Abstract
Background and Purpose
Wandering is one of the most common behavioral and psychological symptoms of dementia, and associated with some of the adverse outcomes in dementia, such as getting lost or even death. The etiology of wandering is not yet clearly known. As depression and wandering are both very common among the patients with dementia, this study examined the relationship between the depression and wandering among the community dwelling patients with dementia.
Methods
Fifty community dwelling patients diagnosed with dementia were included in this study if they had primary family caregiver, older than age 18 in Seoul, South Korea. The Geriatric Depression Scale, Korean Version (GDS-K), Korean Version of the Mini-Mental State Examination (K-MMSE) and Korean Version of Revised Algase Wandering Scale-Community Version (K-RAWS-CV) were used to measure the severity of depression, cognitive function and wandering.
Results
Thirty percents of the patients showed wandering. Mean score of GDS-K was significantly higher in wanderers than non-wanderers. Severity of depression was significantly correlated with the total score of K-RAWS-CV and subscales of persistent walking, repetitive walking, eloping behavior, and mealtime impulsivity in whole sample. K-MMSE score also was related to wandering behavior. The prevalence odds ratio for wandering in depressed patients compared with undepressed group was 8.386 (95% confidence interval: 1.978–35.561).
Wandering is one of the most common and exhausting behavioral and psychological symptoms of dementia for caregivers.1 Also, it has adverse outcomes on patient such as getting lost,2 malnutrition,1 weight loss,3 fatigue, sleep disturbance,4 social isolation,5 earlier institutionalization,6 and injury.7 The term 'wandering' is frequently used as a broad term encompassing a diverse set of behaviors and is often considered as a kind of agitated behavior.8 In 2007, a scientific definition of wandering was suggested as 'a syndrome of dementia-related locomotion behavior having a frequent, repetitive, temporally-disordered, and/or spatially-disoriented nature that is manifested in lapping, random, and/or pacing patterns, some of which are associated with eloping, eloping attempts, or getting lost unless accompanied'.9
Previous studies estimated the rates of wandering as 17.4% in community dwelling patients with dementia,10 18.7% in drug-naïve Alzheimer disease patients,11 21% to 67.5% in nursing home residents.121314 Longitudinal studies indicate that wandering behavior starts on the average 10 months after diagnosis of dementia in 40% of individuals,15 but eventually occurs in 80% of all patients with dementia.16 In a large, multiethnic sample of community-dwelling patients, wandering was the most prevalent dementia-related behavior regardless of the ethnicity.17
Yet the etiology of wandering remains unsolved, there are three main approaches: biological, psychosocial, and person-environment interaction.18 A biological hypothesis includes the dysfunction of right parietal dysfunction, spatial perception and memory,1920 impairments in visual attention and an optic flow perception,2122 execution problem from thoughts to actions,23 and the wayfinding difficulties.2425
The need-driven dementia-compromised behavior (NDB) model explains how wandering results from the interaction of background and proximal factors.26 Background factors constitute relatively stable characteristics of the person with dementia, such as cognitive status, health condition, and personal characteristics, including depression. Proximal factors are more fluid or dynamic features of the person and of the immediate environment such as physiological need states, social and physical environment.27 Both background and proximal factors interact or combine to produce NDBs including wandering. Particularly there are a few studies found that wandering was associated with depression.1101628
Several studies support the relationship between emotions and behaviors in dementia2930 and implicate the correlation between mood states (e.g., depression and anxiety) and problematic behaviors including wandering.193132 Specifically, basal ganglia and amygdala, which are related to emotional functions, are relatively conserved along the progression of Alzheimer's disease.33 Neuroimaging studies also demonstrated preserved glucose utilization in primary sensory and motor cortex, the basal ganglia, the thalamus, and the cerebellum, while decreased glucose utilization in in higher cortical regions.3435 Clinically, Alzheimer disease patients with depression showed higher rates of wandering than those without depression,31 anxiety symptoms were also positively correlated with wandering.1932 One study showed that positive environmental valence may reduce a wanderer's walking.36 Because brain pathways processing emotions are relatively spared in dementias like Alzheimer's disease,33343537 emotion may become predominant factor in determining the behavior of patients with dementia, especially as dementia progresses and the influence of cognition on emotion is weakened.38
Not only cognitive factors, emotional factors are also important in understanding wandering behaviors of patients with dementia, and it becomes more important as cognitive function decline. Especially, depression is known for its association with wandering, but the detailed aspects of how wandering is related with depression is not well known yet. The present study examined the relationship between depression and wandering by assessing wandering behavior in organized method.
