. However, diagnosis of NPH is often challenging because of its varying presentation and overlap with other disorders common in the elderly such as neurodegenerative diseases including MSA. Furthermore, not all patients show the classic triad of symptoms. In addition, some patients often present with signs of movement disorders such as parkinsonism. Therefore, some patients have been treated with inadequate therapy. Previous studies have reported the post-mortem findings of 38 patients who had been clinically diagnosed with idiopathic NPH with vascular changes (71%), Alzheimer's disease (AD) (61%), and progressive supranuclear palsy (PSP) (2.6%), which were the most frequent co-existing pathologies.34 Some of the NPH patients with pathologic findings of PSP and AD also had a successful shunt procedure; thus raising questions about the accuracy of diagnosis in these particular cases.56 Thus, if hydrocephalus is found in neurodegenerative disease with gait disturbance, the possibility of accompanying NPH should be considered. In this patient, disproportion between narrowing of the CSF space at the high convexity and dilatation of the Sylvian fissure on brain MRI may serve as an important imaging marker for NPH.7
In this patient, one of the most important reasons for the possibility of NPH is the presence of cognitive impairment. Traditionally, it has been thought that obvious dementia is not a feature of MSA. Usually, neurodegenerative diseases which regularly present with co-occurring parkinsonism and dementia are idiopathic Parkinson's disease (with dementia), dementia with Lewy bodies, PSP, and corticobasal degeneration syndrome. In addition, vascular parkinsonism and NPH are often accompanied by parkinsonism and dementia. But, recent studies have shown that dementia occurs in patients with MSA up to a rate of 31%, and dementia has been reported even in patients with pathologically-proven MSA.8 However, in this patient, clinical improvement of cognitive dysfunction after VP shunt placement suggests that cognitive impairment is associated with NPH rather than MSA.
NPH is a potentially treatable neurological disorder. Therefore, it is important to diagnose and differentiate it from other treatment-resistant neurodegenerative diseases, and this neurodegenerative disease was MSA in our patient. When hydrocephalus and clinical features of NPH are present in neurodegenerative disease with gait disturbance, the possibility of accompanying NPH should be suspected and performing CSF removal for shunt responsiveness should be considered.
Figures and Tables
Fig. 1
Fluid-attenuated inversion recovery image of the patient. Enlargement of the ventricles and disproportion between narrowing of the CSF spaces at the high convexity and dilatation of the Sylvian fissures (A and B) were consistent with the imaging features of NPH. There was no atrophy of the putamen, middle cerebellar peduncle, pons, or cerebellum, as seen in MSA (C and D). CSF: cerebrospinal fluid, MSA: multiple system atrophy, NPH: normal pressure hydrocephalus.

Fig. 2
18F-FP-CIT PET and 18F-FDG PET images of the patient. A: 18F-FP-CIT PET image showed asymmetrically decreased FP-CIT binding in the left posterior putamen. B: 18F-FDG PET image demonstrated decreased metabolism in the left basal ganglia and preserved metabolism in the brainstem and cerebellum. 18F-FDG PET: 18F-fluorodeoxyglucose positron emission tomography, 18F-FP-CIT PET: 18F-fluorinated-N-3-fluoropropyl-2-b-carboxymethoxy-3-b-(4-iodophenyl) nortropane positron emission tomography.
References
1. Hakim CA, Hakim R, Hakim S. Normal-pressure hydrocephalus. Neurosurg Clin N Am. 2001; 12:761–773. ix

2. Gilman S, Wenning GK, Low PA, Brooks DJ, Mathias CJ, Trojanowski JQ, et al. Second consensus statement on the diagnosis of multiple system atrophy. Neurology. 2008; 71:670–676.

3. Leinonen V, Koivisto AM, Savolainen S, Rummukainen J, Sutela A, Vanninen R, et al. Post-mortem findings in 10 patients with presumed normal-pressure hydrocephalus and review of the literature. Neuropathol Appl Neurobiol. 2012; 38:72–86.

4. Cabral D, Beach TG, Vedders L, Sue LI, Jacobson S, Myers K, et al. Frequency of Alzheimer's disease pathology at autopsy in patients with clinical normal pressure hydrocephalus. Alzheimers Dement. 2011; 7:509–513.

5. Curran T, Lang AE. Parkinsonian syndromes associated with hydrocephalus: case reports, a review of the literature, and pathophysiological hypotheses. Mov Disord. 1994; 9:508–520.

6. Magdalinou NK, Ling H, Smith JD, Schott JM, Watkins LD, Lees AJ. Normal pressure hydrocephalus or progressive supranuclear palsy? A clinicopathological case series. J Neurol. 2013; 260:1009–1013.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download