Abstract
Background
Paget's disease of bone leads to change in the shape and size of the bone and results in reduced bone strength, leading to the complications of deformity, arthritis, and fracture. Due to unknown reasons, Paget's disease is rare in Asian descendants. We report the cases of Paget's disease who visited our institute for 15 years and reviewed the literatures.
Methods
We retrospectively reviewed the medical records and radiograms of 8 patients (6 female and 2 male) who were diagnosed as Paget's disease of bone. Diagnosis was confirmed by typical radiological feature in the involved skeletons and/or pathologic findings.
Results
Pelvis, skull and spine were three most frequently involved bones. All involved bones in our cases showed changes in shape and trabecular pattern which resulted in bowing of lower extremity, secondary osteoarthritis, compression fracture of spine and enlargement of skull. Mean follow time was 4.71 years and all patient were treated bisphosphonate (BP). Use of BP controlled the level of serum alkaline phosphatase level effectively.
Conclusions
We have reviewed eight patients who were previously diagnosed as Paget's disease of bone in our institute. We could identify typical radiologic and clinical findings such as bowing deformity of long bone, secondary osteoarthritis, compression fracture and osteomyelitis of mandible that deteriorated the quality of their living.
Paget's disease of bone is a progressive disorder characterized by an increased rate of bone turnover and remodeling leading to excessive bone resorption and disorganized bone formation. It is also called as osteitis deformans because it leads to change in the shape and size of the bone.[1234] It often involves the axial skeleton such as skull, spine and pelvis. Bowing deformities occur frequently in the long bones of the extremities, especially in the femur and tibia due to its shape and weight bearing. Due to unknown reasons, Paget's disease is rare in Asian descendants. Only one case series with short term follow up was published in Korea. We reviewed the cases of Paget's disease who visited our institute for 15 years and reviewed their skeletal manifestation and follow up records focused on the effect of bisphosphonate.
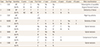
We retrospectively reviewed the medical records and radiograms of 8 patients (6 female and 2 male) who were diagnosed as Paget's disease of bone in our institute since 2001. Seven of them were Korean and one was Russian. They were all middle aged patients and their mean age was 55.4 years (range, 39–67). Diagnosis was confirmed by typical radiological feature in the involved skeletons and/or pathologic findings. Alkaline phosphatase level was elevated in half of the patients. They were all treated with various bisphosphonates. The characteristics of these patients are summarized in Table 1. We made a follow up sheath and checked the effect of bisphosphonate on serum level of alkaline phosphatase in these patients in Table 2.
Diploic widening was noted on the lateral radiograms. One patient was suffered from osteomyelitis of mandible and maxillary bone as well. Pathognomonic finding such as cotton wool appearance' was confirmed in computed tomography (CT) scan (Fig. 1).
Deformity and compression fracture of the involved vertebrae were identified in the CT and magnetic resonance imaging. They were all confirmed by bone biopsy (Fig. 2).
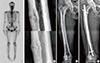
Pelvis and lower extremity; Three patients had lesions in pelvis, three in femur and two in tibia. They all showed thickening of trabeculae. Bowing deformity and/or multiple looser zone were found in the femur and tibia. One Russian patient had severe osteoarthritis of the hip joint which was treated by total joint replacement (Fig. 3).
Mean follow up time was 4.71 years (range, 2–10). All patients took bisphosphonate (BP) for average 2.75 years (range, 1–7). The elevation of serum alkaline phosphatase level was well under control with intake of BP in all cases (Table 2).
A 66 year-old female patient who suffered from an unhealing wound and pus discharge after tooth extraction since 2013 had undergone several debridement surgeries and was diagnosed as Paget's disease of mandible with osteomyelitis. The bony lesions were also confirmed in skull (Fig. 1B, C), pelvis, both femora and tibiae (Fig. 4). Both medial and lateral cortices of the femur were thickened and multiple looser zones were observed in the simple radiogram and technecium 99m whole body bone scan. Slight external expansion of lateral cortex was recognized in the middle one third of right femoral shaft. She was prescribed risedronate due to migratory pain in both lower limbs from 2015. After 1 year of taking risedronate, right thigh pain developed again and did not subside for 3 months.[56] She stopped taking risedronate and visited our clinic for the evaluation of thigh pain and further treatment.
She was afebrile but still had a draining sinus at the inferior aspect of chin due to mandible osteomyelitis. The alkaline phosphatase level had been within normal range consistently for 2-year. Bone specific alkaline phosphatase level (26.8 U/L) was not elevated. Levels of calcium, albumin, 25-hydroxy-vitamin D were normal. White blood cell count, procollagen type I N-terminal propeptide (C1NP) and N-terminal telopeptide (NTx) were within normal range.
Both femora showed thickening and prominence of primary compression and tension trabeculae in the proximal femur. Coxa vara and grade II anterolateral femoral bowing was noted.[7] A beak like protrusion replaced smooth external expansion of the lateral cortex in the femur which was recognized three years ago. Looser zone which was initially noted in the middle of expansion became more distinct and looked like a dreaded black line at the moment.[8] In order to control the thigh pain and prevent impending complete fracture of AFF like lesion, we decided to perform prophylactic femoral nailing using new nailing technique. Nailing procedure was uneventful and nail was inserted in external rotation to accommodate anterolateral femoral bowing.[7] Careful follow up of left femur is also necessary.
In Paget's disease of bone, over-activity of both osteoblasts and osteoclasts, results in either the deposition of low-quality woven bone or areas of osteolysis, respectively. [123] Both can result in reduced bone strength, leading to the complications such as deformity, secondary osteoarthritis, and fracture. Both genetic and environmental factors have been implicated in the pathogenesis of Paget's disease. Paget's disease occurs commonly in families and can be transmitted vertically in an autosomal dominant pattern. Viral infection theory is also advocated by many authors.[2] Several single case reports and one case analysis for 11 patients were reported for Korean patients who were diagnosed as Paget's disease of bone.[4] That suggests rarity of this disease entity in Korea compared to Western countries where Paget's disease is the second most common bone disease after osteoporosis. Pelvis, skull and spine were three most frequently involved bones in their case analysis report. Our cases also showed similar pattern in bone involvement. All involved bones in our cases showed changes in shape and trabecular pattern which resulted in bowing of lower extremity, secondary osteoarthritis, compression fracture of spine and enlargement of skull. Osteomyelitis of mandible and loss of all teeth caused severe decrease in mastication and oral hygiene.
Follow up data (Table 2) showed that the levels of serum alkaline phosphatase were elevated in 4 patients and they were well controlled by various agents of bisphosphonate. The doctors prescribed the bisphosphonate regardless of serum levels of alkaline phosphatase level when patients complain of bone pain in short terms. However, in the case illustration, bisphosphonate was inappropriate to treat this patient due to osteomyelitis of the mandible and atypical features of the femoral insufficiency fracture.[891011] Paget's disease involves both femora and tibiae causing multiple pseudo-fractures (looser zone) in both femora. Chronic insufficiency type fracture in the deformed femur sometimes manifests beak like protrusion in the lateral cortex and a central black line suggesting incomplete AFF. Femoral bowing is one of the causes of atypical femoral diaphyseal fracture as well as long-term use of bisphosphonate.[12] Since she took risedronate for just 1year, it is difficult to estimate the effect of bisphosphonate in this case. The task force team report of the American Society of Bone and Mineral Research excluded the metabolic bone disease such as hyperparathyroidism and Paget's disease in the definition of AFF. It is probably due to difficulty in differentiating the healing callus over the looser zone from periosteal callus reaction in AFF.[13] Aside from the definition of AFF, our patient had the sclerotic bone at the fracture end as well as thigh pain, those were favourable signs of AFF. So, we decided to treat her as if her diagnosis was Paget's disease and AFF.
AFF is difficult to treat once it is completely fractured resulting in high risk of fixation failure and reoperation.[1415] It is beneficial if prophylactic nail is indicated in such patients because clinical results are better. In the surgical treatment of AFF, it is recommended to cover the whole length of femoral shaft so as not to make a stress riser. Severe femoral bowing is contraindicated for prophylactic femoral nailing unless correctional osteotomy is performed. Her femoral bowing deformity was grade II (Fig. 4) and Zimmer natural nail greater trochanter starting femoral nail was inserted using new technique which was developed to accommodate the pre-existing anterolateral femoral bowing with success.[7]
Parathyroid hormone is suggested to be beneficial in the treatment of incomplete AFF. However, it is contraindicated in Paget's disease. And bisphosphonate was inappropriate to treat this patient due to osteomyelitis of the mandible and atypical features of the femoral insufficiency fracture.[9101112131415] Use of denosumab in Paget's disease was not established yet.[16] Since risk of medication-related osteonecrosis of the jaw (MRONJ) was reported in the patients who were treated with denosumab for 10 years. It is not a good choice either. Calcitonin is another option in Paget's disease. However, its use in Paget's disease is still controversial due an increased risk of malignancies in calcitonin-salmon treated patients compared to placebo-treated patients.[1718] Because of limitation in medication, prophylactic nailing in impending AFF in right femur was indicated and performed for her.
Limitations of this study are; First, the patient size was small due to rarity of diseases in Korean ethnics. Second, disease activity was evaluated with serum alkaline phosphatase alone. Third, differentiation of looser zone and transverse fracture was not conclusive. Even though there were few limitations in this study, we could describe the various skeletal manifestations of Paget's disease in Korean patients and effectiveness of bisphosphonate.
Here, we have reviewed eight patients who were previously diagnosed as Paget's disease of bone in our institute. Because of paucity of the cases, only limited analysis was possible. However, we could identify typical radiologic and clinical findings in our cases such as bowing deformity of long bone and subsequent osteoarthritis, compression fracture and osteomyelitis of mandible. Use of bisphosphonate controlled the level of serum alkaline phosphatase level effectively.
Figures and Tables
Fig. 1
(A) General diploic widening and area of lytic defect (osteoporosis circumscripta) is shown in the occipital bone. (B, C) Increased bone density in mandible/maxilla and loss of alveolar bone are shown. The arrow indicates so called ‘cotton wool’ appearance, a pathognomonic finding of Paget's disease.
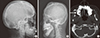
Fig. 2
(A) Multilevel spine involvement with compression fracture and enlargement of spinous processes and laminae is shown. (B) Increased bone formation and bone resorption activity is shown in three lumbar vertebrae with degeneration of intervertebral disc. (C) Suspicious bony lesion in the 3rd lumbar vertebrae was diagnosed as Paget's disease by computed tomography guided spinal bone biopsy. (A, D) Patient's bone biopsy of thoracic vertebrae: irregularly thickened bony trabeculae with osteoblastic and osteoclastic activity are shown (hematoxylin and eosin stain [H & E], ×100 magnification).