The current study explored the relationship between depression and wandering by analyzing the questionnaire collected by interviewing the patient with dementia and the caregiver. This study used a cross-sectional design. Participants were patients with dementia who visited Korea University Anam Hospital or Gangbuk-gu center for dementia, in Seoul, Korea from July, 2014 to February, 2015. The study was approved by institutional review boards at Korea University Anam Hospital. Patients were measured for cognitive function and depression. The caregivers were interviewed for the wandering of the patients.
This study recruited 50 patients who met the following criteria: 1) were aged 65 years or older; 2) met the Diagnostic and Statistical Manual of Mental Disorders 4th edition revision criteria for diagnosis of dementia; 3) were ambulatory. The inclusion criteria for caregivers of the patients with dementia were: 1) a relative (over the age of 18); 2) serving as primary caregiver and has an intimate knowledge of that person over time; and 3) agreed to be interviewed.
The patient's cognitive impairment, wandering status, and severity of depression were measured. Severity of cognitive impairment was measured using the Korean Version of the Mini-Mental State Examination (K-MMSE). The MMSE has become a widely used, well-accepted measure for assessing cognitive status in research and clinical practice. Level of global cognitive impairment by MMSE is on a scale from 0 to 30.
Wandering status of the patients was measured through interviewing the caregivers using the Korean Version of Revised Algase Wandering Scale-Community Version (K-RAWS-CV). K-RAWS-CV is a translated and validated form of RAWS-CV.39 The RAWS-CV40 is an expanded version of the Algase Wandering Scale version 2, containing items that were reworded to apply community living along with new items generated by research team based on their collective clinical and research experience and literature review to quantify wandering behavior of community residing elders. The RAWS-CV, 39 items, has a five-point Likert scale (1 'never/unable' to 5 'always'). There are six subscales including persistent walking (PW), repetitive walking (RW), spatial disorientation (SD), eloping behavior (EB), negative outcomes (NO), and mealtime impulsivity (MI). Total overall range of scores for six subscales is 39–190, higher scores meaning more wandering; individual subscale scores range from 14–0 for PW; 7–35 for RW; 8–40 for EB; 4–20 for SD; 4–20 for NO; and 2–10 for MI. Mean item scores are used in analysis. As an additional item to K-RAWS-CV, a single question ('Is this person a wanderer?') was asked to caregivers to measure four levels of wandering: 1) not a wanderer; 2) wanderes at times; 3) yes, but not problematic wanderer; and 4) yes, and problematic wanderer. Because of the small size of sample, the item was dichotomized into non-wanderers (answer category 1) and wanderers (answer categories 2–4), and the number of patient in each group was 35 and 15, respectively.
Severity of depression of patients with dementia was measured by Geriatric Depression Scale, Korean Version (GDS-K). The GDS-K is validated as a reliable and valid tool for screening major depression depression among the elderly patients in Korea.41 In this study, the score '17' was suggested as the optimal cut-off point of GDS-K for screening major depressive disorder. Patients are divided into depressed and non-depressed by using the optimal cut-off point '17'.
Statistical analysis was performed using the IBM Statistical Package for the Social Science software WIN version 20.0.0 (Chicago, IL, USA). Comparison of the baseline characteristics between wanderers and non-wanderers were performed using the chi-square test for categorical variables, and the Student's t-test or Mann-Whitney test for quantitative variables, with normality verified by the Shapiro-Wilk test of normality. Similar analysis was done for the comparison between depressed and non-depressed group. Cross-sectional associations between 1) K-RAWS-CV and GDS-K; 2) K-RAWS-CV and MMSE-K; 3) each subscales of K-RAWS-CV and GDS-K; 4) each subscales of K-RAWS-CV and MMSE-K were determined by the Pearson's correlation coefficient. K-RAWS-CV total score was further explored by multiple linear regression, with GDS-K and MMSE-K. Additionally, the interaction between GDS-K and MMSE-K was explored after standardizing the variables using multiple linear regression. Logistic regression analysis was done to assess relationships between GDS-K and wandering after adjusting for K-MMSE. Statistical significance was considered when p-value was less than 0.05.
The study participants had a mean age of 76.6 years, and there were no gender difference. Means (standard deviations) for the K-MMSE, GDS-K, and K-RAWS-CV were 17.92 (4.92), 12.94 (8.36), and 1.623 (0.62), respectively. The rate of wandering among the community-dwelling elders with dementia was 30 percent. As seen in Table 1, GDS-K score was significantly higher in wanderers than non-wanderers (p<0.05). Age, gender, score of K-MMSE, and its subscales were not significantly different between wanderers and non-wanderers.
Table 2 shows the wandering rate in depressed group was significantly higher than non-depressed group (p<0.001) after dividing the patients into depressed group and non-depressed group. There was no difference in age, gender, K-MMSE, and its subscales between depressed group and non-depressed group. The total score of K-RAWS-CV and its subscales including PW, RW, EB, and MI was significantly higher in depressed group than non-depressed group (p<0.01). Wanderers (adjusted prevalence odds ratio 8.386, 95% confidence interval: 1.978–35.561) had significantly higher odds of wandering compared to non-wanderers after adjusting the K-MMSE.
Correlation analysis of K-RAWS-CV in whole patients showed positive correlation with GDS-K (r=0.432, p=0.002) (Fig. 1A), and negative correlation with K-MMSE (r=-0.432, p=0.002) (Fig. 1B). Table 3 shows positive correlation of GDS-K with the subscales of K-RAWS-CV including PW, RW, EB, and MI, whereas K-MMSE showed negative correlation with the subscales of K-RAWS-CV including PW, RW, EB, SD, and NO. Multiple linear regression analysis confirmed that above associations of K-RAWS-CV with GDS-K and K-MMSE were statistically significant (p=0.001 and p=0.001 respectively) (Table 4). The multiple linear regression analysis for interaction between GDS-K and K-MMSE showed that the lower the K-MMSE score, the correlation between GDS-K and K-RAWS-CV become stronger, however was statistically insignificant (β=-4.621, p=0.113).
The present study estimated the rate of wandering as 30% in community-dwelling elders with dementia. Previous researches demonstrated 18.7% of drug-naïve community-dwelling Alzheimer's disease patients are wanderer,11 and 67.5% of nursing-home residing dementia patients are wanderer.14 These results are constant with a study that wandering behavior leads familial caregivers decide to place the patient in a nursing home or some other professional care facility.42
Recent study demonstrated that memory recall, language among the subscales of MMSE and Rey-Osterrieth Complex Figure Test, first-edge-arm, and alternating hand among the subscales of Seoul neuropsychological screening battery was significantly lower in wandering group.11 In present study, K-MMSE and its subscales showed no difference between wanderers and non-wanderers in this study. Limited number of participants in this study can be considered as the difference from the previous study. However in whole patients, K-MMSE score showed correlation with K-RAWS-CV which is constant with the previous studies that cognitive dysfunction is related with wandering.1116192043 Specifically, K-MMSE score was correlated with PW, RW, EB, SD, NO among the subscales of K-RAWS-CV.
In the present study, GDS-K scores were significantly higher in wanderers than non-wanderers, and K-RAWS-CV was correlated with GDS-K in whole patients. These results were consistent with previous researches1031 implicated that depression is associated with depression, and clinically, depressed patients with dementia are more likely to wander than those who are not depressed. Additionally, GDS-K was correlated with PW, RW, EB, MI among the subscales of K-RAWS-CV. Interestingly, GDS-K was different from K-MMSE that GDS-K showed correlation with MI and was not correlated with SD and NO. Possible explanation is that depression is associated with wandering in ways of showing impulsive behaviors during mealtime whereas impaired cognitive function is associated with wandering in ways of deficits in way-finding or visuospatial cognitive functions and actual NO of wandering such as fracture or injury. Both depression and impaired cognitive function are associated with the persistent and RW behaviors and EBs such as trying to get out of house.
The interaction between GDS-K and K-MMSE was not statistically significant, however the degrees of correlation between GDS-K and K-RAWS-CV was stronger in patients with lower K-MMSE scores. Of interest is whether decline in cognitive function along with the progression of dementia would increase the influence of emotion on wandering behavior. Previous studies suggests that emotion may become predominant factor in determining the behavior of patients with dementia as the disease progresses.3334353738
The limitation of the present study is that the sample size was small. Therefore, patients were not grouped into specific diseases. As wandering is known to be more frequent in Alzheimer's disease than in vascular dementia or other types of dementia,10 further study on wandering according to the dementia types is required. Moreover, the effect of depression management on wandering was not considered in the present study. Since there is very little data about pharmacological management of wandering including antidepressants or mood stabilizers,18 a more careful study about the efficacy of managing the depression on wandering is required.
Despite these limitations, the present study demonstrated that depression is significantly correlated with wandering, especially in other ways than the cognitive dysfunction is. The present study emphasizes to Clinicians and other health care workers such as nurses dealing with the demented patients, that evaluation of depression is required in wandering patients.
Figures and Tables
Fig. 1
The correlation of the score of K-RAWS-CV with (A) GDS-K (r=0.432, p=0.002) and (B) K-MMSE (r=-0.432, p=0.002). GDS-K: Geriatric Depression Scale, Korean Version, K-MMSE: Korean Version of the Mini-Mental State Examination, K-RAWS-CV: Korean Version of Revised Algase Wandering Scale Community Version.