Fig. 3
(A) Coronal reconstructed computed tomography scan of the pelvis shows severe osteoarthritis of hip joint: loss of joint space and multiple subchondral bone cyst. Paget's disease involved right innominate bone. (B) Prominent varus deformity and thickened trabecular pattern are shown in the distal metaphysis and both condyles of right femur. (C, D) Thickening of anterior cortex resembling saber shin and varus deformity at the periarticular area are identified in the tibia.
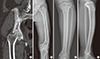
Fig. 4
(A) Whole body bone scan shows hot uptakes in mandible, maxilla, calvarium, pelvis, both femora, and tibiae. Multiple small hot spots in both femoral shafts indicate multiple looser zones. (B) Enlarged views of the mid shaft of right femur (upper part 2013, lower part 2016). (C) Coxa vara and grade II anterolateral femoral bowing (reference line drawn from the tip of the greater trochanter to the center of trochlear notch passes through the medial cortex at the apex of bowing deformity) is shown. A beak like protrusion replaced smooth external expansion of the lateral cortex in the femur (encircled part is enlarged and shown in the lower part of column B). (D) Prophylactic femoral nailing was performed using a new technique which was developed for nailing in atypical femoral fracture associated femoral bowing.
ACKNOWLEDGEMENT
We appreciate professor Hak-Sun Kim, Kyung-Soo Suk, Woo-Suk Lee and Kyung-Hyun Kim who let us analyse their patients for this report.
References
1. Webb NR, Jesse MK. Hip pain. Bisphosphonate-related atypical subtrochanteric femoral fracture in patient with Paget disease. Skeletal Radiol. 2016; 45:825–826. 853–854.
2. Rosen CJ, Compston JE, Lian JB, editors. Primer on the metabolic bone diseases and disorders of mineral metabolism. 7th ed. Washington, DC: American Society for Bone and Mineral Research;2008.
4. Chung YG, Kang YK, Rhee SK, et al. Skeletal manifestation of Paget's disease in Korean. J Korean Orthop Assoc. 2002; 37:649–653.