Table 1
Baseline characteristics of community-dwelling elders with dementia (means and standard deviations)
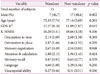
Table 2
Comparison of demographic characteristics, cognitive functions and wandering between depressed and non-depressed (means and standard deviations)

References
1. Rolland Y, Gillette-Guyonnet S, Nourhashémi F, Andrieu S, Cantet C, Payoux P, et al. [Wandering and Alzheimer’s type disease. Descriptive study. REAL.FR research program on Alzheimer’s disease and management]. Rev Med Interne. 2003; 24:Suppl 3. 333s–338s.

2. Gurwitz JH, Sanchez-Cross MT, Eckler MA, Matulis J. The epidemiology of adverse and unexpected events in the long-term care setting. J Am Geriatr Soc. 1994; 42:33–38.
3. Morley JE. Nutrition assessment is a key component of geriatric assessment. In : Vellas B, Guigoz Y, Garry P, Albarede J, editors. Facts and Research in Gerontology. 3rd ed. Paris: Serdi Publishing Company;1997. p. 5–10.
4. Yang CH, Hwang JP, Tsai SJ, Liu CM. Wandering and associated factors in psychiatric inpatients with dementia of Alzheimer’s type in Taiwan: clinical implications for management. J Nerv Ment Dis. 1999; 187:695–697.

5. Beattie ER, Song J, LaGore S. A comparison of wandering behavior in nursing homes and assisted living facilities. Res Theory Nurs Pract. 2005; 19:181–196.

6. Phillips VL, Diwan S. The incremental effect of dementia-related problem behaviors on the time to nursing home placement in poor, frail, demented older people. J Am Geriatr Soc. 2003; 51:188–193.
7. Aud MA. Dangerous wandering: elopements of older adults with dementia from long-term care facilities. Am J Alzheimers Dis Other Demen. 2004; 19:361–368.
8. Dawson P, Reid DW. Behavioral dimensions of patients at risk of wandering. Gerontologist. 1987; 27:104–107.

9. Algase DL, Moore DH, Vandeweerd C, Gavin-Dreschnack DJ. Mapping the maze of terms and definitions in dementia-related wandering. Aging Ment Health. 2007; 11:686–698.

10. Klein DA, Steinberg M, Galik E, Steele C, Sheppard JM, Warren A, et al. Wandering behaviour in community-residing persons with dementia. Int J Geriatr Psychiatry. 1999; 14:272–279.
11. Yang Y, Hwang I, Kwak YT. Neuropsychological characteristics of wandering in patients with drug-naive Alzheimer’s disease. Dement Neurocognitive Disord. 2014; 13:74–78.
12. Schonfeld L, King-Kallimanis B, Brown LM, Davis DM, Kearns WD, Molinari VA, et al. Wanderers with cognitive impairment in Department of Veterans Affairs nursing home care units. J Am Geriatr Soc. 2007; 55:692–699.

14. Song JA, Lim YM, Hong GR. Wandering behavior in Korean elders with dementia residing in nursing homes. J Korean Acad Nurs. 2008; 38:29–38.

15. Jost BC, Grossberg GT. The evolution of psychiatric symptoms in Alzheimer’s disease: a natural history study. J Am Geriatr Soc. 1996; 44:1078–1081.

16. Hope T, Keene J, McShane RH, Fairburn CG, Gedling K, Jacoby R. Wandering in dementia: a longitudinal study. Int Psychogeriatr. 2001; 13:137–147.

17. Sink KM, Covinsky KE, Newcomer R, Yaffe K. Ethnic differences in the prevalence and pattern of dementia-related behaviors. J Am Geriatr Soc. 2004; 52:1277–1283.

20. McShane R, Gedling K, Keene J, Fairburn C, Jacoby R, Hope T. Getting lost in dementia: a longitudinal study of a behavioral symptom. Int Psychogeriatr. 1998; 10:253–260.
21. Kavcic V, Duffy CJ. Attentional dynamics and visual perception: mechanisms of spatial disorientation in Alzheimer’s disease. Brain. 2003; 126(Pt 5):1173–1181.
22. Tetewsky SJ, Duffy CJ. Visual loss and getting lost in Alzheimer’s disease. Neurology. 1999; 52:958–965.

23. Benton AL. Disorders of spatial Orientation. In : Wincken PJ, Bruyn GW, editors. Handbook of Clinical Neurology. Amsterdam: North Holland;1969.

24. Passini R, Rainville C, Marchand N, Joanette Y. Wayfinding in dementia of the Alzheimer type: planning abilities. J Clin Exp Neuropsychol. 1995; 17:820–832.
25. Lim YM, Hong GR, Song JA. Correlation of way-finding and wandering in Korean elders with dementia at home. J Korean Gerontol Soc. 2008; 28:69–86.
26. Algase DL, Beck C, Kolanowski A, Whall A, Berent S, Richards K, et al. Need-driven dementia-compromised behavior: An alternative view of disruptive behavior. Am J Alzheimers Dis Other Demen. 1996; 11:10–19.

27. Nelson AL, Algase DL. Evidence-based protocols for managing wandering behaviors. New York: Springer Publishing;2007.

28. Kiely DK, Morris JN, Algase DL. Resident characteristics associated with wandering in nursing homes. Int J Geriatr Psychiatry. 2000; 15:1013–1020.

29. Bartol MA. Dialogue with dementia: nonverbal communication in patients with Alzheimer’s disease. J Gerontol Nurs. 1979; 5:21–31.

30. Mayhew M. The growing challenge of Alzheimer disease part 2. J Nurse Pract. 2005; 1:149–156.
31. Lyketsos CG, Steele C, Baker L, Galik E, Kopunek S, Steinberg M, et al. Major and minor depression in Alzheimer’s disease: prevalence and impact. J Neuropsychiatry Clin Neurosci. 1997; 9:556–561.
32. Teri L, Ferretti LE, Gibbons LE, Logsdon RG, McCurry SM, Kukull WA, et al. Anxiety of Alzheimer’s disease: prevalence, and comorbidity. J Gerontol A Biol Sci Med Sci. 1999; 54:M348–M352.
33. Eldridge LL, Masterman D, Knowlton BJ. Intact implicit habit learning in Alzheimer’s disease. Behav Neurosci. 2002; 116:722–726.
34. Parks RW, Haxby JV, Grady CL. Positron emission tomography in Alzheimer's disease. In : Parks RW, Zec RF, Wilson RS, editors. Neuropsychology of Alzheimer's disease and other dementias. New York: Oxford University Press;1993. p. 459–488.

35. Mielke R, Heiss WD. Positron emission tomography for diagnosis of Alzheimer’s disease and vascular dementia. J Neural Transm Suppl. 1998; 53:237–250.

36. Yao L, Algase D. Environmental ambiance as a new window on wandering. West J Nurs Res. 2006; 28:89–104.

37. Morris R. The cognitive neuropsychology of Alzheimer-type dementia. Oxford: Oxford University Press;1996.

38. Yao L, Algase D. Emotional intervention strategies for dementia-related behavior: a theory synthesis. J Neurosci Nurs. 2008; 40:106–115.
39. Son GR, Song J, Lim Y. Translation and validation of the Revised-Algase Wandering Scale (community version) among Korean elders with dementia. Aging Ment Health. 2006; 10:143–150.
40. Algase DL, Son GR, Beattie E, Song JA, Leitsch S, Yao L. The interrelatedness of wandering and wayfinding in a community sample of persons with dementia. Dement Geriatr Cogn Disord. 2004; 17:231–239.

41. Cho MJ, Bae JN, Suh GH, Hahm BJ, Kim JK, Lee DW, et al. Validation of Geriatric Depression Scale, Korean version (GDS) in the assessment of DSM-III-R major depression. J Korean Neuropsychiatr Assoc. 1999; 38:48–63.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download