5. Bhargava P, Maki JH. Images in clinical medicine. “Cotton wool” appearance of Paget's disease. N Engl J Med. 2010; 363:e9.
6. Khosla S, Burr D, Cauley J, et al. Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2007; 22:1479–1491.

7. Park YC, Song HK, Zheng XL, et al. Intramedullary nailing for atypical femoral fracture with excessive anterolateral bowing. J Bone Joint Surg Am. 2017; 99:726–735.

8. Koh JS, Goh SK, Png MA, et al. Femoral cortical stress lesions in long-term bisphosphonate therapy: a herald of impending fracture? J Orthop Trauma. 2010; 24:75–81.

9. Tan A, Goodman K, Walker A, et al. Long-term randomized trial of intensive versus symptomatic management in Paget's disease of bone: The PRISM-EZ study. J Bone Miner Res. 2017; DOI: 10.1002/jbmr.3066.

10. Yang KH, Min BW, Ha YC. Atypical femoral fracture: 2015 position statement of the Korean society for bone and mineral research. J Bone Metab. 2015; 22:87–91.

11. Won Y, Lim JR, Kim YH, et al. Atypical femoral fracture combined with osteonecrosis of jaw during osteoporosis treatment with bisphosphonate. J Bone Metab. 2014; 21:155–159.

12. Oh Y, Wakabayashi Y, Kurosa Y, et al. Stress fracture of the bowed femoral shaft is another cause of atypical femoral fracture in elderly Japanese: a case series. J Orthop Sci. 2014; 19:579–586.

13. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014; 29:1–23.

14. Cho JW, Oh CW, Leung F, et al. Healing of atypical subtrochanteric femur fractures after cephalomedullary nailing: which factors predict union? J Orthop Trauma. 2017; 31:138–145.

15. Lim HS, Kim CK, Park YS, et al. Factors associated with increased healing time in complete femoral fractures after long-term bisphosphonate therapy. J Bone Joint Surg Am. 2016; 98:1978–1987.

16. Reid IR, Sharma S, Kalluru R, et al. Treatment of Paget's disease of bone with denosumab: case report and literature review. Calcif Tissue Int. 2016; 99:322–325.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download